Research Article - The International Tinnitus Journal (2019) Volume 23, Issue 1
Sleep Disturbances Associated With Tinnitus: Reduce the Maximal Intensity of Tinnitus
Department of Pain therapy, Pain Clinic De Bilt, Groenkanseweg, Netherlands
Send correspondence to:
Selim Unsal, PHD
Department of Pain therapy, Pain Clinic De Bilt, Groenekanseweg 70, 3732AG De Bilt, Netherlands. E-mail: hmkoning@pijnkliniekdebilt.nl Tel: +0031302040753.
Paper submitted to the ITJ-EM (Editorial Manager System) on June 08, 2019; and Accepted on June 24, 2019
Citation: Koning HM. Sleep Disturbances Associated With Tinnitus: Reduce the Maximal Intensity of Tinnitus. Int Tinnitus J. 2019;23(1):64-68.
Abstract
Introduction: The high prevalence together with the serious impact of sleep disturbances assessed in tinnitus patients urge the need for effective therapy that could improve patients' sleep quality.
Objectives: The purpose of this study was to assess the reported prevalence and severity of sleep disturbance in chronic tinnitus patients and to extract possible tinnitus specific factors that increase the risk of developing sleep disturbances.
Design: Subjects were 165 consecutive patients who came to our clinic from January 2017 to January 2019 for consultations on their tinnitus that persisted for one month or longer. Patients charts, audiogram, and sleep questionnaire were reviewed retrospectively and data from these patients were recorded.
Results: Half of the tinnitus patients experienced a poor sleep quality. Cervical pain, the use of benzodiazepines and antidepressants, a higher maximal and a higher mean intensity of tinnitus were associated with a poor sleep quality. Especially, a higher maximal intensity of tinnitus was associated with a poor sleep quality. With a VAS of the maximal intensity of the tinnitus higher than 85 millimeter, 69% of the patients have a poor sleep quality. If the VAS of the maximal intensity of the tinnitus was less than 60 millimeter, none of the patients had a poor sleep quality.
Conclusions: In a cohort of patients with chronic tinnitus, we found that half of the tinnitus patients experienced poor sleep quality. The level of the maximal intensity of tinnitus was associated with the sleep quality. It seems that reduction of the intensity of the tinnitus is essential for improvement of quality and patients' quality of life in patients with tinnitus
Introduction
Difficulty initiating sleep, difficulty maintaining sleep, and a poor perceived quality of sleep are frequently encountered in patients with tinnitus [1]. Tinnitus severity is highly correlated with patients' degree of sleep disturbance and reduction of the intensity of the tinnitus could improve sleep quality and patients' quality of life [2-5]. The high prevalence together with the serious impact of sleep disturbances assessed in tinnitus patients urge the need for effective therapy that could improve patients' sleep quality. The purpose of this study was to assess the reported prevalence and severity of sleep disturbance in chronic tinnitus patients and to find possible tinnitus specific factors that increase the risk of developing sleep disturbances.
Materials and Methods
Subjects: The Medical research Ethics Committees United (Nieuwegein, the Netherlands) approved the present observational study and waived the request for informed consent for the current study. A retrospective chart review was conducted. All patients who visited our clinic between January 2017 and January 2019 for tinnitus that persisted for 1 month or longer were included. There were no exclusion criteria. All patients were previously consulted by an otorhinolaryngologist and all patients who suffered with unilateral tinnitus had anatomical pathology ruled out by MRI. The workup of a patient with tinnitus consisted of a standardized clinical history, a bilateral audiogram, and a standardized questionnaire for the sleep. The standardized clinical history included tinnitus characteristics (left side and/or right side, traumatic cause, duration of complaints, age of onset, and the minimal, maximal and mean intensity of their tinnitus measured by the visual analog scale), medication, and concomitant symptoms (self-reported hearing loss, the presence of dysbalance, dizziness, and cervicalgia). A standardized bilateral clinical audiogram assessed pure tone thresholds at 250, 500, 1000, 2000, 4000, and 8000 Hz. A standardized questionnaire for the sleep included three questions (“Is it hard to fall in sleep?”, “Are you awake at night?”, and “Are you good awake in the morning?”. Each question could be answered with none, slight, moderate, or good.
Data Assessment: Patient charts were reviewed retrospectively to obtain data. Data recorded from these patients are patient characteristics (age, sex), tinnitus characteristics (left side and/or right side, traumatic, duration of complaints, and age of onset, and the minimal, maximal and mean intensity of their tinnitus measured by the visual analog scale), comorbidity (self-reported hearing loss, the presence of dysbalance, dizziness, and cervicalgia), and the results of the sleep questionnaire. Visual Analog Scales (VAS) of tinnitus are 10-cm lines anchored at the left end by “no tinnitus” and at the right end by “unbearable tinnitus”. The patient is asked to place vertical marks on the scale to indicate the level of the mean, minimal and maximal intensity of his or her tinnitus. Using a ruler, the score is determined by measuring the distance (millimetre) on the 10-cm line between the “no tinnitus” anchor and the patient’s mark, providing a range of scores from 0-100. A higher score indicates greater intensity of tinnitus. The three questions of the sleep questionnaire were rated with none (0), slight (1), moderate (2), or good (3). The sleep-score is calculated by totalling the scores of the three questions of the sleep questionnaire, providing an overall score ranging from 0 to 9, where a lower score denotes a healthier sleep quality. A total score of 6 or greater indicates poor sleep quality, and a score lower than 6 is regarded as normal. A standard clinical audiogram assessed pure tone thresholds at six different frequencies from 250 Hz to 8 kHz (250, 500, 1000, 2000, 4000, and 8000 Hz). Each ear was exposed to pure tones ranging from 250 Hz to 8 kHz at increasing intensities until the threshold of detection was reached. The audiogram of the dominant side of the tinnitus was selected for analysis. In cases of bilateral tinnitus with equal intensity, the mean of the results of the audiogram of both sides was used.
Statistical Methods: Statistical analysis was performed with Minitab 16 (Minitab Inc, State College, PA, USA). A χ2 test was used for dichotomous variables, and Student’s t-test was used for continuous variables. Discriminant analysis for division in four groups was used in order to evaluate the correlation of the maximal intensity of tinnitus with the result of each question of the sleep questionnaire. A value of P < 0.05 was considered statistically significant.
Results
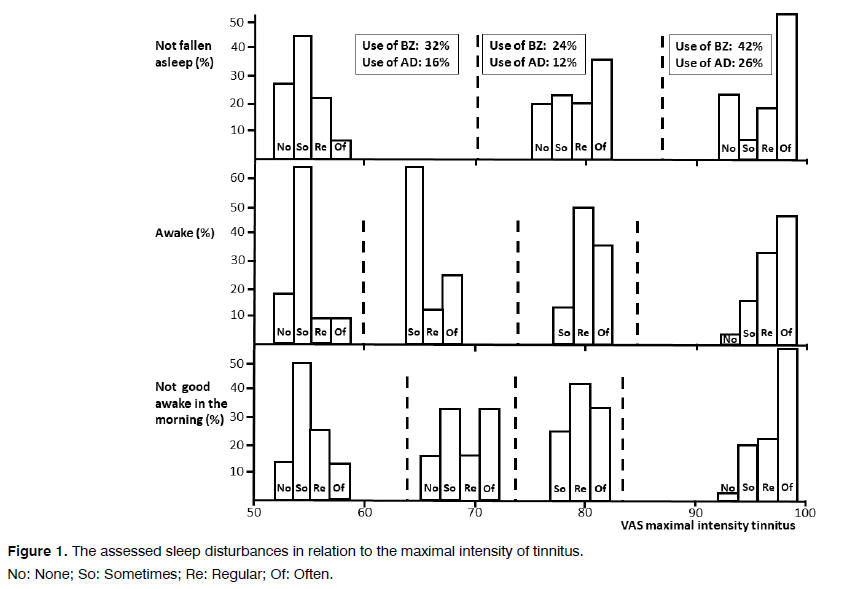
From January 2017 to January 2019, 165 patients came to our clinic in De Bilt for consultations on their tinnitus that persisted for one month or longer. The characteristics of these patients are shown in Table 1. Tinnitus was associated with a hearing loss in the higher frequency (4 KHz to 8 KHz), and with a high prevalence of cervical pain. Half of the tinnitus patients experienced a poor sleep quality. Patients with a poor sleep quality were compared with the patients with normal sleep quality (Table 2). Cervical pain, the use of benzodiazepines and antidepressants, a higher maximal and a higher mean intensity of tinnitus were associated with a poor sleep quality. Especially, a higher maximal intensity of tinnitus was associated with a poor sleep quality. Discriminant analysis for division in four groups was used in order to evaluate the correlation of the maximal intensity of tinnitus with the result of each question of the sleep questionnaire. The level of the maximal intensity of the tinnitus could predict the response on questions “Is it hard to fall in sleep?”(Proportion Correct=0.419), “Are you awake at night?”(Proportion Correct=0.466), and “Are you good awake in the morning?” (Proportion Correct=0.419). The levels of the maximal intensity of the tinnitus which indicated a change between the groups are indicated in Figure 1. If the VAS of the maximal intensity of the tinnitus is higher than 71 millimeter more patients have difficulty fallen asleep, if it exceed 73 millimeter than more patients are awake, and if it exceed 74 millimeter than more patients are not good awake in the morning. A VAS of the maximal intensity of the tinnitus higher than 85 millimeter was associated with serious sleep problems with a high prevalence of not fallen asleep, being awake and not good awake in the morning, despite the use of benzodiazepines and antidepressants. With the use of Figure 1, we defined subclasses of VAS of maximal intensity of tinnitus to indicate the chance of a poor sleep quality (Table 3). With a VAS of the maximal intensity of the tinnitus higher than 85 millimeters, 69% of the patients have a poor sleep quality. If the VAS of the maximal intensity of the tinnitus was less than 60 millimeter, none of the patients had a poor sleep quality.
| Prevalence | Median | Q1 – Q3 |
|---|---|---|
| Age (year) | 57 | 49.0 – 63.5 |
| Gender (male) | 56% | |
| Self-perceived hearing loss | 60% | |
| Cervical pain | 65% | |
| Poor sleep quality | 50% | |
| Sleep-score | 5.5 | 3.0 – 8.3 |
| Period of tinnitus (year) | 6 | 1.9 – 16.0 |
| Intensity of the tinnitus | ||
| Mean | 70 | 50 – 83 |
| Maximal | 85 | 70 – 95 |
| Minimal | 44 | 20 – 66 |
| Hearing loss (dB) at: | ||
| 250 Hz | 15 | 10.0 – 25.0 |
| 500 Hz | 15 | 5.0 – 25.0 |
| 1 KHz | 15 | 8.0 – 30.0 |
| 2 KHz | 20 | 10.0 – 35.0 |
| 4 KHz | 40 | 20.0 – 55.0 |
| 8 KHz | 50 | 25.0 – 65.0 |
Table 1. Clinical characteristics of the patients with tinnitus.
| Age (year) | Poor sleep quality | Normal sleep quality | P-value | ||||
|---|---|---|---|---|---|---|---|
| (sleep-score of 6 of higher) | (sleep-score less than 6) | ||||||
| Prev | Mean | SEM | Prev | Mean | SEM | ||
| Gender (male) | 44% | 57.4 | 1.7 | 54.2 | 2.1 | 0.245 | |
| Self-perceived hearing loss | 58% | 69% | 0.274 | ||||
| Cervical pain | 71% | 49% | 0.031 | ||||
| Use of Benzodiazepines | 42% | 22% | 0.042 | ||||
| Use of Antidepressants | 24% | 9% | 0.048 | ||||
| Use of Antipsychotics | 7% | 0% | 0.078 | ||||
| Period of tinnitus (year) | 8.9 | 1.7 | 11 | 1.5 | 0.357 | ||
| Intensity of the tinnitus (VAS; millimetre) | |||||||
| Mean | 71 | 4.5 | 57 | 3.9 | 0.017 | ||
| Maximal | 88 | 1.9 | 71 | 4.1 | 0 | ||
| Minimal | 51 | 5.3 | 40 | 4.2 | 0.119 | ||
Table 2. Differences in characteristics between patients with and without poor sleep quality.
| Maximal intensity of tinnitus (VAS) | Poor sleep quality | Sleep score |
|---|---|---|
| Prevalence | Mean SEM | |
| Less than 60 millimetre | 0% | 3.0 0.37 |
| 60-73 millimetre | 36% | 4.5 0.81 |
| 74-85 millimetre | 38% | 5.8 0.51 |
| More than 85 millimetre | 69% | 6.7 0.44 |
Table 3. Sleep quality in subclasses of maximal intensity of tinnitus.
Discussion
In a cohort of patients with chronic tinnitus, we found that half of the tinnitus patients experienced poor sleep quality. The level of the maximal intensity of tinnitus was associated with the sleep quality. A VAS of the maximal intensity of the tinnitus higher than 85 millimeter was associated with serious sleep problems, despite the use of benzodiazepines and antidepressants. If the VAS of the maximal intensity of the tinnitus was less than 60 millimeter, none of the patients had a poor sleep quality. The prevalence of sleep disorders in chronic tinnitus patients is reported from 66% to 76% [2-5]. Sleep complaints in tinnitus patients include difficulty in falling asleep, difficulty in maintaining sleep, early morning wakefulness, and non-restorative sleep with daytime sleepiness, and chronic fatigue [1-6]. In mammals, physiological sleep is comprised of two distinct states called rapid-eye movement (REM) sleep and non-REM (NREM) sleep that alternate through the night in a cyclical fashion [7]. NREM sleep is divided into progressively deeper stages, named stage N1, stage N2, and stage N3. Stage N3 seems important for cerebral restoration and recovery, the maintenance and consolidation of memory, and metabolic regulation [8]. Polysomnographic findings in chronic tinnitus patients indicated that patients with tinnitus stayed longer in shallow sleep and spent less time in stage N3 NREM sleep and in REM sleep [9]. The way tinnitus can induce disturbed sleep is not clearly understood. Normal transitions from wakefulness to sleep involve sleep-related inhibition of the multiple arousal systems [10]. The thalamus is involved in the regulation of arousal and sleep, and especially the “nonspecific” thalamic nuclei promote arousal [11]. Tinnitus activates the “nonspecific” auditory thalamic nucleus, the medial geniculate body, and therefore may stimulate the arousal system during sleep [12] However, it seems that this interruption only take place if the maximal intensity of tinnitus exceed a level of 60 millimeter. If the VAS of the maximal intensity of the tinnitus was less than 60 millimeter, none of the patients had a poor sleep quality. A VAS of the maximal intensity of the tinnitus higher than 85 millimeters was associated with serious sleep problems, despite the use of benzodiazepines and antidepressants. This raise the question whether medication intend to improve the sleep in patients with tinnitus are useful in patients with severe tinnitus. Our study indicates that this would not be the case and we advise therapy to lower the maximal intensity of the tinnitus for sleep problems associated with tinnitus. The use of hypnotic drugs, such as benzodiazepines, and of antidepressants, such as tricyclic’s and Selective Serotonin Reuptake Inhibitors (SSRIs) for improvement of sleep problems in patients with severe tinnitus should also be questioned. This study has several limitations. First, the current retrospective study comes with inherent limitations. A prospective follow-up study would be necessary to confirm these results. Second limitation is the use of the reported sleep questionnaire instead of standardized sleep questionnaires. In a prospective follow-up study adding such a questionnaire could give more information for the sleep disorders associated with tinnitus.
Conclusions
In a cohort of patients with chronic tinnitus, we found that half of the tinnitus patients experienced poor sleep quality. The level of the maximal intensity of tinnitus was associated with the sleep quality. A VAS of the maximal intensity of the tinnitus higher than 85 millimeter was associated with serious sleep problems, despite the use of benzodiazepines and antidepressants. If the VAS of the maximal intensity of the tinnitus was less than 60 millimeter, none of the patients had a poor sleep quality. It seems that reduction of the intensity of the tinnitus is essential for improvement of sleep quality and patients' quality of life in patients with tinnitus.
Conflict of Interest
The Author declares no potential conflict of interest on publishing this paper.
References
- Izuhara K, Wada K, Nakamura K, Tamai Y, Tsuji M, Ito Y, et al. Association between tinnitus and sleep disorders in the general Japanese population. Ann Otol Rhinol Laryngol. 2013;122:701-6.
- Wakabayashi S, Saito H, Oishi N, Shinden S, Ogawa K. Effects of tinnitus treatments on sleep disorders in patients with tinnitus. Int J Audiol. 2018;57:110-14.
- Drexler D, López-Paullier M, Rodio S, González M, Geisinger D, Pedemonte M. Impact of reduction of tinnitus intensity on patients quality of life. Int J Audiol. 2016;55:11-19.
- Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol. 2000;21:287-93.
- Schecklmann M, Pregler M, Kreuzer PM, Poeppl TB, Lehner A, CrönleinT, et al. Psychophysiological Associations between Chronic Tinnitus and Sleep: A Cross Validation of Tinnitus and Insomnia Questionnaires. Biomed Res Int. 2015;46-109.
- Attanasio G, Russo FY, Roukos R, Covelli E, Cartocci G, Saponara M. Sleep architecture variation in chronic tinnitus patients. Ear Hear. 2013;34:503-7.
- Weber F, Hoang Do JP, Chung S, Beier KT, Bikov M, Saffari Doost M, et al. Regulation of REM and Non-REM Sleep by Periaqueductal GABAergic Neurons. Nat Commun. 2018;9:354-56.
- Gobbi G, Comai S. Differential function of melatonin MT1 and MT2 Receptors in REM and NREM Sleep. Front Endocrinol (Lausanne). 2019;1:10-87.
- Teixeira LS, Oliveira CAC, Granjeiro RC, Petry C, Travaglia ABL, Bahmad F. Polysomnographic findings in patients with chronic tinnitus. Ann Otol Rhinol Laryngol. 2018;127:953-61.
- Gvilia I. Underlying brain mechanisms that regulate sleep-wakefulness cycles. Int Rev Neurobiol. 2010;93:1-21.
- Honjoh S, Sasai S, Schiereck SS, Nagai H, Tononi G, Cirelli C. Regulation of cortical activity and arousal by the matrix cells of the ventromedial thalamic nucleus. Nat Commun. 2018;29;9:21-100.
- Mazurek B, Stöver T, Haupt H, Klapp BF, Adli M, Gross J, et al. The significance of stress: Its role in the auditory system and the pathogenesis of tinnitus. 2010;58:162-72.