Research Article - Otolaryngology Online Journal (2020) Volume 10, Issue 5
Role of Lymphoscintigraphy and SPECT-CT in Sentinel Lymph Node Detection in Early Stage Squamous Cell Carcinoma of Oral Cavity: Our Experience
Ramya Rathod, Jaimanti Bakshi*, Naresh Kumar Panda, RoshanVerma, Anish Bhattacharya, Amanjit BalPost graduate institute of medical education and research, Chandigarh, India
- *Corresponding Author:
- Jaimanti Bakshi
Post graduate institute of medical education and research
Chandigarh, India
Tel: +919855827931
E-mail: drjayabakshi@ymail.com
Received: July 17, 2020; Accepted: November 16, 2020; Published: November 23, 2020
Abstract
Objective: A multidisciplinary team trial in a tertiary care centre in patients with early stage squamous cell carcinoma of oral cavity to review the established role of advanced imaging modalities like lymphoscintigraphy and SPECT-CT in sentinel lymph node identification and to layout our experience in performing this modality.
Methods: A prospective, case control study of diagnosed cases of T1/T2 N0 squamous cell carcinoma of oral cavity undertaken from December 2016 to January 2018 at our institution of which the patients in study group underwent SLNB guided neck dissection and the patients in control group underwent Elective Neck Dissection. We compared both the groups in terms of the operating time, the post-operative histopathology, the diagnostic accuracy and the outcomes which were statistically analysed. Also we studied and analysed the efficacy of static and dynamic lymphoscintigraphy followed by SPECT-CT in identifying sentinel lymph node areas in neck and intra-operative gamma probe use to precisely locate the sentinel nodes.
Results: Out of 40 patients, 20 each in study and control groups were included. The SLN identification rate was 100% with combined SPECT-CT and gamma probe use whereas it was 70% with imaging alone. The sensitivity, specificity, positive predictive value and negative predictive value of SLNB and END were 80% , 56.58%, 9.61%, 98% and 78.5 %, 73.48% ,10.67% , 98.8 % respectively. The operating time was less in the SLNB group with statistically significant difference between the two groups.
Conclusion: High SLN identification rate with combined use of SPECT-CT and gamma probe and high NPV render SLNB as a reliable modality in the management of early stage oral cavity cancers in a centre with a multidisciplinary team set up and appropriate facilities.
Keywords
Oral cavity, Cell carcinoma, Lymph node
Introduction
Cervical lymph node metastasis is the single most important prognostic factor in squamous cell carcinoma of head and neck which can decrease the 5-year survival rates to <50%. None of the currently available imaging methods reliably depicts small tumor deposits in non-enlarged lymph nodes or differentiate reactively enlarged lymph nodes from metastatic adenopathy. Therefore, management of a clinically N0 neck is performed when the risk of micro metastasis is more than 30% for which either Radiotherapy or Elective neck dissection (END) are practiced [1].
Better modality of managing N0 neck is neck dissection with Elective neck dissection being the gold standard. There is a paradigm shift from extensive to selective neck dissection for oral cavity cancers. But the rate of skip metastases to level IV is approximately 10% for tongue primaries. Thus, the concept of sentinel lymph node biopsy (SLNB) came into practice which mimics physiological migration of cancer cells from the tumor to the lymph nodes with migration of known detectable tracer. Previous studies have made use of a triple diagnostic approach which includes use of peritumoral radiotracer injection followed by lymphoscintigraphy which points towards the area to be explored during neck dissection, an intra operative Gamma probe use which pinpoints the sentinel and non-sentinel lymph nodes and a peritumoral vital dye injection which stains the lymphatic tracts to the sentinel node thus assisting in careful dissection [2].
Tc 99 m is a near ideal pharmaceutical agent with a physical half-life of 6 hours and its principal mode of decay is by a process called Isomeric transition [3]. Gamma camera has a Sodium Iodide (NaI) scintillating crystal which interacts with the gamma rays emitted from the patient and emits thousands of light photons which are collected on an array of photo multiplier tubes (PMT) which gives total radiotracer uptake and its spatial distribution within tissue [4]. SPECT-CT gives better definition to the imaging with localization of the lymph nodes relative to anatomical landmarks and also reduces the obscuring of nodes by activity of an injection site that is near the tumor [5].
Additions of serial step sectioning and immunohistochemistry to the routine histopathological examination of the sentinel lymph nodes have been studied to improve the diagnostic accuracy of the SLNB procedure. In this study, we aimed to study the correlation between the detected sentinel lymph nodes in the study group and their post-operative histopathological reporting to establish its diagnostic accuracy in comparison to elective neck dissection performed in the control group.
Materials and Methods
The study was conducted in the Department of Otolaryngology and Head & Neck Surgery, Post Graduate Institute of Medical Education and Research (PGIMER), Chandigarh, India in collaboration with Department of Nuclear medicine and Department of Pathology. The study duration was one and half years i.e. January 2017 to July 2018. This was prospective, case control study with a total of 40 diagnosed patients of early stage squamous cell carcinoma of oral cavity enrolled into study and control groups. A prior approval of institute ethics committee was obtained. The plan of treatment for the study and control groups was discussed in detail to the patients and their attendants and informed and written consent was taken before proceeding with the study. The minimum follow up period planned for both groups during the study period was 6 months and maximum follow up period was variable.
Inclusion criteria: All diagnosed cases of stage I and II (AJCC TNM 7th edition) oral cavity squamous cell carcinoma between 20 to 80 years of age were included in the study.
Exclusion criteria: Patients with T3 or T4 disease irrespective of nodal status, with node positive neck, with malignancy of multiple subsites of oral cavity, with any other co-existing malignancies, with prior history of treatment of neck by surgery or radiotherapy or chemotherapy and patients who are unfit for surgery due to associated Comorbidities were not considered for the study.
Study group: SLNB guided Neck dissection +Wide local excision of the primary tumor. A four quadrant peritumoral, submucosal, filtered Tc 99 m sulphur colloid radiotracer injection was given an hour prior to taking up the patient for the surgery. The radiotracer was procured from Board of radiation and isotope technology (BRIT), Government of India, Department of Atomic Energy. Early, dynamic and late, static lymphoscintigraphy imaging followed by a SPECT-CT was carried out. We used a Siemens (Germany) SymbiaT-16 Dual head Gamma camera with 16 slice CT scanner for the lymphoscintigraphy and SPECT-CT .We used the EuroRad, Large size, Europrobe model Gamma probe. Once the patient was induced of general anesthesia, Gamma probe was applied to the neck and the neck levels with high radioactivity were marked and documented as preflap counts i.e., before raising the subplatysmal flaps. Gamma probe was applied once the subplatysmal flaps were raised and the radioactivities were documented as post-flap in vivo counts i.e., after raising the subplatysmal flaps but before performing the neck dissection. The neck dissection of the patient was planned according to the sentinel lymph node level obtained and one level below the sentinel lymph node level was included in the neck dissection specimen. In the dissection of level IB, submandibular gland was removed in most of the cases. Exploration of Level IIB and Level V was dependent upon the radioactivity in Level IIA. Once the lymph node and the fibrofatty tissue from one level were dissected, gamma probe was applied to the specimen and radioactivity counts were recorded as post-flap exvivo counts i.e., the radioactivity of the lymph node after their resection. After the planned neck dissection was completed, gamma probe was applied to the bed of the dissected neck levels and checked for any residual radioactivity which was recorded as bed counts. If any radioactivity was detected in the bed, then that level was re-explored for any residual lymph nodes or fibro fatty tissue and was excised. The resected lymph nodes and fibrofatty tissue were labelled separately for each level and sent for the histopathological examination. The sentinel lymph nodes were not revealed to the histopathologist.
Control group: Elective neck dissection + Wide local excision of primary.
The plan of neck dissection in this group was decided intra-operatively based upon the detection of grossly visualised lymph nodes in various neck node levels. One level below the level of grossly visualised lymph node was included in the neck dissection. Exploration of levels IIB and V was dependent upon the presence of lymph nodes in level IIA. The excised lymph nodes and fibro fatty tissue were labelled separately for each level and sent for the histopathological examination.
In both the groups, a 1-1.5cm margin was marked all around the primary tumor and the tumor was excised by utilising a monopolar cautery and a harmonic scalpel based upon accessibility to the primary tumor site. In case of suspicion of inadequate resection, margins were sent for frozen section and wide local excision (WLE) was revised accordingly. The defect created was either primarily closed as in all the cases of carcinoma of tongue or a split thickness skin graft was harvested and was used to cover the defect as in most of the cases of buccal mucosa . In case of a larger defect, loco regional flaps were utilised to reconstruct the defect.
Histopathological examination of the lymph nodes included grossing, hematoxylin and eosin staining and serial step sectioning with a minimum of 5 slices to a variable maximum number, each measuring upto 5 microns were obtained. In highly suspicious nodes with presence of micrometastases or sinus histiocytosis, Immunohistochemistry for pancytokeratin was utilised. In the study group, a revision histopathological examination were carried out on the sentinel lymph nodes which were reported negative for metastases by serial step sectioning and IHC. Patients were referred for post-operative radiotherapy (PORT) based upon the histopathology.
Statistical Analysis
Analysis was conducted using IBM SPSS statistics version 22.0. The data was entered in a predesigned proforma. Descriptive statistics was used to describe different variables. These included measures of central tendency and dispersion for continuous variables and frequencies as well as proportions for categorical variables. All point estimates were supplemented with their corresponding 95% confidence interval. Discrete categorical data was represented in the form of either a number (n) or percentage (%). Continuous data, assumed to be normally distributed, was written in the form of its mean and standard deviation and skewed data was written in the form of its median and interquartile range, as per the requirement. The normality of quantitative data was checked by measures of Kolmogorov - Smirnov tests of normality. Proportions were compared using Chi square or Fisher’s exact test, depending on their applicability. Pearson’s correlation coefficient was used to test the relationship between variables. All the statistical tests were two-sided and were performed at a significance level of α=0.05. Diagnostic accuracy was measured by calculating the Sensitivity, Specificity, Positive predictive value and Negative predictive value in both study and control groups.
Results
40 patients were recruited, 20 each into study and control groups between December 2016 and January 2018. The details of demography, primary tumor and its characteristics, type of neck dissection for both the groups have been described in the Table 1 below.
Table 1. Demography and various parameters for patients of study and control groups.
| Characteristics | Study Group (n=20) | Control Group (n=20) | Total (n=40) |
|---|---|---|---|
| Age (Mean ± SD In Years ) |
52.3 ± 16.3 | 50.35 ± 10.8 | |
| Sex | |||
| Male | 13 (65%) | 15 (75%) | 28 (70%) |
| Female | 7 (35%) | 5 (25%) | 12 (30%) |
| Addictions | |||
| Present | 11 (55%) | 14 (70%) | 25 (62.5%) |
| Absent | 9 (45%) | 6 (30%) | 15 (37.5%) |
| Oral Cavity Subsite | |||
| Tongue | 13 (65%) | 13 (65%) | 26 (65%) |
| Buccal Mucosa | 6 (30%) | 5 (25%) | 11 (27.5%) |
| Rmt | 1 (5%) | - | 1 (2.5%) |
| Alveolus | - | 1 (5%) | 1 (2.5%) |
| Lip | - | 1 (5%) | 1 (2.5%) |
| Tnm Staging | |||
| Clinical | |||
| Stage I (T1n0m0) | 5 (25%) | 4 (20%) | 9 (22.5%) |
| Stage Ii (T2n0m0) | 15 (75%) | 16 (80%) | 31 (77.5%) |
| Pathological | |||
| N + | 6 (30%) | 9 (45%) | 15 (37.5%) |
| N1 | 4 | 1 | 5 |
| N2b | 2 | 8 | 10 |
| N - | 14 (70%) | 11 (55%) | 25 (62.5%) |
| Neck Dissection | |||
| Snd | 17 (85%) | 15 (75%) | 32 (80%) |
| Mnd | 3 (15%) | 5 (25%) | 8 (20%) |
| Operating Time ( Mean ± Sd In Hours ) |
2.46 ± 0.48 | 3.09 ± 0.87 | P value 0.007 |
| Tumor Depth | n = 17 | n = 16 | 33 |
| Range In Mm | 1 - 13 | 1 - 20 | |
| Mean ± SD In Mm | 7.24 ± 2.84 | 8.81 ± 5.504 | |
| Complication Rate | 10% ( 2 / 20 ) | 30% ( 6 / 20 ) | 20% ( 8 / 40 ) |
| Recurrence Rate | NIL (n = 19 ) | 5.3% ( 1 / 19 ) | 2.6% ( 1 / 38 ) |
| Death Rate | 5% (1 / 20 ) | 10% (2 / 20) | 7.5% (3 / 40) |
In our study, we have compared the Sentinel lymph node (SLN) identification rate on lymphoscintigraphy, on SPECT-CT and with gamma probe use. This is defined as identification of at least one sentinel lymph node in every patient. The SLN identification rate was same with lymphoscintigraphy and SPECT-CT i.e., the sentinel lymph node levels on lymphoscintigraphy correlated well with those on the SPECT-CT.
Therefore, we have compared the identification rates on SPECT-CT with that of the Gamma probe. The sentinel lymph node identification rate with the SPECT-CT alone was 70% i.e., 14 out of 20 patients had SLNs detected. The 6 patients whose SLNs were not localised on lymphoscintigraphy or SPECT-CT imaging were the 6 cases of carcinoma of buccal mucosa. The Sentinel lymph node identification rate with the gamma probe use intra-operatively was 100 % i.e., all 20 cases had ≥ 1 SLN identified.
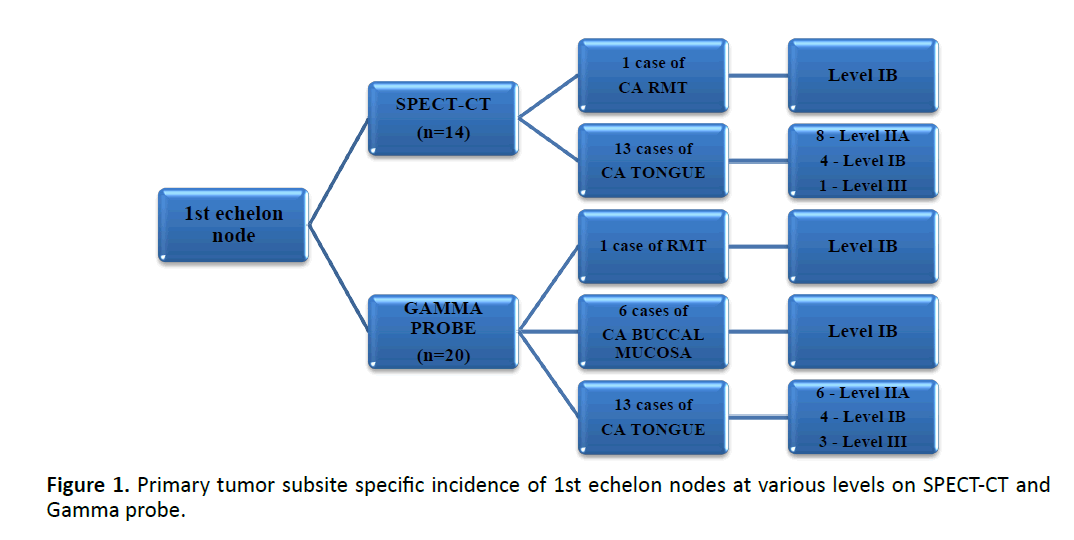
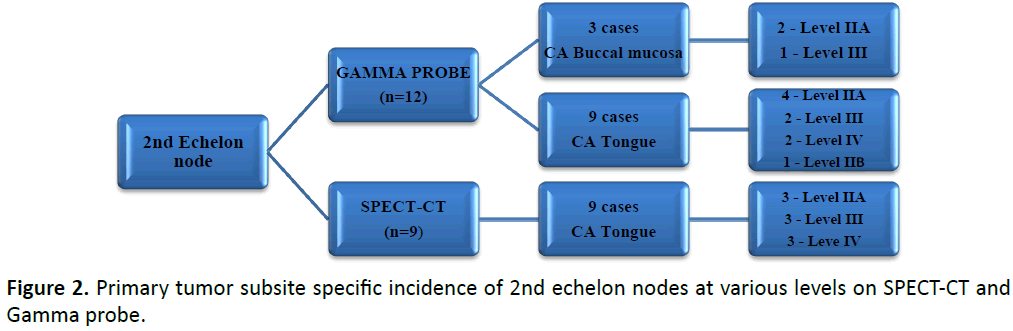
The incidence of various levels of 1st, 2nd and 3rd echelon nodes for various oral cavity subsites on SPECT-CT and Gamma probe localisation was recorded as shown in Figures 1 & 2 and Table 2.
Table 2. Overall incidence of 3rd echelon nodes at various levels on Gamma probe in CA Tongue.
| SLN Levels | Gamma Probe (n=5) |
|---|---|
| Level III | 1 (20%) |
| Level IV | 4 (80%) |
| Total | 5 (100%) |
However, 3rd echelon nodes were only recorded on gamma probe localisation in 5 cases of tongue carcinoma.
In the study group, a total of 21 neck sides were examined in 20 patients and a total of 458 lymph nodes were harvested out of which 208 were the sentinel lymph nodes with an average of 10.4 SLNs harvested per person. Out of 458 LNs harvested, 25 (5.5%) were metastatic of which 20 (80%) were sentinel lymph nodes i.e., the true positives. Remaining 5 (20%) were non-SLNs i.e., the false negatives. In the control group, a total of 361 lymph nodes were harvested from 20 patients with 20 neck sides out of which 14 (3.9%) lymph nodes were metastatic. Out of the 14 metastatic LNs, 11 (78.6%) were true positives and 3 (21.4%) were false negatives. Diagnostic accuracy was calculated for both groups in terms of their sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) as shown in Table 3.
Table 3. Various parameters of diagnostic accuracy for SLNB and END.
| Sensitivity | Specificity | PPV | NPV | |
|---|---|---|---|---|
| SLNB | 80% | 56.58% | 9.61% | 98% |
| END | 78.57% | 73.48% | 10.67% | 98.8% |
Discussion
In our study, 40 patients i.e., 20 each in the study and the control groups were followed up for a minimum of 6 months in most of the cases after the planned intervention in both the groups.
There was no significant difference between age group of patients in both the groups. Men outnumbered women in both the groups. Observations pertaining to age and sex of the patients in this study were similar to the results of study by de carvalho GM, et al. [6] they showed male preponderance with gender distribution and no statistical difference between their groups in terms of age distribution of the patients
The most common oral cavity subsite involved by the primary tumor was tongue in both groups followed by buccalmucosa. The subsite distribution of primary lesion was concurrent with the reviews of Warnaulasuriya S, et al. [7] which states that most common oral cavity subsite in oral cancer is tongue in European and US populations whereas it is the buccal mucosa in the asian population.
TNM staging was studied for both the groups. Majority of the patients in both the groups (75% and 80%) were T2 N0 M0 i.e., stage II pre-operatively. In our study, neck nodal metastasis in stage II patients outnumbered that stage I patients.
In the study group, 6 out of 20 (30%) were upstaged to stage III or IVA. Out of 4 patients who were stage II, 3 (75%) were upstaged to stage III and 1 (25%) was upstaged to stage IVA. Out of 2patients who were stage I, 1 (50%) were upstaged to stage III and 1 (50%) was upstaged to stage IVA. Whereas in the control group, 9 out of 20 (45%) were upstaged to stage III or IVA. All 9 patients were stage II preoperatively. Out of 9, 8 (88.8%) were upstaged to stage IVA and 1 (11.1%) was upstaged to stage III. There was upstaging for stage I and II disease by SLNB by approximately 40% and 26.6% respectively. This was not synchronous with the results of study by Alkureishi LW, et al. [8] where they concluded that T stage has significant correlation with nodal metastasis and also showed a risk of upstaging by SLNB for T1 and T2 tumors of approximately 30% and 50%. In the control group, END upstaged stage II disease by approximately 56.25%.
The sentinel lymph node identification rate in our study was 100% with combined use of imaging and intra-operative gamma probe whereas it was 70% with only imaging which included lymphoscintigraphy and SPECT-CT whereas in study by Schilling C, et al. [9] the SLN identification rate was 99.5% with lymphoscintigraphy and gamma probe use. The SLN identification rate was same on comparing lymphoscintigraphy and SPECT-CT in contrast to study by Toom IJD, et al. [10] in which they concluded that use of SPECT-CT in addition to lymphoscintigraphy identified additional SLNs and upstaged the procedure. In our study, the 30% of patients whose SLNs were not detected on imaging were the cases of carcinoma of Buccal mucosa where intra-operative gamma probe identified the SLNs in all these cases. So far, no studies have been done exclusively on SLNB of carcinoma of buccal mucosa to determine its role. Also the identification rate of multiple SLNs was better with intra-operative gamma probe use when compared to the imaging.
We studied the incidence of 1st, 2nd and 3rd echelon nodes in all the patients undergoing SLNB and compared them with the use of imaging and gamma probe. The 1st, 2nd and 3rd echelon nodes were determined by correlating the lymphoscintigraphy and SPECT-CT imaging with the intra-operative radioactive counts of the lymph nodes on the application of the gamma probe. Overall incidence of 1st echelon node was highest at level IIA with imaging and at level IB with gamma probe use. While the subsite specific incidence showed highest incidence at level IIA for ca tongue cases on both imaging and probe use and at level IB for buccal mucosa and RMT cases.
2nd echelon nodes were detected in 9 cases of CA tongue on imaging and in additional 3 cases of CA buccal mucosa on gamma probe. The overall incidence of 2nd echelon nodes was equal in levels IIA, III and IV on imaging and was highest in level IIA followed by III on probe use. The site specific incidence of 2nd echelon nodes for ca tongue was equivalent in levels IIA, III and IV on imaging whereas it was highest in level IIA with gamma probe.
3rd echelon nodes were detected in 5 cases of CA tongue intra-operatively with gamma probe use with highest incidence in level IV in 4 patients (80%). So far studies have showed total number of SLNs detected but none of the studies have demonstrated in detail about the various levels of echelon nodes in OCSCC.
The operating time differed for the study and control groups and the difference was statistically significant with reduced operating time in the SLNB group. In our study, this difference was due to the pre-determined neck node levels that were to be explored and dissected in the study group when compared to the control group. Extensive exploration and dissection of the neck was avoided in majority of the patients in the SLNB group with the added advantage of detecting the residual radioactivity pointing to missed or residual SLNs by using the gamma probe intra-operatively which were quickly removed. Also few cases in the control group needed defect reconstruction with locoregional flaps which could have increased the operating item in this group. Previous studies similar to our study do not mention about the operating time in their conclusions.
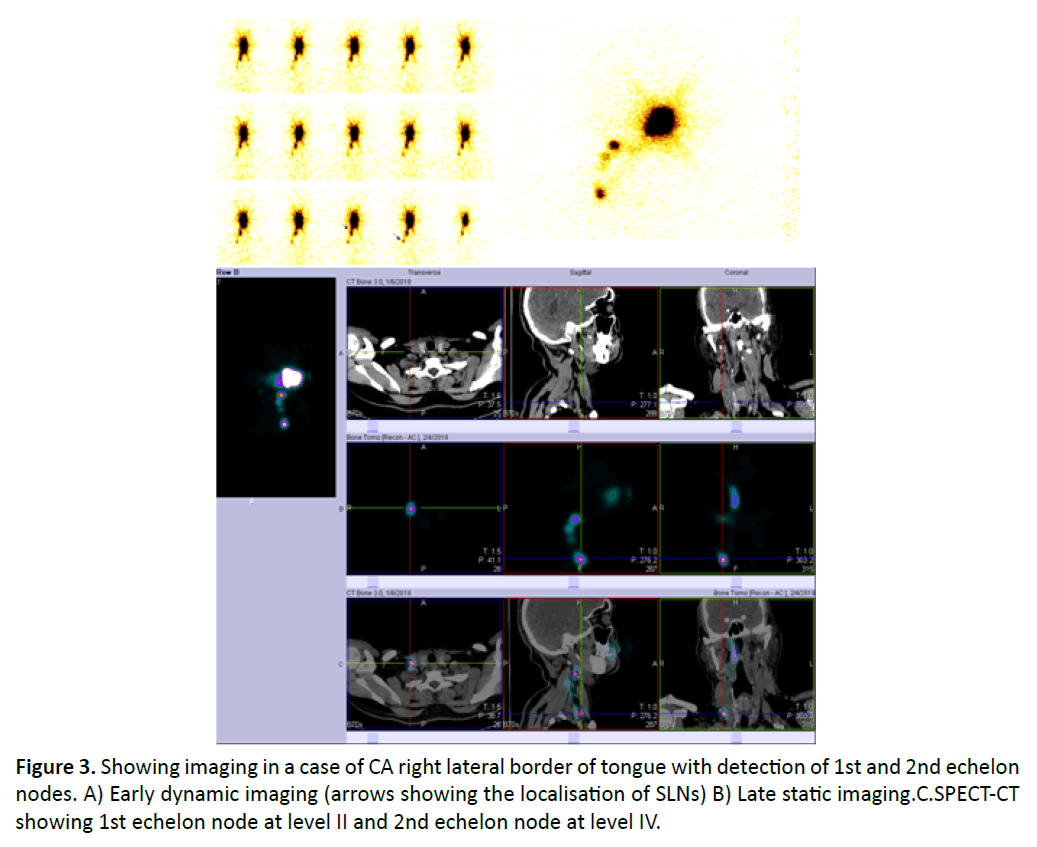
The diagnostic accuracy of SLNB in our study in terms of SLN identification rate, sensitivity, specificity, positive predictive value (PPV) and the negative predictive value (NPV) were 100%, 80%, 56.58%, 9.61% and 98% respectively. We quote two biggest meta-analysis in the literature studying the diagnostic accuracy of SLNB in OCSCC. In study by Hassan O, et al. [11] the sensitivity, specificity, PPV, NPV were 93%, 100%, 100%, 97% respectively and in study by Liu M, et al. [12] the SLN identification rate, sensitivity and NPV were 96.3%,87% and 94% respectively. The revision histopathological examination performed in the study group by further serial slicing and Immunohistochemistry for pancytokeratin identified 2 patients Figure 3 with positive SLNs one each in both the patients which increased the number of true positives and increased the sensitivity of the procedure from 78.2 % to 80 %.
Conclusion
High Sentinel lymph node identification rate using SPECT-CT and gamma probe localisation and high NPV render SLNB as a reliable modality that can be practiced with available resources in cases of early stage oral cavity squamous cell carcinoma facilitating the practice of selective neck dissection thus avoiding the morbidity associated with extensive procedures like END or MND. Detailed histopathological examination of the sentinel lymph nodes by serial step sectioning and immunohistochemistry for pancytokeratin increases the sensitivity of SLNB and detects micro metastasis. SLNB has definitive role to play in early stage carcinoma of tongue whereas its role in other subsites of the oral cavity like buccal mucosa need to be studied distinctively.
References
- Woolgar JA. Detailed topography of cervical lymph node metastases from oral squamous cell carcinoma. Int J Oral Maxillofac Surg. 1997; 26: 3‑9.
- Nieweg O, Tanis P, Kroon B. The definition of a sentinel node. Ann surg oncol. 2001, 8(6): 538-41.
- Ziessman HA, O’Malley JP, Thrall JH. Oncology: Non-positron emission tomography. Nuclear medicine-the requisites. In: Fahey FH, editors. Philadelphia: Saunders Elsevier 2014; 281-3.
- Ziessman HA, O’Malley JP, Thrall JH. Radiation detection and instrumentation. Nuclear medicine-the requisites. In: Fahey FH, editors. Philadelphia: Saunders Elsevier 2014; 42-4.
- Ziessman HA, O’Malley JP, Thrall JH. Radio pharmaceuticals. Single-Photon Emission Computed Tomography, Positron Emission Tomography, and Hybrid Imaging. In: Fahey FH, editors. Philadelphia: Saunders Elsevier 2014; 56-7.
- De Carvalho GM, Dias VG, Kohler H, Chone CT, Guimaraes AC, et al. Sentinel Lymph Node Biopsy vs. Elective Neck Dissection in Patients with T1/T2 N0 Oral Squamous Cell Carcinoma: A Matched Pair Analysis. Int J Oral Craniofac Sci. 2016; 2(1): 047-51.
- Warnakulasuriya S. Global epidemiology of oral and oropharyngeal cancers- A review. Oral Oncol. 2009; 45: 309-16.
- Alkureishi LW, Ross GL, Shoaib T, Soutar DS, Robertson AG, et al. Does tumor depth affect nodal upstaging in squamous cell carcinoma of the head and neck?. Laryngoscope. 2008; 118(4): 629-34.
- Schilling C, Stoeckli SJ, Haerle SK, Broglie MA, Huber GF, et al. Sentinel European Node Trial (SENT): 3-year results of sentinel node biopsy in oral cancer. Eur J Cancer. 2015; 51:2777-84.
- Toom IJD, Schie AV, Weert SV, Karagozoglu KH, Bloemena E, et al. The added value of SPECT-CT for the identification of sentinellymph nodes in early stage oral cancer. Eur J Nucl Med Mol Imaging. 2017; 44: 998-1004.
- Hassan O, Taha MS, Mehairy HE. Sentinel lymph node biopsy versus elective neck dissection in evaluation of cN0 neck in patients with oral and oropharyngeal squamous cell carcinoma. Systematic review and meta-analysis study. Egypt J Ear Nose Throat Allied Sciences. 2015; 16: 25-34.
- Liu M, Wang SJ, Yang X, Peng H. Diagnostic Efficacy of Sentinel Lymph Node Biopsy in Early Oral Squamous Cell Carcinoma: A Meta-Analysis of 66 Studies. Plos One. 2017; 1-18.