Review Article - Asian Journal of Biomedical and Pharmaceutical Sciences (2022) Volume 12, Issue 90
Review article on pathogenesis of malarial fever.
Bhawana Vadde*
Department of Nursing, Florence Nightingale Training College of nursing, Sawangi (M), Wardha, India
- *Corresponding Author:
- Bhawana Vadde
Department of Nursing
Florence Nightingale Training College of Nursing
Sawangi (M)
Wardha
India
E-mail: vaddebhawna7@gmail.com
Received: 23-May-2022, Manuscript No. AABPS-22-66332; Editor assigned: 25-May-2022, PreQC No. AABPS-22-66332(PQ); Reviewed: 08-June-2022, QC No. AABPS-22-66332; Revised: 11-June-2022, Manuscript No. AABPS-22-66332(R); Published: 18-June-2022, DOI:10.35841/2249-622X.90.130
Citation: Vadde B. Review article on pathogenesis of malarial fever. Asian J Biomed Pharmaceut Sci. 2022;12(90):130
Abstract
Malaria, a severe illness is caused by a parasite. It carries on to be a threat to the wellbeing in several nations. In the article here, the introduction, life cycle, pathologic process, diagnosis, treatment of protozoal infection is presented in Associate in nursing exceedingly comprehensive manner. Plasmodium, is the etiologic agent of protozoal infection preponderantly Plasmodium falciparum. Transmission involves 2 hosts-definitive host is feminine genus Anopheles |arthropod genus} mosquito during which it completes its sexual cycle (Anopheles Gambiae and Anopheles funetus) and Human-the host within which the vegetative cycle is completed. 50% of the globe population remains in danger for acquiring this deadly illness though the incidence has greatly reduced over the decades. Globally, the morbidity and fatality estimates of protozoal infection have lessened although few dispatches in in African nation there was a high incidences of malaria. In some malaria-endemic areas, protozoal infection transmission is therefore severe that a corpulent magnitude of community is infected nonetheless not created sick by the parasites. This host has developed sufficient immunity to protect against protozoan disease, but is not a protozoan infection. In this situation, finding a protozoan parasite in a sick folk doesn’t always mean that the disease is the induced by a parasite. There square measure varied prophylactic agents available together with antimalarial regimens. Vaccination for prevention is available. However, because resistance is widespread between commonly used drugs and pesticides, three vaccine strains and many new compounds are consistent with diagnostic and clinical studies.
Keywords
Malaria, Anopheles, Plasmodium falciparum, Vaccine, Protozoa.
Introduction
Malaria can be a serious Diseases caused by parasites that infect humans by being bitten by infected female arthropod mosquitoes. Prevention and treatment are possible. The word protozoal infection is from Latin word os aria which means “foul air”.
Transmitted by bite of the feminine arthropod genus dipteran, protozoal infection is result of completely unlike species of plasmodium particularly Plasmodium vivax Plasmodium falciparum, Plasmodium knowlesi, Plasmodium ovale and Plasmodium malaria. Of these the falciparum species is what the reason behind the lions share fatalities is. Ol-ld the Africa [1,2]. Plasmodium vivax incorporates a wide distribution however the chance of infection is tokenish as a result of African populations lack the Duffy factor. With timely treatment, the general public expertise fast resolution of symptoms; but, important complications could occur, as well as cerebral protozoal infection, severe protozoal infection anemia, coma, or death.
According to World Health Organization, In 2019, there have been AN calculable 229 million cases of protozoal infection across the world. The calculable range of protozoal infection A total of 409,000 people died in 2019.Children whose age is underneath five years are the foremost endangered cluster stricken by malaria; in 2019, they accounted for sixty seven (274 000) of all protozoal infection deaths all over the globe [2,3].
The World Health Organization African Area carries an unjustifiably high rate of the worldwide protozoal infection burden. In 2019, the region had ninety four of protozoal infection incidences and fatalities. Total endowment for protozoal infection management and eradication reached a calculable US$ three billion in 2019. Benefactions from governments of several local countries resulted an estimated amount of US$ 900 million, representing thirty first of the resultant funding.
In India, approximately one three billion people are at excessive chance of contracting malaria. India is chargeable for 2% of world malaria times and 2% of global wide malaria deaths (fifty two percentages of all malaria deaths out of doors of sub-Saharan Africa). India additionally bills for 85.2% of the malaria burden in Southeast Asia.
