Research Article - Journal of Physical Therapy and Sports Medicine (2022) Volume 6, Issue 4
The effect of cryotherapy vs dynamic compression on pain and range of motion in acute low back pain patients following short-term Physical Therapy?
Jena Etnoyer-Slaski1, Jay Greenstein2, Robert Topp3*1Director of Kaizo Clinical Research Institute, Kaizenovate 827E Rockville Pike, United States
2CEO of Kaizo Health, Kaizo Clinical Research Institute, Kaizenovate 827E Rockville Pike, United States
3Professor, College of Nursing, University of Toledo 3000 Arlington Ave, Toledo, United States
- *Corresponding Author:
- Robert Topp
Professor, College of Nursing
University of Toledo, 3000 Arlington Ave Toledo
Tel: (419) 383-5852
E-mail: Robert.Topp@UToledo.Edu
Received: 26-May-2022, Manuscript No. AAJPTSM-22-65079; Editor assigned: 31-May-2022, PreQC No. AAJPTSM -22-65079(PQ); Reviewed: 14-June-2022, QC No AAJPTSM-22-65079; Revised: 16-June-2022, Manuscript No. AAJPTSM-22-62101(R); Published: 21-June-2022, DOI:10.35841/aajptsm-6.4.116
Citation: Etnoyer-Slaski J, Greenstein J, Topp R. The effect of cryotherapy vs dynamic compression on pain and range of motion in acute low back pain patients following short-term Physical Therapy? J Phys Ther Sports Med. 2022;6(4):116
Abstract
Background: Low Back Pain (LBP) is a common and persistent health problem with increasing prevalence. Treatment for this condition commonly includes physiotherapy with the complimentary therapies of cryotherapy or massage. External Pneumatic Compression (EPC) devices have been developed to administer massage-like therapy. Both cryotherapy and massage have been demonstrated to reduce pain and may improve joint range of motion. Purpose: The purpose of this study was to compare pain and back Range of Motion (ROM) measures among patients with LBP who received either cryotherapy or EPC immediately following three sessions of physiotherapy. Methods: A randomized 2-group pretest-posttest study design examined LBP patients who received either cryotherapy (n=20) or EPC (n=16) immediately following their first three weekly sessions of physiotherapy. Back pain and four measures of back ROM were measured prior to beginning physiotherapy and immediately following the third session of physiotherapy. Immediately following each supervised physiotherapy sessions all participants participated in either cryotherapy or EPC. The cryotherapy group had a cryotherapy pack placed on their low back for 20 minutes. EPC group members were placed in an EPC hip attachment which fit over their lower back, pelvis, and thighs bilaterally. This device produced intermittent compression massage of the quads, hamstrings, IT bands, glutes, and lower back for 20 minutes. Results: Most of the participants in the cryotherapy (75%) and the EPC (80%) groups reported declines in pain beyond the minimal clinically important difference although only the cryotherapy group exhibited a statistically significant decline (p=.01) in their back pain. The cryotherapy group did not change ROM while the EPC group improved (p<0.05) all four of the back ROM measures over the duration of the study. Conclusion: Both cryotherapy and EPC following physiotherapy sessions can produce clinically important reductions in pain while only EPC resulted in improvements in back ROM.
Keywords
Vertebrates, Cryotherapy, Massage, Low back pain, Range of motion, Physiotherapy.
Introduction
Low Back Pain (LBP) is a significant health problem affecting 50–80% of adults at some point in their life with the prevalence and incidence of LBP being reported to be as high as 20.0% and 7.0%, respectively [1]. The etiology of this condition is commonly unknown and presents as persistent pain in the lower back [2]. LBP is broadly classified as chronic or acute, with chronic LBP persisting for greater than 12 weeks and acute pain being less than 12 weeks in duration [3]. Treating LBP is challenging as evidenced by the wide variety or treatments available and the increasing incidence of LBP in the US and worldwide [4]. The American College of Physicians (ACP) has developed clinical guidelines for treating LBP [5] including exercise, stretching, multidisciplinary rehabilitation, acupuncture, and mindfulness-based stress reduction. In addition, cryotherapy, cold therapy or the application of ice is widely used in physiotherapy clinics during and following therapy sessions in order to reduce pain and/or increases in joint range of motion (ROM). This treatment is used because it is simple to apply, low cost, promotes local analgesia6 and inhibits inflammation [6,7]. Cryotherapy is hypothesized to achieve the analgesic effect by reducing nociceptive nerve conduction which increases the pain threshold [6]. Cryotherapy may also involve the release of endogenous opioids further reducing pain perception [8]. In an early study, investigators concluded that cryotherapy accompanied with a pharmacologic treatment could relieve pain to a greater degree than pharmacologic treatment alone among the patients with acute low back pain [9]. This initial beneficial effect of cryotherapy on LBP was not supported by a review that concluded insufficient evidence to evaluate the effects of cryotherapy for treating LBP [10]. A more recent study indicated repeated applications of whole body cryotherapy reduced pain, disability and inflammation markers among patients with chronic LBP [11]. A review by Kalli & Fousekis [12] concluded that there is “no strong evidence” to indicate that cryotherapy can influence joint strength or neuromuscular control but does improve joint range of motion among athletes. Thus, the literature is equivocal on the effect of cryotherapy to reduce pain and improve joint ROM among patients with LBP and indicates the need for additional study.
Massage has also been used to treat LBP. Massage, is defined as a patterned and purposeful manipulation of soft-tissue for therapeutic purposes [13]. A recent scoping review concluded that massage therapy is a preferred technique in chronic musculoskeletal pain management [14]. In a recent review of the literature, [15]. Also reported that a variety of different types of massage therapies can decrease pain and improve functioning among chronic LBP patients. These findings are consistent with previous investigators who reported structural (e.g., deep tissue) and relaxing (e.g., Swedish, hot stone) massage therapy techniques had a similar, beneficial effect on reliving pain, enhancing functioning, and increasing ROM among patient with chronic LBP [16-19].
Recently External Pneumatic Compression (EPC) devices have been developed to administer massage-like therapy. EPC devices provide compression to the limbs via inflatable cuffs which, typically, inflate sequentially from distal to proximal [20]. The sequential nature of inflating, holding, and deflating cuffs is believed to return blood and lymph, and thereby facilitate the transport of wastes and metabolites, from the periphery to the core [21,22]. The efficacy of EPC has been studied as a technique to facilitate recovery following muscle damage [23]. Hoffman [24] reported similar reductions in muscle pain and fatigue following a single post-race treatment intervention of either massage or EPC after a 161-km ultramarathon. A study comparing 20-minute interventions of EPC over five days following completing a muscle damage protocol indicated this therapy reduced delayed onset muscle soreness (DOMS) compared to continuous compression over the five days [20]. A recently completed critical appraisal of studies in this area [25] concluded that EPC devices provide immediate pain relief similar to massage from prolonged exercise-induced DOMS. These authors concluded that an immediate effect of a single treatment does not provide extended pain relief or functional recovery from exerciseinduced muscle damage [25]. Engaging in physiotherapy to treat LBP, although not as intense as completing an endurance event or a muscle damage protocol, may also result in minor muscle damage contributing to pain and reduced joint mobility immediately following the therapy session. To date no study has compared the pain and back range of motion of LBP who receive cryotherapy or EPC following a session of physiotherapy.
The purpose of this study was to compare pain and back ROM measures among patients with LBP who receive either cryotherapy or EPC immediately following three sessions of physiotherapy. This purpose will be addressed by the following protocol guided by two hypotheses:
H1: LBP patients who receive EPC immediately following their first three sessions of physiotherapy will report different levels of pain compared to LBP patients who receive cryotherapy immediately following their first three sessions of physiotherapy.
H2: LBP patients who receive EPC immediately following their first three sessions of physiotherapy will exhibit different changes in back ROM compared to LBP patients who receive cryotherapy immediately following their first three sessions of physiotherapy.
Methods
Design
A randomized two-group pretest-posttest study design was employed to address the study hypotheses. A convenience sample of 40 new patients with acute LBP during their initial visit to a community-based physiotherapy clinic for treatment of their LBP were recruited for participation in the study. At the initial visit, a health care provider validated their diagnosis of LBP as persistent pain in the lower back not lasting more than 12 weeks, of greater than 3 on a 10-point pain intensity scale over the past week, with and without radiating pain to the legs, without clinical features of serious spinal pathology (eg, cauda equina syndrome, infection, fracture, or cancer). Individuals were excluded from the study if they had a history of back surgery, severe mental illness (e.g. schizophrenia) or were physically unable to complete any of the data collection protocols. Following this assessment for inclusion and exclusion criteria to the study then offered the patient a flier explaining the study. Patients who expressed an interest in participating in the study were then approached by a member of the research staff who answered their questions and obtained written consent (Blinded Name of IRB) to participate in the study. A randomized blocking technique was used to initially assign the same number of patients to the two study groups. After providing consent, each subject selected 1 of 40 envelopes; inside of each envelope was a card that indicated their treatment group assignment as either EPC or cryotherapy. Following the group assignment, baseline data were collected, and then each subject engaged in their first session of physiotherapy. Immediately following this first session, and following the next two sessions of physiotherapy, the respective experimental therapy (i.e., cryotherapy or EPC) assigned to each subject was applied by the physical therapist conducting their therapy session. Following completion of their third session of physiotherapy and completion of the experimental intervention each subject again completed the same data collection protocol as they completed at baseline before starting therapy. This methodology resulted in a 2 x 2 pretest-posttest design in which equal numbers of patients were randomly assigned to EPC or cryotherapy groups and evaluated on the outcome variables prior to and following the first three sessions of physiotherapy treating their LBP. All participants who completed the study were given a $25 gift card for participating.
Participants
Patients presenting to a community-based physiotherapy clinic with complaints of acute onset LBP were initially assessed by a provider who confirmed the diagnosis of acute LBP. The diagnosis of acute low back pain was defined as LBP present for up to 12 weeks with the source of the pain originating from spinal joints, discs, vertebrae, or soft tissues of the lower back [3]. Eligible patients also reported the pain in their lower back to be a 3 or greater on a scale of 0 (no pain) to 10 (worst pain imaginable) and reported not consuming any pain medications including muscle relaxants, anti-inflammatory or analgesics during the previous six hours prior to data collection. Patients were excluded from the study if they were younger than 18 years of age, pregnant, had an active cancer diagnosis, a wound or tumor in the area where the EPC or cryotherapy were to be applied, a bone fracture or radiculopathy. Patients were also excluded if they reported signs of acute pulmonary edema, thrombophlebitis, congestive cardiac failure, infection, deep vein thrombosis, episodes of pulmonary embolism, or any signs of poor venous and lymphatic return.
Data collection
Following providing informed consent but prior to engaging in their first weekly session of physiotherapy, all participants completed baseline data collection. This baseline data collection included participants completing a demographic questionnaire where they reported their age, height, weight, age and how many days per week they exercised. After completing the demographic questionnaire participants were asked to rate their current LBP on an 11-point Numeric Pain Rating Scale (NPRS) with 0 indicating no pain, and 10 indicating the worst pain imaginable. The NPRS has been reported to provide a reliable measure of LBP and can predict disability of patients with LBP [26].
Following this assessment of each participant’s LBP the four measures of the participant’s back ROM was assessed including lumbar flexion, right and left trunk side flexion and right hip flexion. All ROM measures were assessed by the same member of the research team using the Easy Angle digital goniometer (Performance Health, Chicago, IL.) following the protocol recommended by the manufacturer. This goniometer has been reported to be a valid and reliable measure of back and neck ROM. Assessment of trunk flexion began with positioning the participant standing with knees straight and physical identification of the posterior superior iliac spine (PSIS) [27]. The goniometer was then positioned on the spine at the level of the PSIS and set to zero. While not allowing the participant to move, the goniometer was then positioned at the L1/T12 level of the spine and the second upright measure was recorded in degrees from the initial zero reading at the PSIS. The participant was then instructed to bend forward as far as possible in the frontal plane, keeping their knees straight, while not deviating to either side, flexing their lumbar spine and holding the position while measurements were recorded.
While the participant held this flexed position, the goniometer was again placed on the spine and the level of the PSIS and zeroed. The goniometer was then placed on the spine at the L1/T12 level of the spine, and the second flexion measure was recorded in degrees. The absolute difference between the second upright measure and the second flexion measure was considered the participant’s lumbar flexion and recorded in degrees. This procedure was repeated three times and the greatest lumbar flexion was recorded in order to determine the participant’s maximum capacity for lumbar flexion and not the average of successive trials.
Assessment of trunk side flexion began with the participant seated upright in a neutral position on a backless stool with the hips flexed between 60-90 degrees in order to stabilize the hip joint. The goniometer was placed on the spine at the level of L1/T12, zeroed and held in place. When assessing right trunk side flexion, the participant was then instructed to lean to the right in the sagittal plane while maintaining their frontal plane as far as they could and to hold this position while the value from the goniometer was recorded. The degrees from zero were considered the participant’s right trunk side flexion. This procedure was repeated three times and the greatest right trunk side flexion was recorded. This measurement procedure was repeated on the left side to record the participant’s left trunk side flexion.
Right hip flexion was assessed by initially positioning the participant supine on an examination table with legs extended in a neutral position. The goniometer was then placed horizontally on the examination table and zeroed. The participant was then instructed to flex their right hip unassisted by bringing their right knee to their chest while bending their knee, keeping their left leg straight on the examination table and not deviating their right leg in the sagittal plane. While maintaining this hip flexed position the goniometer was aligned with the participant’s right femur and the degrees were considered the participant’s right hip flexion. This procedure was repeated three times and the greatest right hip flexion was recorded.
Procedure
All participants were scheduled for three consecutive supervised physiotherapy sessions at a community-based clinic to treat their LBP following the baseline data collection. Each participant had their three physiotherapy sessions supervised by the same therapist and these therapists supervised the therapy of participants in both of the study groups. The first physiotherapy session was completed immediately following baseline data collection. These physiotherapy treatment sessions were approximately and hour in duration and included stretching and rehabilitation exercises. Although these sessions may have been individualized by the attending therapist each of these sessions included a 5-minute sub maximum warm of pedaling a stationary bike, followed by static stretching exercises of the hamstrings, quadriceps, gluteals and lower back. Following the flexibility exercises the participant engaged in strength training exercises of the hamstrings, quadriceps, gluteals and lower back at a duration and intensity chosen by the therapist. Participants then walked at a self-selected speed on a treadmill for 5-mintes as a cooldown. The purpose of the therapy session was twofold, to decrease the hypertonicity of the muscles and to re-strengthen the muscles. On the days when the participant was not scheduled to attend a supervised physiotherapy session, they were instructed to complete standard lower back strengthening and range of motion exercises on their own at home. Over the duration of the study all participants were instructed to maintain their usual activity as tolerated and not to undertake any additional exercise or pain management therapies beyond what was recommended by the therapist managing their care.
Immediately following each of the supervised physiotherapy sessions all participants participated in their respective post therapy intervention which included cryotherapy or EPC. Following their supervised physiotherapy participants assigned to the cryotherapy group were placed in a comfortable prone position and the therapists placed a standard reusable, 6 x 6 inch rectangular cryotherapy pack on top of the participant’s shirt on their low back. A timer was set for 20 minutes and after the time expired the cryotherapy pack was removed and the participant’s therapy session ended.
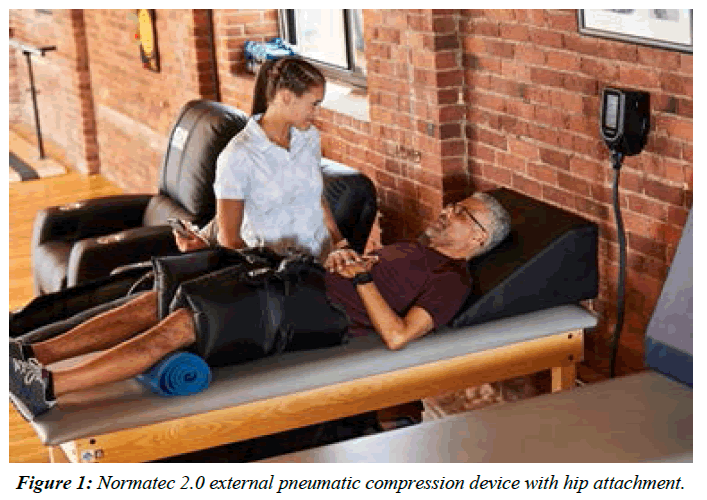
Similarly, immediately following their supervised physiotherapy participants who were assigned to the EPC group utilized the Normatec 2.0 (Hyperice, Irvine, CA USA) with the hip attachment which fit, like a pair of shorts over the lower back, pelvis, and thighs bilaterally (Figure 1). Two overlapping zones created an intermittent compression massage of the quads, hamstrings, IT bands, glutes, and lower back, with two adjustable buckles over the pelvis to ensure a snug and secure fit. Participants in this group were positioned in a supine position with back support. The EPC device was then attached to a computerized air pump that was able to inflate each cell of the device with a different pressure, cyclically inflating and partially deflating. The pump was set to factory defaults of 70 mm Hg peak pressure per cell, 30-second rest, and inflations sequencing from distal to proximal. The pump included a computerized timer and a repeatable pressure sequence. The timer was set for 20 minutes, after the time expired the EPC device was removed and the subject’s therapy session ended.
Analysis
Initial analysis involved comparing the two study groups on demographic measures with continuous variables being compared with an independent t-test and discrete variables being compares using a Chi Square statistic. The study design consisted of measuring each participant’s pain and four measures of back ROM prior to beginning therapy for their LBP and following three separate clinic visits to treat their acute LBP. During each of these first three separate clinic visits participants were given their assigned intervention, cryotherapy or EPC immediately following their therapy session. This design resulted in two groups of participants being measured twice or a 2x2 repeated measures design. Repeated measures ANOVA were performed with time and treatment serving as the independent variables. Significant main effects and/or interaction effects were further analyzed using Tukey post hoc comparisons. G*Power software28 was employed to determine a sample size necessary to detect a 0.35 effect size difference between the two treatment groups over the two data collection points. The assumptions of α=0.05, β=0.20 (statistical power =1-β=0.80) and an r=0.5 as the correlation between measures within an individual justified a sample size of 16 participants per study group.
Results
16 of 20 (80%) participants randomly assigned to the receive the EPC treatment completed the trial and 20 of 20 (100%) participants assigned to receive the cryotherapy completed the trial. Table 1 presents comparisons of the demographic characteristics among the two study groups. No significant differences in demographic characteristics were observed (p>0.05 for all).
| Variable | EPC (n=16) | Cryotherapy (n=20) | Statistical Comparison |
|---|---|---|---|
| Age (yrs) | 37.33 ± 17.46 | 34.90 ± 2.70 | T=0.49, p=0.63 |
| Height (in) | 67.69 ± 4.01 | 66.90 ± 9.63 | T=0.31, p=0.76 |
| Weight (lbs) | 176.2 ± 44.0 | 185.9 ± 41.6 | T=0.68, p=0.50 |
| BMI (kg/m2) | 26.93 ± 6.06 | 31.89 ± 17.97 | T=1.06, p=0.30 |
| Exercise (sessions/week) | 4.00 ± 1.79 | 2.86 ± 2.13 | T=1.73, p=0.09 |
| Sex | M: 11 (69%) F: 5 (31%) |
M: 14 (67%) F: 7 (33%) |
Χ2=0.02, p=0.89 |
BMI - Body Mass Index;
M=Male; F=Female
Table 1. Demographics of the Sample.
Table 2 presents comparisons of pain and the four measures of back ROM measured at the start and the completion of the trial within and between the Cryotherapy and EPC groups.
| Outcome | Start of the Trial | End of the Trial | ||
|---|---|---|---|---|
| Cryotherapy | EPC | Cryotherapy | EPC | |
| Pain (A.U.) | 4.50 ± 0.53 | 5.40 ± 0.60 | 1.30 ± 0.44* | 2.27 ± 0.50 |
| Lumbar Flexion (°) | 58.37 ± 7.26 | 38.47 ±-8.18 | 67.26 ± 8.00 | 55.13 ± 9.00* |
| Hip Flexion (°) | 97.50 ± 6.77 | 90.33 ± 7.82 | 96.70 ± 6.35 | 112.60 ± 7.33* |
| Left trunk side flexion (°) | 24.65 ± 1.91 | 16.67 ± 2.20# | 28.50 ± 2.20 | 22.40 ± 2.54* |
| Right trunk side flexion (°) | 23.80 ± 1.94 | 16.53 ± 2.24# | 27.25 ± 2.17 | 23.13 ± 2.51* |
#, indicates between-groups difference at start of trial (p<0.05);
*indicates within-group difference from start of trial (p<0.05)
Table 2. Pain and back range of motion at start and end of the trial with cryotherapy and external pneumatic compression.
Reported pain at the start of the trial was not different between the groups (p>0.05). Compared to pain values at the start of the trial, there was a statistically significant decrease in pain in the Cryotherapy group (-3.20 ± 2.33 p=0.00). Although the similar reduction in pain observed in the EPC group (-3.13 ± 2.39,) did not reach statistical significance (p>0.05). Lumbar and hip flexion were similar between groups at the start of the trial (p>0.05 for both ROM measures). No significant change in lumbar and hip flexion was observed for the cryotherapy group from the start of the trial (+8.89 ± 19.90°, p>0.05 and -0.80 ± 14.24°, p>0.05 for lumbar and hip flexion, respectively). In the EPC group, both lumbar (+16.66 ± 17.55°, p=0.00) and hip flexion (+22.27 ± 15.56°, p=0.00) were significantly increased at the end of the trial compared to the start of the trial. At the start of the trial the Cryotherapy group presented with significantly greater left (24.65± 1.91 vs 16.67± 2.20, p<0.00) and right trunk side flexion (23.80 ± 1.94 vs 16.53 ± 2.24, p<0.00) compared to the EPC group. Over the duration of the trial the EPC demonstrated a significant increase in their left (+5.73 ± 8.74°, p=0.01 value) and right side trunk flexion (+6.60 ± 8.53°, p=0.02) While the Cryotherapy group did not change their left (+3.85 ± 13.83°, p=0.23) or right side flexion (+3.45 ± 10.10°, p=0.14 for left and right trunk side flexion, respectively). There were no differences between the groups in left and right side flexion at the end of the trial (p>0.05).
Discussion
This study is one of the first to evaluate the efficacy of EPC hip attachments with LBP patients. The findings provide partial support for the first study hypotheses. The cryotherapy group reported a statistically significant decline in their pain over the duration of the trail. While the reduction in pain observed in the EPC group although similar, did not achieve statistical significance [28]. This finding is consistent with previous studies that have reported the efficacy of cryotherapy to effectively reduce pain associated with a variety of conditions [29] including LBP [30]. Previous studies have also reported EPC can reduce exercise induced pain [23-25] following a single bout of training [31] among elite athletes. The mean reduction in pain observed in cryotherapy group (3.20 ± 2.33) achieved statistical significance while the reduction in pain observed in the EPC group (-3.13 ± 2.39) did not exceed this statistical threshold. This similar mean reduction in pain observed among the two treatment groups is supported by the similar percentage of individuals who achieved the Minimal Clinically Important Difference (MCID) for pain reduction determined by Farrar et al. [32] of 2-points on an 11-point scale. Approximately 75% of participants in the cryotherapy group and 80% of participants in the EPC group met or exceeded the MCID for reduced pain. This finding appears to indicate that pain relief offered by the “massage action” of the EPC to relieve muscle and joint tension and pain in the treated tissues has a similar clinical efficacy to the “numbing” pain relieving effect of cryotherapy in decreasing nociceptive nerve activity. The lack of the EPC therapy to produce a statistically significant decrease in pain may be due to the heterogeneity of pain being experienced by this group as evidenced by greater standard deviations for pain exhibited by the EPC group. Further research is needed to explore the physiological mechanisms by which the EPC results in pain relief and if these mechanisms are distinct from cryotherapy. If the mechanisms are different, then the potential exists to examine the combined effects of these therapies to reduce pain.
These results support hypothesis two as evidenced by patients with acute LBP who engaged in the EPC intervention exhibiting improvements in all four measures of back ROM while patients with acute LBP who received the cryotherapy did not change in any measure of back ROM over the duration of the study. These findings appear consistent with previous literature which did not conclusively indicate that cryotherapy increases joint ROM. The previous studies that indicated cryotherapy increased joint ROM were among athletes or involved patients with LBP engaging in multiple sessions of whole-body cryotherapy or cryotherapy combined with pharmacologic treatment. In contrast to the cryotherapy group, there appeared to be consistent improvements in back ROM observed among the study participants with LBP who engaged in EPC. This finding was consistent with previous investigators who reported various massage interventions can increase ROM [16-19].
These finding that that the EPC resulted in improved lumbar flexion, hip flexion, left trunk side flexion and right trunk side flexion is also support by a preliminary study in the area indicating that this therapy can increase lower extremity ROM [33] and facilitated joint functioning following various muscle damaging protocols [24-26]. EPC has also been reported to positively affect joint ROM and skeletal muscle oxidative stress during recovery from exercise [34-36]. It is plausible that the physiotherapy sessions may have resulted in microtrauma of the tissues of the lower back and pelvis and that EPC immediately following these therapy sessions mitigated stiffness and/or pain through facilitating the mobilization of wastes and extra cellar fluid removal from the treated tissues [21].
The present study is not without limitations. First, the protocol did not include a “control condition” consisting of only the physiotherapy without a post therapy intervention. Thus, changes in pain and/or ROM cannot be attributed to the cryotherapy or EPC interventions alone. However, the researchers sought to compare the additional benefit of including different complementary interventions to traditional therapy. The second limitation of the study was the EPC group experienced a 20% dropout. While noteworthy, this is like what has been considered a priori and observed post hoc in other acute LBP studies [37,38]. While no explanation for dropouts among the EPC group was documented, it is unlikely due to lack of benefit given the results observed. Finally, the study protocol did not document the participant’s compliance with the standard lower back strengthening and ROM exercises prescribed to be completed on their own at home. This compliance with therapy prescribed to be completed at home may have had a direct or combined effect with the two interventions tested in this trial. Notably, compliance with the adjunct therapies (i.e., cryotherapy, EPC) was 100% given that they were performed in the clinic under the supervision of study personnel. Future studies examining the efficacy of EPC and cryotherapy following sessions may include a true control and/or sham condition, document compliance with prescribed at home therapy as well as an assessment of patient perceptions of comfort/tolerance and effectiveness.
Conclusion
Both 20 minutes of cryotherapy and EPC following the first three sessions of physiotherapy can produce clinically important reductions in pain while only EPC resulted in improvements in back ROM among low back pain patients.
COI Statement
None of the authors or their family member have a COI, in the form of financial interest in the sponsor of this project or in the outcomes of the study.
Sponsor
This study was supported by a grant to by Hyperice, Inc. 525 Technology Drive, Suite 100 Irvine, CA 92618 who manufactures the Normatec 2.0.
References
- Fatoye F, Gebrye T, Odeyemi I. Real-world incidence and prevalence of low back pain using routinely collected data. Rheumatol Int. 2019;39(4):619-26.
- Maher C, Underwood M, Buchbinder R. Non-specific low back pain. The Lancet. 2017;389(10070):736-47.
- Lam OT, Strenger DM, Chan-Fee M, et al. Effectiveness of the McKenzie method of mechanical diagnosis and therapy for treating low back pain: literature review with meta-analysis. J Ortho & Sports physTher. 2018;48(6):476-90.
- Foster NE, Anema JR, Cherkin D, et al. Prevention and treatment of low back pain: evidence, challenges, and promising directions. The Lancet. 2018;391(10137):2368-83.
- Qaseem A, Wilt TJ, McLean RM, et al. Clinical Guidelines Committee of the American College of Physicians*. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann of Internal Med. 2017;166(7):514-30.
- Allen RJ. Physical agents used in the management of chronic pain by physical therapists. Phys Med and Rehabili Clin. 2006;17(2):315-45.
- Deal DN, Tipton J, Rosencrance E, et al. Ice reduces edema: a study of microvascular permeability in rats. JBJS. 2002;84(9):1573-8.
- Lateef F. Post exercise ice water immersion: Is it a form of active recovery?. Journal of Emergencies, Trauma and Shock. 2010;3(3):302.
- Dehghan M, Farahbod F. The efficacy of thermotherapy and cryotherapy on pain relief in patients with acute low back pain, a clinical trial study. J Clin and Diagnostic Res: JCDR. 2014;8(9):LC01.
- French SD, Cameron M, Walker BF, et al. A Cochrane review of superficial heat or cold for low back pain. Spine. 2006;31(9):998-1006.
- Salas-Fraire O, Rivera-Pérez JA, Guevara-Neri NP, et al. Efficacy of whole-body cryotherapy in the treatment of chronic low back pain: Quasi-experimental study. J Orthopaedic Sci. 2021.
- Kalli K, Fousekis K. The effects of cryotherapy on athletes’ muscle strength, flexibility, and neuromuscular control: A systematic review of the literature. J Bodywork and Movement Ther. 2020;24(2):175-88.
- Ooi SL, Smith L, Pak SC. Evidence-informed massage therapy–an Australian practitioner perspective. Complementary Ther in Clin Practice. 2018;31:325-31.
- Elibol N, Cavlak U. Massage therapy in chronic musculoskeletal pain management: a scoping review of the literature. Medicina Sportiva: J Romanian Sports Med Soc. 2019;15(1):3067-73.
- Skelly AC, Chou R, Dettori JR, et al. Noninvasive nonpharmacological treatment for chronic pain: A systematic review.
- Netchanok S, Wendy M, Marie C. The effectiveness of Swedish massage and traditional Thai massage in treating chronic low back pain: a review of the literature. Complementary Ther in ClinPractice. 2012;18(4):227-34.
- Rahmayani, N. The effect of traditional Thai massage on chronic low back pain. Int J Multi-Science 2020;1(06):31-9.
- Laosee O, Sritoomma N, Wamontree P, et al. The effectiveness of traditional Thai massage versus massage with herbal compress among elderly patients with low back pain: A randomised controlled trial. Complementary Ther in Med. 2020;48:102253.
- Boguszewski D, Krupiński M, Białoszewski D. Assessment of the Effect of Swedish Massage and Acupressure in Rehabilitation of Patients with Low Back Pain. Preliminary Report. Ortopedia, Traumatologia, Rehabilitacja. 2017;19(6):513-21.
- Winke M, Williamson S. Comparison of a pneumatic compression device to a compression garment during recovery from DOMS. Int J Exercise Sci. 2018;11(3):375.
- Brock KA, Eberman LE, Laird RH, et al. Sequential pulse compression’s effect on blood flow in the lower-extremity. J Sport Rehabili. 2020;29(1):7-11.
- Martin JS, Martin AM, Mumford PW, et al. Unilateral application of an external pneumatic compression therapy improves skin blood flow and vascular reactivity bilaterally. Peer J. 2018;6:e4878.
- Berry MJ, Bailey SP, Simpkins LS, et al. The effects of elastic tights on the post-exercise response. Canadian journal of sport sciences. Can J Sport Sci. 1990;15(4):244-8.
- Heapy AM, Hoffman MD, Verhagen HH, et al. A randomized controlled trial of manual therapy and pneumatic compression for recovery from prolonged running–An extended study. Res in Sports Med. 2018;26(3):354-64.
- Stedge HL, Armstrong K. The Effects of Intermittent Pneumatic Compression on the Reduction of Exercise-Induced Muscle Damage in Endurance Athletes: A Critically Appraised Topic. J Sport Rehabili. 2021;30(4):668-71.
- Shafshak TS, Elnemr R. The visual analogue scale versus numerical rating scale in measuring pain severity and predicting disability in low back pain. JCR: J Clin Rheumatol . 2021;27(7):282-5.
- Luedtke K, Schoettker-Königer T, Hall T, et al. Concurrent validity and reliability of measuring range of motion during the cervical flexion rotation test with a novel digital goniometer. BMC Musculoskeletal Disorders. 2020;21(1):1-0.
- Verma JP, Verma P. Determining sample size and power in research studies. Springer Singapore; 2020.
- Garcia C, Karri J, Zacharias NA, et al. Use of Cryotherapy for Managing Chronic Pain: An Evidence-Based Narrative. Pain and Therapy. 2021;10(1):81-100.
- Dehghan M, Farahbod F. The efficacy of thermotherapy and cryotherapy on pain relief in patients with acute low back pain, a clinical trial study. J Clin and Diagnostic Res: JCDR. 2014;8(9):LC01.
- Sands WA, McNeal JR, Murray SR, et al. Dynamic compression enhances pressure-to-pain threshold in elite athlete recovery: exploratory study. The J Strength & Conditioning Res. 2015;29(5):1263-72.
- Farrar JT, Young JP, LaMoreaux L, et al. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149-58.
- Sands WA, Murray MB, Murray SR, et al. Peristaltic pulse dynamic compression of the lower extremity enhances flexibility. The J Strength & Conditioning Res. 2014;28(4):1058-64.
- Haun CT, Roberts MD, Romero MA, et al. Does external pneumatic compression treatment between bouts of overreaching resistance training sessions exert differential effects on molecular signaling and performance-related variables compared to passive recovery? An exploratory study. PLoS One. 2017;12(6):e0180429.
- Marcello RT, Fortini L, Greer BK. Intermittent pneumatic compression boot use elevates blood lactate during subsequent exercise. Int J Exercise Sci. 2019;12(2):385.
- Chase JE, Peeler JD, Barr MJ, et al. The impact of a single bout of intermittent pneumatic compression on performance, inflammatory markers, and myoglobin in football athletes. J Trainol. 2020;9(1):33-8.
- Bishop PB, Quon JA, Fisher CG, et al. The Chiropractic Hospital-based Interventions Research Outcomes (CHIRO) study: a randomized controlled trial on the effectiveness of clinical practice guidelines in the medical and chiropractic management of patients with acute mechanical low back pain. The Spine J. 2010;10(12):1055-64.
- Parkin-Smith GF, Norman IJ, Briggs E, et al. A structured protocol of evidence-based conservative care compared with usual care for acute nonspecific low back pain: a randomized clinical trial. Archof Phys Med and Rehabili. 2012;93(1):11-20.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref