Case Report - Otolaryngology Online Journal (2020) Volume 10, Issue 4
Pleomorphic Adenoma of the Larynx: A Case Report
Umutoni Josiane*, Victor Nyabyenda, Louise Munezero, Felix ManirakizaCollege of Medicine and Health Sciences, School of Medicine and pharmacy, University of Rwanda, Kigali, Rwanda
- *Corresponding Author:
- Umutoni Josiane
ENT Department, College of Medicine and Health Sciences
School of Medicine and pharmacy
University of Rwanda, Kigali, Rwanda
Email: umujojo125@gmail.com
Received: February 04, 2020; Accepted: July 25, 2020; Published: July 31, 2020
Abstract
Pleomorphic adenomas (PA) also called benign mixed tumors are most common tumors of salivary gland. Pleomorphic adenoma arising from the larynx is very rare. We report a 28 years old male patent who presented with shortness of breath and dry cough since 2 years, treated as asthma. The last crisis the patent warrants an intubaton which failed and warrants an ENT consultaton. ENT examinaton showed a mass in the subglotc region. Afer excision the pathology was in favor of pleomorphic adenoma.
Keywords
Pleormorphic adenoma, Larynx, Airway obstruction
Introduction
Pleomorphic adenomas (PA) also called benign mixed tumor are most common tumors of salivary glands. They occur mainly in major salivary glands but may also arise from minor salivary glands of upper respiratory and alimentary tract [1]. Histologically, these tumors are encapsulated and consist of benign epithelial and/or myoepithelial and stromal elements [2]. About 80% of PAs arise in the parotid gland, 10% in the submandibular gland, and 10% in the minor salivary glands of the oral cavity, paranasal sinuses, and upper respiratory and alimentary tract [3]. Those tumors have the capacity to transform into malignancy when they stay long without treatment [4].
Pleomorphic adenoma arising from the larynx is very rare, the literature report less than 30 cases [5]. Pleomorphic adenoma may occur at any age, but mainly they affect patients in the 4-6 decades with a male to female ration 2:1 [6]. When the larynx is involved, the most common site of involvement is the epiglottis and subglottis in some cases [5].
Case Report
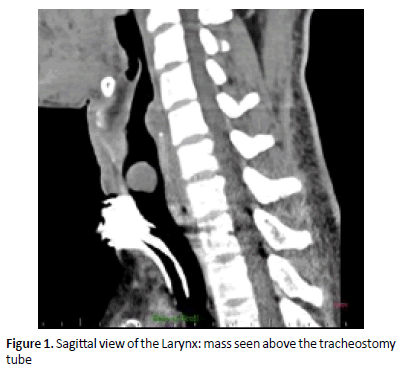
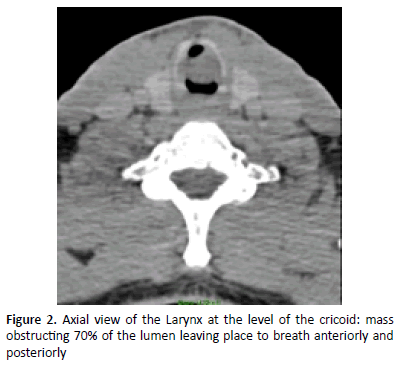
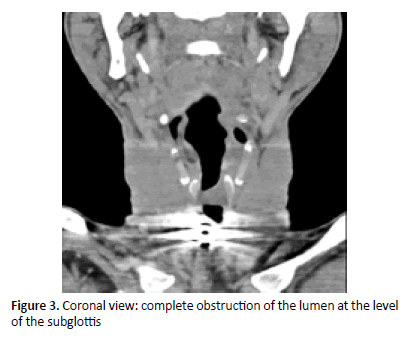
A 28 years old male patient with a 2-year history of shortness of breath, and dry cough. During those 2 years he presented to the accident and emergency department, where he was treated as a patient with asthma crisis. Initially he was improving on asthma treatment by bronchodilators and steroids. However over the course of time the symptoms were increasing in frequency and severity. Lastly the patient presents with severe l respiration distress that has been alleviated by a difficult intubation using a number 6.0 endotracleal tube as the biggest tube to pass in the subglottis and this warranted an ENT consultation. Meanwhile the patient had an accidental ex-tubation and re-intubation was difficult hence an emergent tracheostomy was done. CT scan was performed and showed in figures (Figures 1-3).
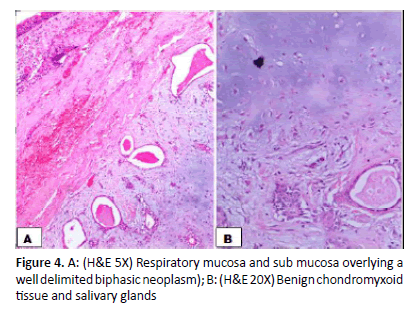
A direct laryngoscopy was done and revealed a submucosal mass arising from the right posterolateral subglottic region extending into the lumen with occlusion of up to 70% with normal vocal cord mobility. According to the history and physical examination the mass was in favor of a benign mass. Endoscopic surgery of the mass was done with complete excision. Macroscopically the mass was submitted as 2 fragments, the biggest was 2x1x0.5 cm and the smallest 0.5x0.5x0.2cm. Microscopy showed respiratory mucosa overlying a well circumscribed, biphasic neoplasm composed of proliferative benign salivary glands into a benign chondromyxoid stroma (Figure 4).
Discussion
For our case there has been a delay in the diagnosis of around 2 years. The literature also reports that usually there is a delay in the diagnosis of those uncommon tumors due to their non-specific clinical presentation [5]. Initially our patient was treated as asthmatic till he warranted an emergency intubation. Therefore, a complete head and neck examination including indirect or direct laryngoscopy with regard to the benign tumors in this organ is necessary for patients with respiratory problems. Current approaches in use for the excision of laryngeal pleomorphic adenomas include lateral pharyngotomy, laryngofissure, and use of laser [5]. As lack of experienced surgeons in the above procedure we did complete endoscopic resection which is usually done for small tumors. At the time of surgery the patient was having a tracheostomy: the tube has been kept for 7 months after surgery with a monthly evaluation of the patency of airway by trans-stomal flexible nasopharyngoscopy and finally a complete decanulation was done. Since then the patient has been reviewed every month for a period of 6 months to exclude any reccurence. At the time of our report the patient had no complication.
Conclusion
We recommend that every patient with signs of upper respiratory tract obstruction must be examined by a head and neck surgeon. The signs of obstruction may include hoarseness of voice, stridor and shortness of breath. This facilitates early diagnosis and prevents morbidity and mortality which may occur if the disease is not recognized early.
Conflict of interest: All authors declare no conflict of interest.
References
- Flint PW. Cummings otolaryngology - head and neck surgery (5th Edn).
- Argat M, Maier A, Mohadjer C, et al. Pleomorphic adenoma of the larynx. Eur Arch OtoRhino Laryngology 1994; 251(5): 304-6.
- Eveson JW, Cawson RA. Salivary gland tumours: A review of 2410 cases with particular reference to histological types, site, age and sex distribution. J Pathol 1985; 146(1):51-8.
- Harada H. Histological investigation regarding to malignant transformation of pleormorphic adenoma (so-called Malignant mixed Tumor) of the salivary Gland Origin: special reference to carcinosarcoma. Kurume Med J 2000.
- Jafari S. Pleormorphic adenoma of the larynx: A case report. Iran J Otorhinolaryngol 2016.
- Datarkar AN, Deshpande A. Giant Parapharyngeal Space Pleomorphic Adenoma of the Deep Lobe of Parotid Presenting as Obstructive Sleep Apnoea: A Case Report & Review of the Diagnostic and Therapeutic Approaches. J Maxillofac Oral Surg 2015; 14(3): 532-7.