India accounts for 47% of global P. vivax malaria cases, making it very important to combat malaria worldwide, especially in Southeast Asia. The country has made great strides in combating and eradicating malaria. In 2019, there were 6.8 million fewer cases than in 2016, and the number of cases per 1,000 people at risk fell from 10 to 433. Over the same period, mortality rates ranged from 0.018 to 0.006 people at Peril [2-4].
Malaria has a noteworthy financial impact on Indian families with the direct pocket money of 4,444 people from$ 0.34 to $ 7.66 (average $ 2.67), with a 24-day loss of productivity. The yearly cost of malaria in the United States is approximated to be around US$1940 million. 2018, only 7 of 36 U.S. states had 90% of suspected cases [5]. Like other states in northeastern India, this state has forest-like rolling hills, tribal or conflict zones, and has a high incidence of malaria. Even in states where malaria transmission is minimal, the most of malaria cases are concentrated in areas with the Geographical or sociopolitical characteristics mentioned above [5-7].
Life cycle of Malarial Parasite
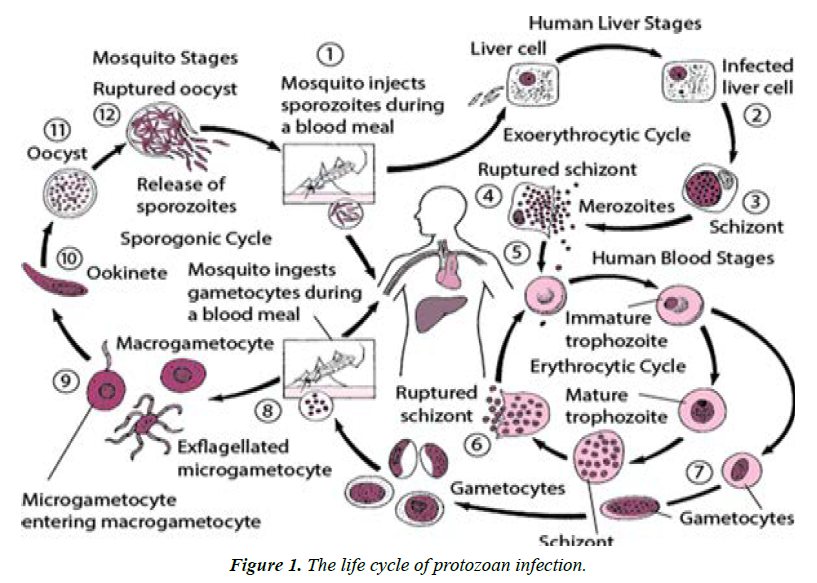
Plasmodium sporozoan is transmitted to people once insects increase your chances by biting your skin, examining the blood vessels to feed, and secreting various vasodilators. Finding blood vessels and inserting saliva into the blood to forestall coagulation 30-60 minutes after immunization, sporozoite-like filaments are delivered to liver by the cardiovascular system [8]. Within On 712 days, sporozoite transforms into meristem and can last up to 30. Advance Merozoites that disrupt liver cells. Meanwhile, some vivax and ovoid sporozoites are hypnotic, which may stay for months or years in the liver and can revert in affected individuals. Patients appear to have relapsed with a protozoan pyrexia infection for several years. When deed an epidemic space [9]. It suggests that, a minimum of sometimes, falciparum incorporates a dormant stage; the apomictic cycle begins, with the Merozoites incursive blood corpuscle to grow by intense Hb [10]. Inside the host blood corpuscle, Parasites develop into late sporangia in the first annular stage, thus resulting in up to 32 Merozoites counting in a species of parasites with division stages involving VI during mitosis [11].
As soon as the red blood cell division disrupts, the released Merozoites advance into their life cycle, penetrating into various red blood cells. Alternating fever usually occurs Just in time Up to or now of blood corpuscle ruptures as schizonts disrupt to unleash unfamiliar infectious Merozoites [12,13]. Is happens each forty eight h in tertian protozoal infection and each seventy two h in fundamental quantity protozoal infection. throughout this perennial cycle, Some merozoites differ in the sexual morphology of males {and females} called erythroid gamete mother cells with one nucleus and so pending the arrival of a blood seeking female arthropod genus dipteran Infiltration of dipteran gametocytes causes flagellation, infiltration into macrogametes, zygotes formation or growth of microgametes formed as a result of fertilization [13,14].The zygotes transform ookinetes and so become a spherical oocyst. Within the oocyte, the nucleus divides again and again, with the creation of an outsized range of sporozoites and enlargement of the oocyst. Once the sporozoites are totally shaped, the oocyst ruptures, cathartic the sporozoites into the haemocoel (the mosquito’s body cavity). Sporozoites migrate to the secretory glands and end their life cycle. Uptake of sporozoite by mosquito glands. When introduced into an entirely new human host, the life cycle of protozoan infection continues (Figure 1).
Pathogenesis
Gametocytes and nonsexual stage of parasites will adhere to the tube epithelial tissue of assorted organs like respiratory organ heart brain liver urinary organ placenta and hypodermic tissue. Severe complications like cerebral protozoal infection is that the results of parasite sequestration that happens [15]. There's native drive because the blood flow is reduced that the replication and IRBC projecting to non-infected red blood cell is promoted.
Plasmodium falciparum vivax and everyone will type 'rosettes' that may be a type of cyto adherence. Plasmodium falciparum is that the one inflicting dangerous complication. Once the protozoal infection parasite entry in our body varied inflammatory cells like neutrophils monocytes NK cells in conjunction with the inflammatory mediators are discharged. This manifests as fever, headaches, nausea and different consequences. An important issue causative to serve type of illness is that the imbalance in unharness of professional and anti-inflammatory mediators. Though protozoal infection is one in all the most important causes for morbidity not everybody UN agency gets infected is seriously unwell or dies. Frequent exposure to the parasites in endemic areas results in acquisition of specific immunity and so serious issues are restricted to kids. Malaria in older generation will manifest as delicate febrile unhealthiness.
Transmission
According to UN agency in most cases, protozoal infection is transmitted through mosquitoes. About thirty major carriers of protozoan infections. All kinds of vectors you need are biting between darkness and dawn. The strength of Transmission depends on factors related to the parasite, the vector, the human host, and the environment [16].
Anopheles mosquitoes lay their eggs in water and the larvae hatch into adult mosquitoes. The feminine mosquitoes look for provender to cherish their eggs. all kinds of anopheles dipterous insect has its own most well-liked aquatic habitat; as an example, some like Small, shallow H2O collections such as puddles and hoof prints abound in tropical countries throughout the season. The transmission is particularly powerful where deep terrans have a longer duration (to give the parasite time to complete development in mosquitoes) and prefer to bite humans over a variety of animals. Longterm and persistent human bites the presence of 4,444 vector species on the continent is the main conclusion that about 90 of the world's protozoan infections occur in Africa.
Transmission is conjointly dependent on climate which will have an effect on the amount and lifespan of mosquitoes, like downfall patterns, febricity and humidness. In some areas, transmission is seasonal, there are elevations throughout the season, and only occurs once per season. Protozoan epidemics will begin when climatic and other conditions suddenly promote transmission in the area wherever folks have very low or no immunity to protozoal infection. They will together occur once folks with low immunity get into areas with profound protozoal infection transmission, as an example to seek out job, or as refugees [17]. The man’s immunity is in addition a necessary issue, especially for adults in regions with moderate to intense communication. Partial immunity develops over the period of exposure and does not provide complete security, but it will scale back the danger that protozoal infection can cause serious illness. For this, most protozoal infection deaths in continent occur in little kids, in areas where transmission is low and immunity is low, all age groups are at danger.
Malaria in Pregnancy
Congenital malaria is caused through the transmission when Parasites or infected red blood cells pass from mother to newborn during or during labor, rather than by a female anopheline mosquito bite [18].
Diagnosis in pregnancy
Microscopic diagnosis enables for species identification and parasitaemia calculation, allowing for the prescription of appropriate anti-malarial. Rapid detection tests can miss the low levels of parasitaemia that are common in pregnant women, and rapid detection tests for Vivax malaria are relatively insensitive [19].
The vegetative form of mature Plasmodium falciparum and the presence and number of schizonts should be documented as important prognostic parameters in peripheral blood smears. Malaria pigment is found in more than 5% of poly morpho nuclear leukocytes in peripheral blood films. Medications in pregnancy may be less effective However; this effect may be related to a decrease in the concentration of antimalarial drugs during pregnancy. Women should be informed of the likelihood of relapse and appropriate follow-up plans. Example: If symptoms or fever reappear, blood counts should be repeated. Once in 7 days blood film screening, on the other hand, can help diagnose and treat malaria early. In Thailand, this has been found to minimize maternal mortality due to malaria. Although there is no evidence of weekly blood smears in the UK. Because Thailand is a region with less endemic disease, the immune levels of Thai women are similar to those of non-endemic females in the United Kingdom.
Risk of infection of the disease to the baby vertically,
1. If there is an infection during labor and the placenta and umbilical cord become infected, vertical transmission to the fetus can occur. Malaria was detected on a blood test.
2. For malaria during labor using a standard microscope of a thick and thin blood smear and weekly blood smears over the next 28 days [18,19].
Diagnosis: Protozoal disease designation involves various protozoal infection parasites or antigens/products in patient blood. Protozoal infection ought to be directly treated because it is medical emergency. Clinical affiliation bets on Signs and symptoms of the patient and the results of the physical examination. The initial manifestations of protozoan infection are highly variable and varied Fever, headache, weakness, myalgia, chills, dizziness, abdominal pain, diarrhea, nausea, emesis, loss of appetite, itching [20,21].
Malaria is analyzed victimization completely distinctive styles e.g., typical microscopic designation by staining skinny and thick peripheral blood smear, alternative concentration techniques, e.g.
1. quantitative buffy coat (QBC) technique
2. fast diagnostic tests, [21,22]
4. Para Screen, [24]
5. SD Bio line, [25]
6. Para check, and
7. molecular diagnostic ways, like enzyme chain reaction (PCR) [26]
Anti-Malarial drugs
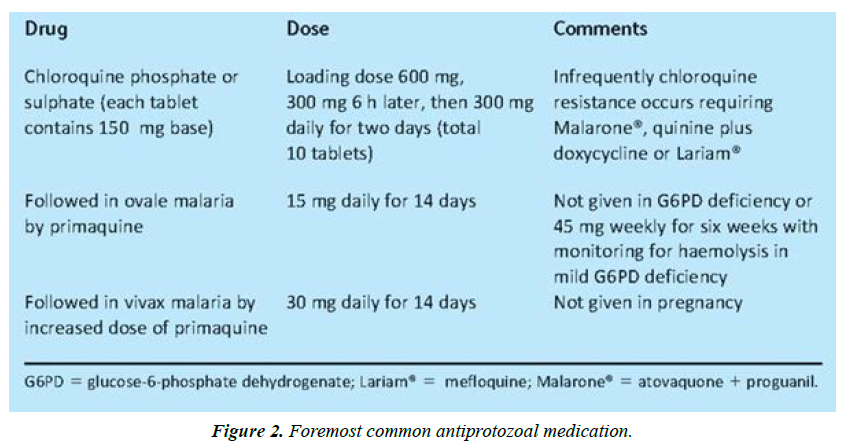
The foremost common antiprotozoal medication includes:
Chloroquine phosphate was being used as one of the most popular drugs in the aid of the disease worldwide. But the resistance acquired to the drug due to Chloroquine resistant molecule (PfCRT) undergoes mutation which leads to little quantity of the drug accumulation in the food cavum. All the strains of plasmodium were at risk because of it being an effective schizonticidal agent [27].
Prim quinine, which blocks the spread of malaria, is efficient contra to P vivax and P ovale infection proves lethal to the gametocytes. It is a weak action against the asexual stage of blood vivax malaria. Antimalarial drugs, usually in combination with blood schizonticide against red blood cell parasites, successfully treat reversible protozoal infections caused by vivax or ovale.
Also known as Artemisinin-based combination therapy is ACT is a mix of two or a lot of medication that employment against the Plasmodium vivax in numerous ways that. This can be typically the well-liked treatment for chloroquineresistant protozoal infection. Examples embody artemetherlumefantrine (Coartem) and artesunate-mefloquine (Figure 2).
Complications and manifestations
1. The classic (but rarely observed) attack of malaria lasts 6-10 hours. It consists of
2. A cold stage (sensation of cold, shivering)
3. A hot stage (fever, headaches, vomiting; seizures in young children); and
4. Finally a sweating stage (sweats, return to normal temperature, tiredness).
5. The presenting features include: Hyperthermia, headaches, nausea vomiting malaise etc.
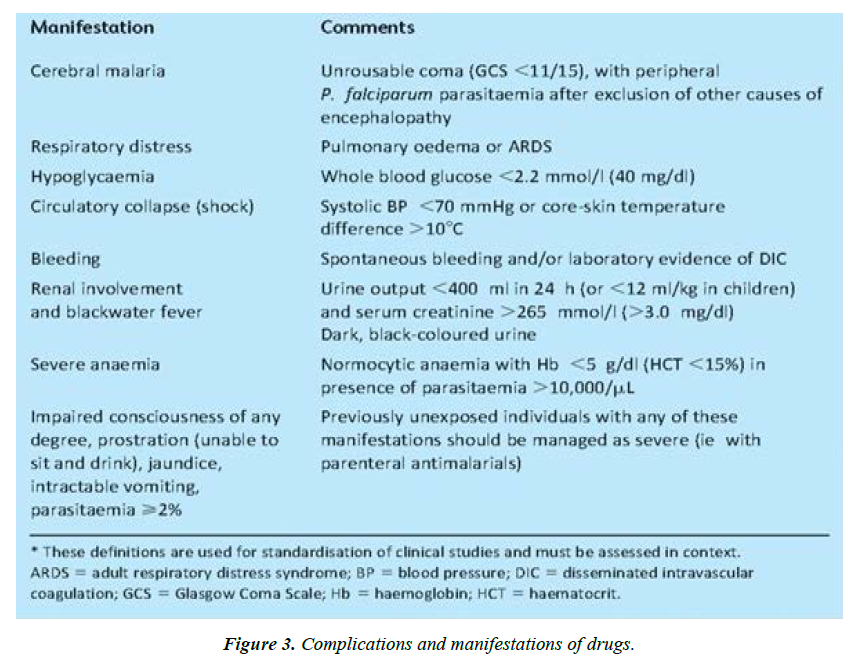
The fatal infection which concerns 15 percent of four thousand to five thousand cases of malaria being reported per annum proves to be severe form of the disease. Just like p. falciparum the cerebral malaria is often fatal. Other complications include multi organ failure-Which makes malaria a fatal systemic disease with increasing rate of mortality. At time of diagnosis of the infection mortality is related to the presenting neurological involvement, Respiratory insufficiency, Circulatory shock, metabolic acidosis and hyperlactatemia (Figure 3).
Prevelance of Malaria
Malaria imposes an exceptional socio-financial With the burden on mankind and six diseases (diarrhea, Acquired immunodeficiency syndrome, TB, measles, Hep B, and pneumonia), debts for eighty five percent of worldwide infectious disorder burden. Malaria torments ninety nations and provinces with inside the equatorial and semitropical regions, and nearly one 1/2 of them are in Africa, Southern Sahara. About thirty six percent of the sector public (i.e., 2020 million) is uncovered to the chance of being affected with malaria. The WHO surveys 300-500 million malaria instances per annum, with ninety% of this case load being present in Africa. In addition, the expected annual fatality caused by malaria degrees from 700 K to 2.7 million worldwide and > Seventy five percent of them are African kids and pregnant mothers. Queries were declared approximately reliability of those estimates due to the fact maximum that there is a lack of reliable diagnostic centers and reporting systems, especially in Africa's ultra-high and holo-endemic countries.
In the Southeast Asia the World Health Organization, of 1.four billion humans dwelling in eleven nations (land stretch, 8,466, six hundred km2; that is, 6% of worldwide stretch), 1.2 billion are uncovered to the chance of malaria, maximum of which stay in India. Five None, Southeast Asia contributed to most effective. Five million instances to the worldwide load of malaria. Among this, India on my own contributed seventy six percent of the entire instances. Taking into consideration scientific episodes, it has now been expected with the assist of epidemiologic fashions and geographical and demographic facts that Plasmodium falciparum assessments outdoor Africa, especially in Southeast Asia, are 200% better than said via way of means of the World Health Organization (i.e., 118. ninety four million of worldwide evaluation of five hundred fifteen million instances). In summation to this, load of P. vivax malaria with inside the international has been calculated at 71-eighty million instances, of which Southeastern Asia and Westernern pacific nations subsidized forty two million instances.
References
- https://www.vivaxmalaria.org/india
- Who. World malaria report 2020: 20 years of global progress and challenges. World malaria report. 2020:1-51.
- Narain JP, Nath LM. Eliminating malaria in India by 2027: the countdown begins!. The Indian journal of medical research. 2018 Aug;148(2):123.
- Nureye D, Assefa S. Old and recent advances in life cycle, pathogenesis, diagnosis, prevention, and treatment of malaria including perspectives in Ethiopia. The Scientific World Journal. 2020 Feb 14;2020.
- Warrell DA, Gilles HM. Essential malariology. CRC Press; 2017 Dec 14.
- Carter R, Mendis KN. Evolutionary and historical aspects of the burden of malaria. Clinical microbiology reviews. 2002 Oct;15(4):564-94.
- National Institutes of Health. Understanding malaria. Fighting an ancient scourge. US Department of Health Human Services. 2007.
- Krettli AU, Miller LH. Malaria: a sporozoite runs through it. Current Biology. 2001 May 15;11(10):R409-12.
- Centers for Disease Control and Prevention. The history of malaria, an ancient disease. Global Health, Division of Parasitic Diseases and Malaria ed. 2010.
- Rollinson D, Hay SI, Price R, Baird JK. The Epidemiology of Plasmodium vivax: History, Hiatus and Hubris, Part B. Academic Press; 2013 Jan 31.
- World Health Organization. World malaria report 2015. WHO; 2016 Jan 30.
- World Health Organization. World Malaria Report 2012. World Health Organization; 2012.
- Kalilani L, Mofolo I, Chaponda M, Rogerson SJ, Alker AP, Kwiek JJ, Meshnick SR. A randomized controlled pilot trial of azithromycin or artesunate added to sulfadoxine-pyrimethamine as treatment for malaria in pregnant women. PLoS One. 2007 Nov 14;2(11):e1166.
- McGready R, Stepniewska K, Lindegardh N, Ashley EA, La Y, Singhasivanon P, White NJ, Nosten F. The pharmacokinetics of artemether and lumefantrine in pregnant women with uncomplicated falciparum malaria. European journal of clinical pharmacology. 2006 Dec;62(12):1021-31.
- Salmani Manjunath P, BV PB. Comparative study of peripheral blood smear and quantitative buffy coat in malaria diagnosis.
- Tagbor H, Bruce J, Browne E, Greenwood B, Chandramohan D. Malaria in pregnancy in an area of stable and intense transmission: is it asymptomatic?. Tropical medicine & international health. 2008 Aug;13(8):1016-21.
- Kotepui M, Ratcha C, Uthaisar K. Clinical characteristics, parasite diagnosis and hematological parameters of malaria in Surat Thani Province, Thailand. Journal of Health Research. 2017;31(4):281-8.
- Naber SP. Molecular pathology--diagnosis of infectious disease. New England Journal of Medicine. 1994 Nov 3;331(18):1212-5.
- Ratsimbasoa A, Fanazava L, Radrianjafy R, Ramilijaona J, Rafanomezantsoa H, Ménard D. Evaluation of two new immunochromatographic assays for diagnosis of malaria. The American journal of tropical medicine and hygiene. 2008 Nov 1;79(5):670-2.
- Autino B, Corbett Y, Castelli F, Taramelli D. Pathogenesis of malaria in tissues and blood. Mediterranean journal of hematology and infectious diseases. 2012;4(1).
- Trampuz A, Jereb M, Muzlovic I, Prabhu RM. Clinical review: Severe malaria. Critical care. 2003 Aug;7(4):1-9.
- Aschale Y, Mengist A, Bitew A, Kassie B, Talie A. Prevalence of malaria and associated risk factors among asymptomatic migrant laborers in West Armachiho District, Northwest Ethiopia. Research and Reports in Tropical Medicine. 2018;9:95.
- Micah AE, Su Y, Bachmeier SD, Chapin A, Cogswell IE, Crosby SW, Cunningham B, Harle AC, Maddison ER, Moitra M, Sahu M. Health sector spending and spending on HIV/AIDS, tuberculosis, and malaria, and development assistance for health: progress towards Sustainable Development Goal 3. The Lancet. 2020 Sep 5;396(10252):693-724.
- Patil PS, Chandi DH, Damke S, Mahajan S, Ashok R, Basak S. A retrospective study of clinical and laboratory profile of dengue fever in tertiary care Hospital, Wardha, Maharashtra, India. J Pure Appl Microbiol. 2020 Sep 1;14(3):1935-39.
- Murray CJ, Abbafati C, Abbas KM, Abbasi M, Abbasi-Kangevari M, Abd-Allah F, Abdollahi M, Abedi P, Abedi A, Abolhassani H, Aboyans V. Five insights from the global burden of disease study 2019. The Lancet. 2020 Oct 17;396(10258):1135-59.
- Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, Abbasi-Kangevari M, Abbastabar H, Abd-Allah F, Abdelalim A, Abdollahi M. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020 Oct 17;396(10258):1204-22.
- Franklin RC, Peden AE, Hamilton EB, Bisignano C, Castle CD, Dingels ZV, Hay SI, Liu Z, Mokdad AH, Roberts NL, Sylte DO. The burden of unintentional drowning: global, regional and national estimates of mortality from the Global Burden of Disease 2017 Study. Injury prevention. 2020 Oct 1;26(Suppl 2):i83-95.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref