Brief Report - Journal of Clinical Pathology and Laboratory Medicine (2023) Volume 5, Issue 2
Study of Hemostatic control in chronic liver disease patient utilising Thromboelastography and clot waveform analysis
Anjali Jose*, Geeta Vidyadharan, Shine Sadasivan, Greeshma C Ravindran, Renjitha Bhaskaran, Anju Gopinath, Bitty Kurian
Department of Pathology, Amrita Institute of medical sciences Kochi, Kerala, India.
- Corresponding Author:
- Anjali Jose
Department of Pathology
Amrita Institute of medical sciences Kochi
Kerala, India.
E-mail: anjalijose48@gmail.com
Received: 01-Mar-2023, Manuscript No. AACPLM-23-87422; Editor assigned: 03-Mar-2023, PreQC No. AACPLM-23-87422(PQ); Reviewed: 17-Mar-2023, QC No. AACPLM-23-87422; Revised: 23-Mar-2023, Manuscript No. AACPLM-23-87422(R); Published: 30-Mar-2023, DOI:10.35841/aacplm-5.2.136
Citation: Jose A, Vidyadharan G, Sadasivan S, et al. Study of hemostatic control in chronic liver disease patients utilizing thromboelastography and clot wave form parameters. J Clin Path Lab Med. 2023;5(2):136
Abstract
Background: The Hemostatic pathways are generally altered in patients with liver dysfunction. Chronic Liver Diseases (CLD) results in reduced synthesis of Pro-coagulant along with anticoagulant factors and is also related to reduce level of platelet number and function. In Rebalanced hemostasis the defects in pro hemostatic contributors are compensated by complex changes in the anti-hemostatic factors. Global Coagulation Assays (GCA) provides a composite picture of clot dynamics. Our intention was to understand significance of GCA and correlation of Thromboelastography and clot waveform parameters among different subsets of CLD patients. Method: Prospective study of 74 patients from gastroenterology department in Amrita institute of medical sciences with diagnosis of CLD subcategorized into CHILD class was enrolled in our study. Blood collected in two blue tubes from each patient. One sample is centrifuged to attain platelet poor plasma further assessed in DT-100 /Tcoag optical analyzer and the parameters min1, min2 and max2 of PT and APTT waveform were recorded. TEG analysis done from citrated whole blood (2nd sample) using kaolin as activator. The software processed graph reflecting the kinetics and strength of clot, with clot lysis and the values R (Reaction time), Kinetics (K), alpha angle, Maximum Amplitude (MA), clot lysis (ly30) and Coagulation Index (CI) were collected. Results: Extrapolation of individual parameters of GCA showed that parameters min 1 and min 2 of APTT waveform, max2 of PT waveform and TEG parameters such as MA and K showed statistically significant difference from CHILD A – CHILD C disease spectrum. Also, significant correlation between the TEG parameters like Maximum Amplitude (MA), angle, Reaction Time with clot wave form parameters such min 1, min2 and max2 of PT and APTT waveform were attained. Conclusion: TEG and CWA provides a better understanding about the clot strength and dynamics which could be exploited to analyses the homeostatic control in different subsets of CLD patients
Keywords
APTT-Activated Partial Thromboplastin Time, Clot wave form, Prothrombin Time-PT, Thromboelastography.
Introduction
The primary and the secondary hemostatic pathway are generally affected in patients with liver dysfunction. Chronic Liver Diseases (CLD) are conditions in which there is reduced synthesis of Procoagulant along with anticoagulant factors and also related to reduced levels of platelet number and function.
These alterations in the hemostasis affect the Prothrombin Time (PT) and Activated Partial Thromboplastin Time (APTT). However, these parameters are now considered as “not so good” predictors of bleeding risk and are also known to show variations in the clinical manifestation among the patients even if their individual values are same.
The common belief of association of liver disease with an increased tendency towards bleeding is evidenced by the Observations such as higher rate of bleeding complications seen in patients suffering from advanced liver disease. It’s also, presumed that most of these patients are “auto- anticoagulated” and therefore being protected against thrombotic disease. However, it has been noted there is an increased frequency of intravascular coagulation in these patients even though reliable supporting data is scarce. Most of the Patients with liver dysfunction have complex alteration in the maintenance of hemostasis. In Rebalanced hemostasis the defects in pro hemostatic contributors are compensated by complex changes in the anti-hemostatic factors, due to such alterations in the hemostasis, one cannot solely rely on individual coagulation factor levels, or on unembellished tests such as the PT or APTT to predict the hemostatic status as they don’t evaluate this potential state of rebalance therefore such tests are more useful for the diagnosticians for monitoring patients with isolated defects in the hemostasis, for example, patients suffering from hemophilia or patients having isolated thrombocytopenia.
Tests which provides a composite picture from the initiation of clot formation to final clot strength which helps in the identification of many coagulation abnormalities, most commonly known as Global Coagulation Assays(GCA) such as Thrombin Generation Test (TGT), viscoelastometrics assays (RTOEM, TEG) and clot wave form analysis can be utilized to evaluate the coagulopathy of the liver disease patients. To date there are only few studies specifically investigating the effects of different subsets of chronic liver disease patients on global coagulation assays such as TEG and clot wave form analysis? Therefore, we plan to examine the correlation between the TEG and clot waveform parameters among different subsets of CLD patients.
Methods
Selection and description of study participants
The research has been approved by the Institutional Review Board
Prospective study of 78 patients attending gastroenterology department in Amrita institute of medical sciences with diagnosis of chronic liver disease were enrolled in our study. The patients were divided according to the modified Child Pugh (C-P) classification.
Technical information
The objectives were- To correlate the clot waveform parameters such as min 1, min2 and max2 with Thromboelastography test parameters such as Reaction time (R value), Kinetics (K value), alpha angle, Maximum Amplitude (MA), Coagulation Index (CI) and lysis 30 in Chronic Liver Disease (CLD) patients, Child Pugh(C-P) classification was taken to know the severity of the patients and the parameters included in this classification included serum bilirubin, albumin, PT (Prothrombin Time), degree of ascites and encephalopathy. A patient with total score of 5-6 was categorized as CHILD A, score of 7-9 was categorized as CHILD B and score of 10-15 was categorized into CHILD C. All the patients were above 18yrs and informed consent was taken from these patients.
Procedure of sample collection and analysis
Patients diagnosed under chronic liver disease were subcategorized into CHILD class. Blood was collected in two blue tubes which is 3.2% sodium citrated blood collection tube from each patient. One of the samples is centrifuged at 1500 rpg for 10 min to attain platelet poor plasma which is then assessed in DT-100 /Tcoag optical analyzer and the parameters min1, min2 and max2 of PT and APTT waveform were collected and recorded. TEG analysis was performed from the citrated whole blood (2nd sample) using kaolin as activator. The software processed graph reflecting the clot kinetics, clot strength and clot lysis and the values R (Reaction time), Kinetics (K), alpha angle, Maximum Amplitude (MA), clot lysis (ly30) and Coagulation Index (CI) were collected and recorded in these patients. The parameters obtained from the CWA analysis (min1, min 2 and max2 of PT and APTT waveform) and the TEG parameters (R, K, MA, Ly30 and CI) was analyzed to understand the trend of these parameters in different CHILD group and to know how both the global coagulation assay correlate with each other and whether any of these parameters can be used to stratify these patients. Patient previous history of bleeding and platelet was also recorded.
Statistical Analysis
Statistical analysis was done using IBM SPSS 20. (SPSS Inc, Chicago, USA). Categorical variables are represented as number and percentage. To test the statistical significance of the linear relationship between the clot waveform parameters Such as min1, min2 and max2 with TEG parameters such as reaction time (R value), kinetics (k value), alpha angle, maximum amplitude, and Coagulation Index (CI) in CLD Patients in various CHILD score, Spearman rank correlation coefficient was used and its significance tested using linear reg t-test. To test the statistical significance of the difference in the median of min1, min2 and max2, Kinetics (k value), and maximum amplitude, among the CHILD class, Kruskal Wallis Test was used followed by Dun Bonferroni multiple comparison test. A p value<0.05 was considered as statistically significant.
Result
Total of 74 patients, which were sub-categorized according to CHILD class. The individual parameters of CWA which include min1 min 2 max2 PT and APTT waveform were analyzed and its was found that min 1, min2 of both PT and APPT and max2 of PT waveform showed a statistically significant difference from CHILD A- CHILD C spectrum and among the TEG parameters MA and K showed a statistically significant difference among the groups Table 1. The correlation between the parameters of TEG and CWA were assessed and it was observed that in CHILD A and CHILD B maximum amplitude was correlated with CWA parameters such as min1 and min2 and max2 of PT and APTT waveform, however in CHILD C this correlation was not observed and it was the parameter Reaction time® in TEG statistically significant correlation with the CWA parameters Table 2.
| Groups | MAX2 | p-value | ||
|---|---|---|---|---|
| n | Mean ± SD | Median (Q1,Q3) | ||
| CHILD A | 41 | 0.00167±0.000626 | 0.00179(0.00140,0.00201) | <0.001 |
| CHILD B | 18 | 0.00112±0.000756 | 0.00098(0.00052,0.00193) | |
| CHILD C | 14 | 0.00049±0.000451 | 0.00034(0.00015,0.00085) | |
Table 1: Shows Comparison of the max 2 in PT waveforms among CHILD Class.
| Groups | MIN1 | p-value | ||
|---|---|---|---|---|
| n | Mean ± SD | Median (Q1-Q3) | ||
| CHILD A | 41 | -0.0634±.0334 | -0.0670(-0.0801,-0.0513) | <0.001 |
| CHILD B | 18 | -0.049 6±0.0237 | -0.0447(-0.0599,-0.0359) | |
| CHILD C | 14 | -0.0249±0.0228 | -0.0152(-0.0346,-0.0095) | |
Table 2: Shows Comparison of the mean min1 in APTT waveforms among CHILD Class.
Discussion
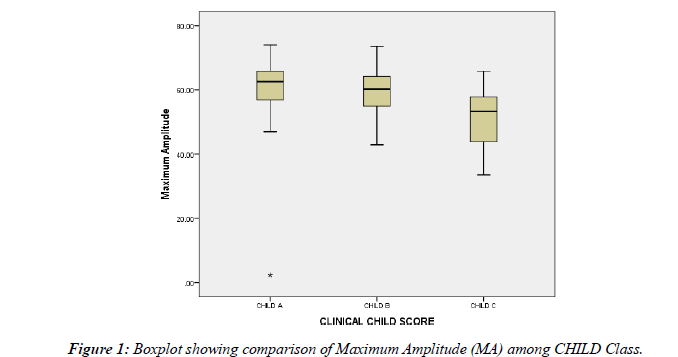
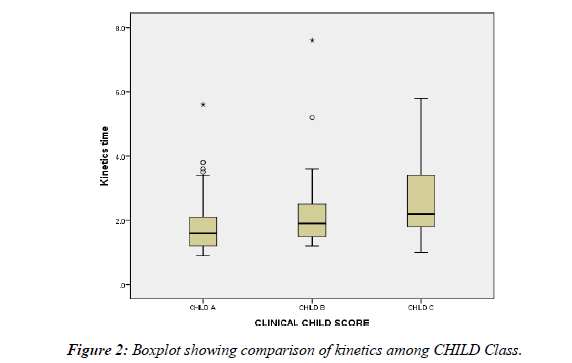
The global coagulation assay provides a better picture about the dynamics of clot formation and lysis as compared to conventional test such as PT and APTT Figure 1. In order to understand the complex hemostasis in CLD patients, the TEG and the clot waveform parameters of chronic liver disease patients were analyzed with respect to Child Pugh clinical categories (CHILD A, CHILD B, and CHILD C) Figure 2. The TEG parameters which were included in our study were defined as:
Reaction time (R min): Time between the initiations of the coagulation cascade to the initial formation of fibrin.
Kinetic time (K min): Time between initial formations of fibrin to 20mm of clot firmness.
Angle (alpha degrees): Rate of fibrin formation and crosslinking.
Maximum amplitude (mm): Maximum clot strength.
Coagulation index: Overall coagulation status-(automatically calculated index from machine by taking into account the parameters R, K, Alpha angle and maximum amplitude) Table-3.
| Groups | Maximum Amplitude | p-value | ||
|---|---|---|---|---|
| n | Mean ± SD | Median (Q1-Q3) | ||
| CHILD A | 41 | 60.5951±11.30467 | 62.50(56.8-65.8) | 0.002 |
| CHILD B | 18 | 59.7889±8.45971 | 60.25(54.9-64.2) | |
| CHILD C | 14 | 50.4846±10.09479 | 53.3.2(43.9-57.8) | |
Table 3: Comparison of the Maximum Amplitude among CHILD Class.
The clot waveform parameters of Prothrombin time and activated partial thromboplastin time included in our study were:
Min 1:Time at which maximum velocity of clot formation was reached.
Min 2: Time at which maximum change in velocity (acceleration) of clot formation was reached.
Max 2: Time at which maximum change in deceleration of clot formation was reached.
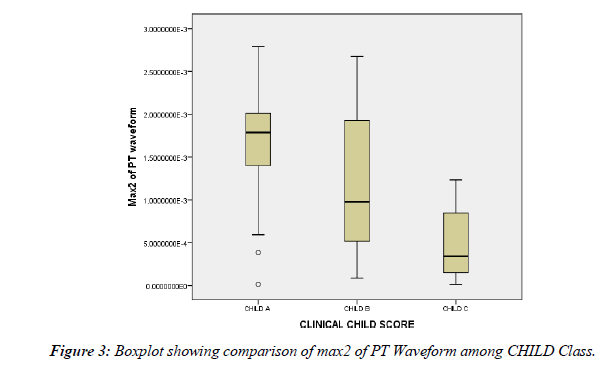
Among the TEG parameters that were assessed it was noticed that the mean Maximum amplitude (clot strength) showed statistically significant difference and showed a decrease in values as we moved through the spectrum from CHILD A–CHILD B - CHILD C. This denotes that the overall clot strength decreased as we progressed from early stage to later stage. In a study conducted by Zhe Zhu et al, it was inferred that MA could be used as sole predictor of mortality in patients with HBV-related acute liver failure and a cut off <51.1mm indicated a poorer prognosis However in the present study a similar cut off could not be established Table-4. A study conducted by comparing with general population, the mean maximum amplitude was found to be within the lower limits in CLD patients with decompensated disease. It was also observed that Kmin (the time between the initial formation of fibrin to specific clot strength) showed statistically significant difference and values increased from CHILD A –CHILD B- CHILD C which denotes that it’s not only the clot strength that is affected, but even the kinetics of the clot to reach a clot strength of 20mm is also affected as the patient progressed from CHILD A -CHILD B- CHILD C. On comparing the TEG parameters of 109 CLD patients with normal reference range it was observed that CLD patients demonstrated reduced MA, prolonged K min and low alpha angles. Coagulation index (calculated index) which depicts the overall coagulation status of the patient was seen to decrease as the patient progressed from CHILDA – CHILD B -CHILD C. Combining these three observations as we moved from CHILD A – CHILD B – CHILD C, the time to reach a particular point of clot strength increased, the overall clot strength decreased and therefore the overall coagulation status of patient decreased as we moved from initial to later stage of disease Figure-3.
| Correlations between max2 and reaction time | CHILD A | CHILD B | CHILD C |
| Coefficient of correlation (r) | -0.155 | -0.113 | -0.855 |
| p-value | 0.334 | 0.665 | <0.001 |
| n | 41 | 17 | 12 |
| Coefficient of Determination (R2) | 02.4% | 01.3% | 73.1% |
Table 4: Correlation between Max2 of PT waveform with reaction time in CHILD Classes.
The parameters in TEG such as alpha angle and Reaction time did not show any statistically significant difference among the CHILD categories. While studying the utility of TEG parameters in cirrhotic patients in a study, it was observed that the alpha angle was depressed in patients with decompensated liver disease and hyperfibrinogenemia. In our study alpha angle reduced from CHILD A-C but was not statistically significant.
The clot wave form parameters which were compared among the different CHILD groups, the observations were:
• Among CHILD A, CHILD B and CHILD C it was found that mean value of max2 decreased as we analyzed from CHILD A – CHILD B-CHILD C.
This denotes that as the clinical severity of the patient increase the clot gets lysed faster. This may be attributed to reduced clot strength which in turn was correlated with maximum amplitude and clotting index.
• Time to attain maximum velocity increased as doe’s acceleration when we analyses from CHILD A- CHILD B – CHILD C. This was also found to be statistically significant.
In favor of our findings, study conducted by MF Ruberto observed that the CWA parameters which included velocity, acceleration was significantly lower in cirrhotic patients with respect to control group.
Further each CWA parameters were then assessed for correlation with TEG values. The observations were as follows
• Clotting process by both the extrinsic and intrinsic pathways showed similar pattern of correlation.
• The individual correlation of the TEG parameters with the clot waveform parameters were assessed among CHILD A, CHILD B and CHILD C and the observations that were made are -
• CHILD A, the MA was negatively correlated with min 1, min 2 of PT waveforms and positively correlated with max2 of the same.
This correlation signifies that as the clot strength reduced the time required for the maximum velocity and acceleration of the clotting process increased further the time required for the deceleration of the clotting process decreased. Similar correlation was obtained between min1 of APTT waveforms and maximum amplitude however no similar findings were obtained between min2 of APTT waveform and MA.
• In CHILD B also Maximum amplitude showed a positive correlation with max2 and showed a negative correlation with min1 and min2 of APTT waveforms which again indicates that as the time required for maximum velocity and acceleration of the clotting process increased the clot strength reduced and as the clot strength increased then the time required for the deceleration of the clotting process also increased. Also, in CHILD B the parameter alpha angle which denotes the rate of clot formation showed a similar correlation with min 1, min2 and max 2 of APTT waveforms. PT waveform parameters were not found to be correlated with maximum amplitude in this category.
• Contrary to CHILD A and CHILD B, only Reaction Time that depicts the time required to initiate a clot process, showed a positive correlation with min1, min2 of PT and APTT waveforms and negative correlation with seen with max2 of PT and APTT waveforms.
Thus, it may be inferred that in CHILD C category, coagulation dysfunction possibly starts at the precoagulant phase itself and therefore a specific correlation between the clot strength MA (Maximum amplitude) and the Clot wave form parameters could not be established.
So, in summary the correlation among the two global coagulation assays in general indicates that among the TEG parameters it’s the maximum amplitude (MA) and K (min) and among the CWA parameters pmax2, min1 and min2 of both PT and APTT waveform could be used as tool to predict the dynamics of the clot formation in various CHILD categories. To the best of our knowledge, till date no study has been done utilizing the correlations between TEG and selected CWA parameters in the assessment of the complex hemostasis in CLD patients The individual correlation between the TEG and the CWA parameters showed that as compared to CHILD groups A and B, where the selected CWA and TEG values were correlated, as we moved from CHILD A- CHILD C this correlation could not be established as went from CHILD B–C, where R time was the most significantly correlated.
Overall, both the global coagulation assay, the CWA and TEG are good tool to assess the hemostasis in the patients and both may be used as tools to monitor the progression of disease in chronic liver disease patients more so when done simultaneously. The role of platelets in providing clot strength was also investigated by analyzing the platelet count with maximum amplitude. In contrast to other findings, it was observed that no statistically significant correlation was attainable between the two. These discrepancies could be explained by the fact that platelet function couldn’t be assessed here which plays a major role. A Study conducted by Nielsen et a l, in rabbit whole blood model also found no significant correlation were found between the platelet count and clot strength. In contrast to our findings, A study was conducted in 90 chronic liver disease patients which were subcategorized into CHILD A, B, C to access the validity of TEG to predict the risk of post procedural bleeding after cannulation in these patients, and it was found that the K time >3.05 predicts bleeding and a maximum amplitude of >48.8mm predicts non bleeding in cirrhotic patients undergoing these procedures. However in our study, eventually the patient’s previous history of bleeding was obtained and it was found that no statistically significant correlation was noted for TEG and clot waveform parameters. In favor of our finding, study conducted by Kyung-Hwa Shin et al showed that the patient’s previous history of bleed or thrombosis was not correlating with any of the TEG parameters.
There we think that this may be due to the small sample size in our study and deficiency in follow up in these patients over a period of time and also other contributions from other parameters such a history of sepsis, or previous history of drug that could interfere with hemostasis in these patients.
Strengths and limitations of our study
Limitations
? A specific reference cut off the parameters studied could not be established with respect to the clinical categories.
? The TEG and CWA parameters were not able to provide information regarding bleeding manifestations in our study.
? Platelet count did not emerge as a significant parameter in our study even though platelet is major player in deciding hemostasis in CLD.
Strengths
? To include a larger series of cases and equal distribution of cases among the different sub categories.
? Establishment of cut off for each category so that the transition from one to next clinical category may be predicted.
Conclusion
As compared to the conventional test such as Prothrombin Time (PT) and APTT (activated partial thromboplastin time) which we routinely use in Chronic liver disease patients in order to assess the hemostatic changes, the global coagulation assay such as TEG and CWA are found to be more effective in providing better understanding of clot kinetics, clot strength and clot lysis in chronic liver diseases patients. This concept was utilized in our study and it was found that the Parameters in TEG such MA (maximum amplitude) decreased and the K increased as the patient progressed from CHILD A–CHILD B–CHILD C. Therefore, in TEG both these parameters may be used as tool to assess the clot kinetics and strength in these patients.
Among the clot waveform parameters max2 decreased and the parameters min 1, min2 of PT and APTT waveform increased as the patient progressed from CHILD A–CHILD B -CHILD C and therefore was found to be most useful parameters. Therefore, by doing a CWA which is easier and cost-effective technique as it’s a readily and easily available test and further combining it with TEG to know more about the dynamics of clot formation and clot strength, it may be utilized in chronic liver disease patients to understand in detail about the complex hemostasis in these patients.
References
- Lisman T, Porte RJ. Rebalanced hemostasis in patients with liver disease: evidence and clinical consequences. Am J Hematol. 2010;116(6):878-85.
- Shin KH, Kim IS, Lee HJ, et al. Thromboelastographic evaluation of coagulation in patients with liver disease. Ann Lab Med. 2017;37(3):204.
- Ruberto MF, Sorbello O, Civolani A, et al. Clot wave analysis and thromboembolic score in liver cirrhosis: two opposing phenomena. Int J Lab Hematol. 2017;39(4):369-74.
- Zhu Z, Yu Y, Ke Y, et al. Thromboelastography maximum amplitude predicts short?term mortality in patients with hepatitis B virus?related acute-on?chronic liver failure. Exp Ther Med. 2020;20(3):2657-64.
- Lloyd-Donald P, Vasudevan A, Angus P, et al. Comparison of thromboelastographic and conventional coagulation tests in patients with severe liver disease. Clin Appl Thromb Hemost. 2020;26.
- Stravitz RT. Potential applications of thromboelastographic in patients with acute and chronic liver disease. Gastroenterology Hepatol. 2012;8(8):513.
- Solomon C, Ranucci M, Hochleitner G, et al. Assessing the methodology for calculating platelet contribution to clot strength (platelet component) in thromboelastometry and thrombelastography. Anesth Analg. 2015;121(4):868.
- Pandey CK, Saluja V, Gaurav K, et al. K time & maximum amplitude of thromboelastogram predict post-central venous cannulation bleeding in patients with cirrhosis: a pilot study. Indian J Med Res. 2017;145(1):84.
- Premkumar M, Mehtani R, Divyaveer S, et al. Clinical validation of global coagulation tests to guide blood component transfusions in cirrhosis and ACLF. J clin transl hepatol. 2021;9(2):210.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref