Review Article - Asian Journal of Biomedical and Pharmaceutical Sciences (2018) Volume 8, Issue 65
Pathophysiological Ramifications of Diabetic Condition: A Review
Arpit Shahi1, Prasad VSS2, Syed Sarim Imam3, Abdul Muheem4 and Mohammed Asadullah Jahangir3*
1Department of Biotechnology, Deenbandhu Chhotu Ram University of Science and Technology, Sonipat, Haryana, India
2Biochemistry Division, National Institute of Nutrition (ICMR), Tarnaka, Hyderabad, India
3Department of Pharmaceutics, School of Pharmacy, Glocal University, Saharanpur, India
4Department of Pharmaceutics, School of Pharmacy, Jamia Hamdard, New Delhi, India
- *Corresponding Author:
- Mohammed Asadullah Jahangir
Department of Pharmaceutics, School of Pharmacy, Glocal
University, Saharanpur, India
E-mail: asadullahpharma@gmail.com
Accepted on July 4, 2018
DOI: 10.4066/2249-622X.65.18-845
Visit for more related articles at Asian Journal of Biomedical and Pharmaceutical SciencesAbstract
Diabetes is a chronic hyperglycaemic disorder. Due to altered metabolism of insulin and related pathways, consistently raised blood glucose levels leads to manifestation of collateral pathophysiologies or complications. Such long term complications include cardiovascular diseases, nephropathy, neuropathy and retinopathy. Microvascular complications are the major cause of these pathologies. Understanding the etiology of these complications is important to devise effective prevention and treatment strategies. Therefore, the current review was undertaken to enumerate various diabetes related pathologies, the relevant mechanisms, disease progression and available treatment options. The data was collected from major indexing services like-PubMed, Scopus, Google Scholar and some related journals which fall under the scope of the review paper. The major keywords which were used for the collection of data include diabetes, pathophysiology of diabetes, comorbidities of diabetes, diabetes complications, diabetes management, diagnosis of diabetes, diagnosis of comorbidities of diabetes etc. Most of the articles referred are published in last 8 years. However, some relevant articles are also considered which are published before this time frame.
Keywords
Type 1 diabetes, Type 2 diabetes, Diabetic comorbities, Cardiovascular complications, Neuropathy, Nephropathy, Retinopahty
Abbreviations
ACE: Angiotensin-Converting Enzyme; MRI: Magnetic Resonance Imaging; OCT: Ocular Coherence Tomography; CT: Computerized Tomography; DHD: diabetic heart disease; GLP-1: Glucagon-like peptide-1; DPP-4: Dipeptidyl peptidase-4; VEGF: Vascular Endothelial Growth Factor ; KKS: Kinin–Kallikrein System; DKD: Diabetic Kidney Disease; ARBs: Angiotensin II Receptor Blockers; BP: Blood Pressure; DFU: Diabetic Foot Ulcers; ED: Erectile Dysfunction; TSH: Thyroid Stimulating Hormone; OHA: Oral Hypoglycemic Agent; HDL: High Density Lipoprotein; ESS: Epworth Sleepiness Scale; PQSI: Pittsburgh Sleep Quality Index
Introduction
Diabetes is a complex set of metabolic disorder in which the blood sugar levels are consistently raised. In most of the cases the body is either unable to produce insulin effectively or not able to effectively utilize synthesized insulin in the body or sometime a combination of both. Glucose is the source of energy for daily activities. Insulin a hormone produced by the β-cells of Islets of Langerhans of the pancreas helps glucose entre into the cells and through biochemical processes it is broken into usable energy forms- adenosine triphosphate (ATP) [1].
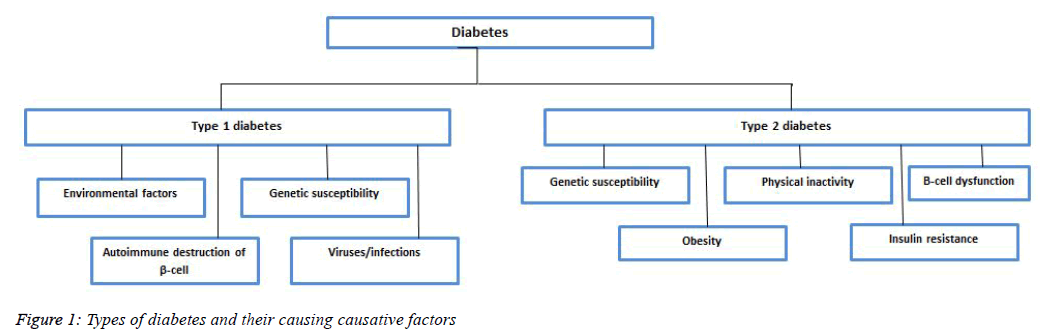
Diabetes is basically of two types namely- Type1 diabetes and Type 2 diabetes (Figure 1). Type 1 diabetes is caused by lack of insulin production due to destruction of insulin producing β- cells (Islets of Langerhans) in the pancreas. Thus, it is also referred to as insulin dependent diabetes mellitus. Type 2 diabetes is commonest form of diabetes. It is caused by a combination of factors including insulin resistance, in which the body is unable to use the insulin effectively. Type 2 diabetes develops when the body is unable to compensate for the impaired ability to use insulin. Sometimes it is also referred to as insulin independent diabetes mellitus. Apart from the two-basic type of diabetes, gestational diabetes is also reported in women during pregnancy [2].
According to the report of WHO, the number of people with diabetes rose from 108 million in 1980 to 422 million in 2014 [3]. The worldwide number of adults with diabetes mellitus is projected to double during the next 2 decades from 135 million in 1995 to more than 300 million by 2025, and the majority of cases are reported in developed countries [4]. Persistent high blood sugar level can be hazardous to health. Although diabetes has no permanent cure, several steps can be taken to manage diabetes and to maintain a healthy life.
Complications and Comorbidities of Diabetes
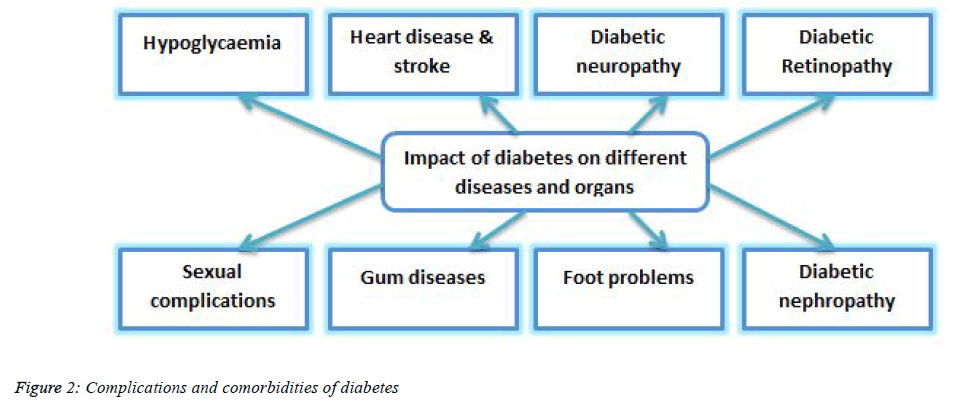
Diabetes is a complex set of metabolic disorder and has its impact on different organs and diseases (Figure 2) [5-9]. Apart from being a deadly disease, diabetes is responsible for causing various complications related to different parts of the body such as nerve, heart, foot, eye, gum and sexual dysfunction (Table 1). In most of the cases, life style management plays an important role in preventing them, several novel therapies are also being investigated for the treatment [10,11].
| Complication type | Distinguishing symptoms | Diagnosis | Therapy/Treatment |
|---|---|---|---|
| Cardiovascular disease | Chest pain, heartburn, shortness of breath, excessive sweating, nausea, vomiting, tiredness | Chest radiography, electrocardiography, echocardiography, catheterization, MRI | Blood pressure management, blood glucose monitoring, individualization of medication |
| Nephropathy | Inconsistent blood pressure, presence of protein in urine, loss of appetite, nausea, vomiting | Blood test, urine test, imaging test, renal function test, kidney biopsy | Management of blood sugar and hypertension, Angiotensin- converting enzyme (ACE) inhibitors like captopril, enalapril, lisinopril, and ramipril are the first line drugs for the treatment. |
| Neuropathy | loss of sensation in various parts such as hands, arms, feet, and legs | physical examinations like filament test, quantitative sensory testing, nerve conduction studies, electromyography, autonomic testing | Management of blood glucose level, proper diet, exercise and cessation of smoking, anti-seizure drugs like pregabalin, gabapentin, carbamazepine and antidepressants like desipramine, imipramine is also included in the therapy for relief from the pain |
| Retinopathy | Floaters, distortion, and/or blurred vision | dilated eye examination, fluorescein angiogram and ocular coherence tomography (OCT) | Management of blood glucose and blood pressure levels, laser surgery, treatment with corticosteroid-releasing implants, Aflibercept, bevacizumab, ranibizumab etc. |
| Sleep apnea | Periodic breathing, respiratory abnormality | Patient history and physical examination, polysomnogram | Good sleep hygiene, cognitive behavioral therapy, sleep restriction and relaxation therapies, medications like: anti-parkinsonian drugs (dopamine agonists) like levodopa, carbidopa, bromocriptine mesylate etc., benzodiazepines like lorazepam, clonazepam, diazepam etc., non-benzodiazepine like zolpidem, eszopiclone etc., opiates, like codeine, oxycodone, methadone etc., are often prescribed to the patient with sleep disorders |
| Thyroid dysfunction | Nervousness and tremor, mental mental fogginess, m menstrual changes, mweight gain, m high cholesterol levels | Sensitive serum thyroid stimulating hormone assay | Thyroid hormone analogues, L-thyroxine are the most widely used thyroid hormone replacement. |
| Sexual dysfunction | Inability to maintain firm erection | Careful examination of penis and testicles and checking your nerves for sensation, blood tests | Treatment can be done by drugs and changes in the life style and daily routine habits, various oral therapies available in the treatment of the ED: sildenafil citrate, tadalafil and vardenafil |
| Pancreatitis | Upper abdominal pain, Oily, smelly stools (steatorrhea), Weight loss | Blood test, stool test, computerized tomography (CT) scan to look for gallstones, abdominal ultrasound | Management of the disease is usually based on first line therapy to control the hyperglycemic condition of the patient, metformin, glipizide, glebenclamide are some of the first line treatment strategy to control high blood glucose level |
| Diabetic foot ulcer | Swelling, discoloration, foul-smelling discharge seeping from wound, fever and chills | Nylon monofilament test, transcutaneous oxygen measurement, ankle-brachial index, absolute toe systolic pressure | Offloading the wound, daily saline dressings, debridement, antibiotic therapy |
| Vitamin D insufficiency | Malaise and deficient immune system, chronic pain, depression, hair loss, weakness | Testing vitamin D levels through blood test | Dietary supplements rich in vitamin D may help in management of type 2 diabetes. Diabetes is a dietary disorder which may be reversed with the help of holistic diet and health and active life style |
Table 1: Etiology, diagnosis and treatment methods for different diabetes complications
Rate of mortality has decreased in the recent times however, with the growing population and altered life style, rate of people being diagnosed with diabetes has increased enormously. Diabetes has diversified and mostly effecting people in the middle and lower income countries [9,12].
Cardiovascular Complications
Diabetes has its impact on cardiovascular system and may provoke stroke and other cardiac disorders. It is usually seen that patients with type 2 diabetes are prone to congestive heart failure. Chronic hyperglycemia is one of the factors which may cause cardiomyopathy; apart from that other factors which influence the disease are severe coronary atherosclerosis, prolonged hypertension [13], micro vascular disease, glycosylation of myocardial proteins, and autonomic neuropathy. Glycemic control, better control of hypertension and prevention of atherosclerosis may help in the management of cardiomyopathy [14].
Diabetes mellitus is not merely a disorder of carbohydrate metabolism; it also influences vascular diseases affecting nearly all type and sizes of blood vessel. Complications in vascular system are responsible for the morbidity and death of patients with diabetes mellitus [15,16].
Other cardiovascular diseases which are influenced by diabetes are coronary artery disease, peripheral arterial disease, and stroke. Diabetes is also the main cause of the various macrovascular complications such as diabetic nephropathy, neuropathy, and retinopathy [17] (Table 2). Hyperglycemia and insulin resistance are the two-major causes of cardiovascular complications. The linkage between diabetes mellitus and macrovascular disease was first studied about 40 years ago which has reported the risk of myocardial infarction (MI) and cardiovascular deaths in different populations [18].
| Complications | Factors |
|---|---|
| Microvascular complications | |
| Retinopathy | ↑ blood glucose, ↑ blood pressure damages blood vessels leading to retinopathy, cataracts and glaucoma. |
| Nephropathy | ↑ blood pressure damages blood vessels and ↑ blood glucose makes the kidney to overwork resulting in nephropathy. |
| Neuropathy | ↑ blood glucose cause injury to nerves mostly in the legs and feet region. This may remain undetected and lead to gangrene. |
| Macrovascular complications | |
| Cerebro-vascular | ↑ blood glucose cause increased risk of cerebrovascular disease and cognitive impairement. |
| Cardio-vascular | ↑ blood glucose, ↑ blood pressure and insulin resistance causes higher risk of coronary heart disease. |
| Peripheral vascular | ↑ blood glucose results in narrowing of the blood vessels, ↓ blood flow to the peripheral parts leading to slow healing process in the feet wound and eventually leading to gangrene. |
| ↑ represents increased; ↓ represents decreased | |
Table 2: Micro-vascular and macro-vascular complications of diabetes
Both type 1 and type 2 diabetes are associated with different types of risk in different population. The Nurses’ Health Study comprising comprising of 116, 316 women aged between 30 to 55 years and followed up for 26 years concluded that type 1 diabetes mellitus was associated with increased risk of both ischemic and hemorrhagic strokes, whereas type 2 diabetes mellitus increased the risk of ischemic stroke, but hemorrhagic stroke was not associated with type 2 diabetes [19].
Better understanding of the mechanism of the disease can assist clinicians in dealing with cardiovascular diseases in patients with diabetes and could help in lessening the devastating complications [20].
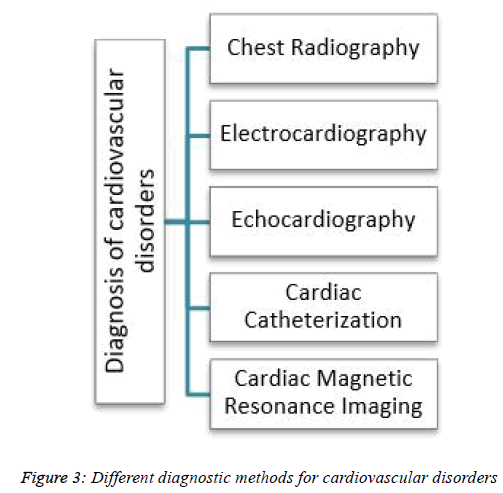
Heart failure is a serious condition with high prevalence. The cost associated with the treatment of the disease is also very high. A powerful sickness control approach with analysis of massive quantity of information, early detection of the sickness, evaluation of the severity and early prediction of damaging activities may help in inhibiting the progression of the disease. It will subsequently improve the quality of life of the patients and will help in reducing the associated medical costs [21,22]. There are some of the common methods that have been used for the diagnosis of most of the cardiovascular diseases (Figure 3) [23,24].
There are various treatment methods available for the diabetic heart disease (DHD). It can be managed by the controlling some of the factors such as blood glucose level. Cardiovascular diseases contribute to higher mortality rate in diabetic patients which is a matter of concern. Various risk factors including hypertension, obesity and dyslipidemia also add up to cardiovascular risk factors among diabetes patients. Risks factors targeted therapies are needed to improve the condition of patients [25].
Management of Type 2 diabetes includes moderate weight loss (~7% of body weight). It improves blood glucose levels, and also positively impact blood pressure and cholesterol levels in the body [26]. Individualization of medication is the key for managing cardiovascular complications associated with diabetes. Incretin-based therapies, Dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide-1 (GLP-1) receptor agonists are some of the newer medicinal approaches for the management of cardiovascular complications associated with diabetes.
Diabetic Neuropathy
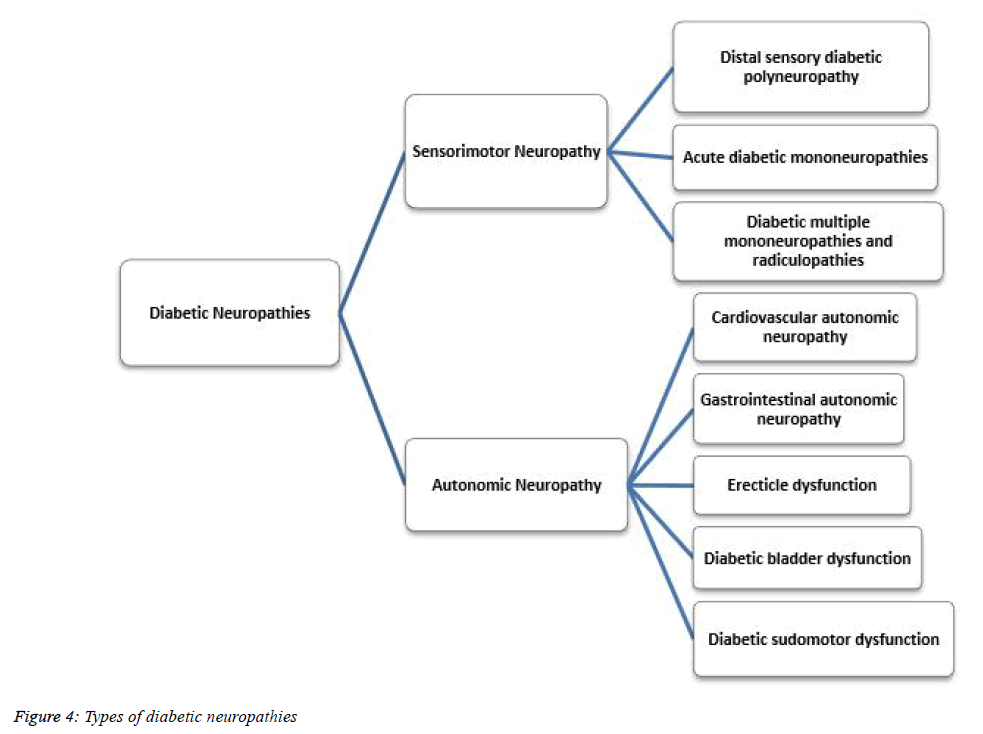
Neurons transmit signals to various parts of the body. Due to the damage of nerve cells caused by both forms of diabetestype 1 and type 2 is associated with various neurological disorders which are together called as diabetic neuropathy. High blood glucose level can cause injury to nerves mostly in the legs and feet region. There are basically two types of diabetic neuropathies (Figure 4) [27].
• Sensorimotor neuropathies
• Autonomic neuropathies
Symptoms of diabetic neuropathy include loss of sensation in the various parts such as hands, arms, feet, and legs. It is thought to affect 1.9% of the world’s population.
Diagnosis of the disease is mostly based on physical examinations like filament test, quantitative sensory testing, nerve conduction studies, electromyography, autonomic testing etc. [27].
Treatment strategy includes management of the diabetes, keeping blood glucose level under control which may help in slowing down of the disease progression. Proper diet, exercise and cessation of smoking help a lot in keeping the disease under control [28-30]. Anti-seizure drugs like pregabalin, gabapentin, carbamazepine and antidepressants like desipramine, imipramine is also included in the therapy for relief from the pain [31].
Diabetic Retinopathy
Among the complications of diabetes (type 1 and type 2), diabetic retinopathy is one of the major one. High blood sugar levels damage the blood vessels of retina, eventually leading to retinopathy [32]. The over-production of a protein called vascular endothelial growth factor (VEGF) is another major cause of retinopathies. Lack of oxygen or hypoxic condition causes more production of VEGF, which in turn stimulates the growth of additional blood vessels in eye, a process which is highly beneficial in hearts but has a contrary effect in eye. The abnormal blood capillaries do not occur in the retina, but it grows in the vitreous region in diabetic retinopathy. Diabetic retinopathy can be managed by controlling the blood glucose and blood pressure levels. Anti-VEGF” medication is another approach for managing retinopathy [33]. In spite of being a novel approach, anti-VEGF fails in a considerable number of patients. Several new therapies are being developed for the treatment of the disease such as corticosteroid-releasing implants, which may be particularly useful in pseudophakic patients, and treatments targeting kinin–kallikrein system (KKS) [34]. Aflibercept, bevacizumab, ranibizumab are some of the FDA approved medication which are capable of reducing macular oedema.
Laser surgery is also exploited for the treatment of the eye diseases. It has proven that laser therapy reduces the risk of severe visual loss by >50% in eyes with high-risk characteristics and may also be beneficial in diabetic retinopathy [35].
Vitrectomy, a surgery in which the Vitreous Humor Gel is removed to provide higher access to the retina is another novel approach for the management of retinopathy. After the surgical operation, saline, silicone oil may be injected into the vitreous gel which will assist to keep the retina functional. Vitrectomy brings significant improvement in the visual outcome [36,37].
Hypoglycemia
Hypoglycemia is a condition, in which excess production of insulin causes low levels of blood sugar. Anti-hyperglycemic agents increase insulin in the body and due to the increased levels of insulin, blood sugar level gets too low. Hypoglycemia also occurs by skipping meals, eating less than normal and excess medication [38]. Symptoms of hypoglycemia includessweating, heart palpitations, shaking, dizziness, hunger, confusion, drowsiness, speech difficulty, odd behavior and incoordination [39].
The patients having diabetes along with chronic kidney disease have a higher frequency of hypoglycemia than the people who are having diabetes but devoid of chronic kidney disease. It was observed in a retrospective analysis involving more than 200,000 patients that the rate of hypoglycemia was approximately twice as high in diabetic patients with chronic kidney disease (glomerular filtration rate <60 mL/min per 1.73 m2) than those without chronic kidney disease (glomerular filtration rate ≥60 mL/min per 1.73 m2) [40,41]. Reasons for this increased risk include reduced insulin requirements because of decreased renal clearance of insulin, decreased degradation of insulin in peripheral tissues, reduced renal gluconeogenesis and prolonged half-life of other drugs in chronic kidney disease. In a study conducted on rat model, hyperglycemia was observed in diabetic pregnant rats due to increased gluconeogenesis [42,43].
Elderly patients are at higher risk of hypoglycemia. Deteriorating renal function affects the drug clearance, leading to drug depot in the body, adverse interactions and decrement in the cognitive functioning. Glycemic thresholds at which counter-regulatory responses to hypoglycemia occur are lowered in elderly persons (e.g., <2.0 mmol/L [36 mg/dL]) decreasing potential reaction time for corrective action and increasing the risk for asymptomatic hypoglycemia [44-46].
Elder adults with diabetes are having a higher risk for hypoglycemia due to altered adaptive physiologic responses to low glucose levels [47]. Hypoglycemia prevention is an important part of diabetes mellitus management and strategies include patient education, glucose monitoring, appropriate adjustment of diet and medications in relation to everyday circumstances including physical exercise, and the application of new technologies such as real-time continuous glucose monitoring, modified insulin pumps and the artificial pancreas [48].
Diabetic Nephropathy
Diabetic nephropathy is defined as the damage caused to the kidney by the high blood sugar due to diabetes [49]. Diabetic kidney disease (DKD), the most frequent and dangerous complications of diabetes affects about one-third of the patients with diabetes. Both forms of diabetes type 1 and type 2 may lead to nephropathic condition of kidney. In addition to the other organs, kidneys also play an important role in glycemic control, particularly due to renal contribution to gluconeogenesis and tubular reabsorption of glucose [50]. Diabetes is the leading cause of end-stage renal disease (ESRD) [51].
Medical screening program is encouraged to recognize a disease in its early phase so that intervention can occur at preclinical stages which ultimately lead to better outcomes. Screening programs may also promote public awareness and education and serve as medical outreach to underserved populations. Such programs have certain factors such as benefits, risks, and costs. For a screening program to be beneficial, it should fulfill several criteria [52-54].
Angiotensin-converting enzyme (ACE) inhibitors like captopril, enalapril, lisinopril, and ramipril are the first line drugs for the treatment. These inhibitors have the potential to lower the amount of protein in the urine and also reduce the risk of cardiovascular diseases [55].
Angiotensin II receptor blockers (ARBs), such as candesartan cilexetil, irbesartan, losartan potassium, and telmisartan [56] are another class of drug having potential to treat diabetic nephropathy. However, these conventional dosage forms undergo extensive first pass metabolism which reduces their bioavailability. Transdermal delivery has gained a significant importance for treatment of the hypertension due to their availability to avoid first pass metabolism [57]. Diabetic nephropathy was categorized into stages: micro albuminuria and macro albuminuria. Microalbuminuria screening should be performed yearly [58]. Patients with micro and macro albuminuria should undergo an evaluation to check the presence of comorbid associations [59].
Glycemic control is essential to delay or prevent the onset of DKD. There are a number of glucose-lowering medications available in the market but only a fraction of them can be used safely in chronic kidney disease and many of them need proper dosing adjustment [60].
Many factors initiate or promote DKD. Initiators of DKD include hyperglycemia and altered expression of certain genes. Promoters of the disease include hyperglycemia, hypertension, dyslipidemia, smoking, ethnicity, sex, age, and a long diabetes duration [61-64].
Blood pressure (BP) control is generally recommended to prevent stroke, cardiovascular disease, and albuminuria.10 mmHg decrease in systolic BP was associated with reduced levels of diabetic microvascular complications, including nephropathy [65,67]. Angiotensin II receptor blockers (ARBs) or angiotensin-converting enzyme (ACE) inhibitors are recommended to control BP with nephrological symptoms [68]. Many novel medications like mineralocorticoid receptor antagonists, endothelin receptor antagonists are being investigated for DKD.
Diabetes and Foot
Diabetic foot disease is a complication of diabetes mellitus, affecting up to 50% of patients with both type 1 and 2 diabetes. It can be classified into neuropathic foot and ischaemic foot. Neruopathic foot is characterized by neuropathic ulcers, charcot joint and neuropathic oedema while in ischemic foot atherosclerosis is the predominant factor leading to the disease [69,70].
Current available treatments for diabetic foot disease are usually not as effective as they should be. This is due to the insufficient knowledge of its underlying mechanisms and treatment tools which may be due to lack of interest and research resources allocated to the study of this complication worldwide [71].
Unfortunately, often patients are in denial of their disease and fail to take ownership of their illness along with the necessary steps to prevent complication and to deal with the many challenges associated with the management of diabetic foot ulcers (DFU). However, numerous studies have shown that proper management of DFU can greatly reduce, delay, or prevent complications such as infection, gangrene, amputation, and even death [72,73].
Diabetes and Gums
Periodontitis is a common chronic inflammatory disease which is characterized by destruction of the supporting structures of the teeth (the periodontal ligament and alveolar bone). It is highly prevalent with severe periodontitis affecting 10–15% of adults and has multiple negative impacts on quality of life [74-76].
It has been suggested that there is a threefold higher risk in people with diabetes (type 1 as well as type 2) to develop periodontitis. However, a clear mechanism to relate these two conditions is still not completely understood [74].
Apart from periodontal and gingival inflammation, diabetes is often also related to other oral complications like xerostomia, dental caries, candida infections, burning mouth syndrome etc [74].
Most of the treatment strategies include elimination of infection either through removal of plaque or calculus or through maintaining the glycemic level. Apart from that, overthe counter antibacterial rinses are also often prescribed to decrease the bacterial load and assist in gum healing. Chlorhexidine is one of the most commonly used oral rinses [74].
Sexual Dysfunction
Diabetes is known to cause multiple medical, psychological, and sexual dysfunctions. Impaired sexual function in men is a well-documented complication of diabetes. Type 2 diabetes has been linked to erectile dysfunction in many research studies [77].
Diabetes is an established risk factor for sexual dysfunction [78,79] in men, a threefold increased risk of erectile dysfunction (ED) was documented in diabetic men as compared with non-diabetic men. Erectile dysfunction is the inability to maintain firm erection for enough period of time to have a successful sexual intercourse. Damage to nerve and blood vessels due to poor long term blood glucose level is the stem cause of ED [79].
The adoption of healthy lifestyles may reduce insulin resistance, endothelial dysfunction, and oxidative stress – all of which are desirable achievements in diabetic patients. Improved well-being may further contribute to reduce and prevent sexual dysfunction in both sexes [80]. It can be cured by various treatments. There are recent advances in the sciences which help in coping up with the disease [81]. Treatment can be done by drugs and changes in the life style and daily routine habits [81]. Various oral therapies available in the treatment of the ED include sildenafil citrate, tadalafil and vardenafil (Levitra) etc. [82].
Diabetes and Sleep
Sleep difficulties are more common in people who have diabetes than in people who don’t. Sleep disorders have a vice versa effect on diabetes as person with diabetes are more likely to develop sleep disorder and loss of sleep (insomnia) may exacerbate the symptoms of diabetes. It is mostly associated with type 2 diabetes [77]. Sleep apnea is one of the most common sleep disorder associated with diabetes.
Sleep apnea is a condition in which breathing repeatedly stops and starts throughout the night. In another study it was concluded that diabetes is associated with periodic breathing, a respiratory abnormality that is associated with abnormalities in the central control of ventilation. Some sleep disturbances may result from diabetes through the deleterious effects of diabetes on central control of respiration [83].
Majority of sleep disorders is diagnosed based on patient history and physical examination. Polysomnogram is also exploited for proper diagnosis of sleep apnea. Management of sleep disorder requires a multi-level approach which includes adherence to good sleep hygiene, cognitive behavioral therapy, sleep restriction and relaxation therapies. Apart from the behavioral approach for managing sleep disorders certain medications like: Anti-parkinsonian drugs (dopamine agonists) like levodopa, carbidopa, bromocriptine mesylate etc., benzodiazepines like lorazepam, clonazepam, diazepam etc., Non-benzodiazepine like zolpidem, eszopiclone etc., Opiates, like codeine, oxycodone, methadone etc., are often prescribed to the patient with sleep disorders. However, it is necessary to inform the doctor about the current diabetic medication a patient is receiving to avoid adverse drug reaction and possible side effects [68].
Diabetes and Thyroid
Along with various disease complications such as diabetic nephropathy, diabetic retinopathy etc. diabetes is also associated with abnormal functioning of thyroid and vice versa [84]. Type 2 diabetes is mostly associated with thyroid dysfunction. In a study by Bhat et al. [85] it was concluded that there are chances of abnormal thyroid function in critical ill patients. The study calculated levels of Serum free triiodothyronine (fT3), free tetraiodothyronine (fT4) and TSH (Thyroid Stimulating Hormone). Low fT3 level was the most common abnormality found in the subjects during the course of the study [85]. In another study it was found that there is significant decrement in the levels of iron and ferritin in patients of hypothyroidism [86,87].
The physiological understanding of correlation between type 2 diabetes and thyroid dysfunction is attributed to genetic expression, impaired glucose utilization, insulin resistance etc. Hyper and hypothyroidism is also associated with insulin resistance and is one of the major causes of impaired glucose metabolism in type 2 diabetes. Regular screening for thyroid abnormalities in diabetic patient is important for early diagnosis and proper management of the disease. Currently sensitive serum thyroid stimulating hormone assay is the first line screening test for the disease [86].
Management of the disease is usually done through thyroid hormone analogues. However, thyroid hormone analogues come with deleterious effects on muscles, bones and heart. Lthyroxine is the most widely used thyroid hormone replacement [87].
Diabetes and Pancreas
Diabetes both the form type 1 and type 2 gradually affects the pancreas. Continuous high blood glucose level creates a toxic environment for the beta cells of the pancreas and adversely impacting their insulin producing capacity. In other cases usually in type 1 diabetes, beta cells become completely incapable of producing insulin due to their reactions with immune defenses of the body. In a hospital-based study by it was found that all types of diabetes are associated with the fatty pancreas. Variables that were included in the study were age, gender, HbA1c, serum creatinine, fasting blood glucose. Fatty pancreas can be an indication for newly diagnosed diabetes [88].
Due to diabetes, pancreas may also get injured. In a study for correlation of type 2 diabetes and pancreatitis, three groups were categorized: healthy controls, prediabetes, and diabetes. After the statistical analysis it was found that the level of serum lipase was elevated in Type 2 diabetes which indicates that serum lipase is a major cause of pancreatitis [89]. Diabetes may also lead to pancreatic cancer and vice versa.
The management of the disease is usually based on first line therapy to control the hyperglycemic condition of the patient. Metformin, glipizide, glebenclamide are some of the first line treatment strategy to control high blood glucose level. Newer medications like gliptins class of drugs are also an important part of the treatment strategy. However, life style management plays a pivotal role for maintaining a healthy life of diabetic patients. In severe condition insulin therapy and surgery are also considered [89].
Diabetes and Levels of Vitamin D and Good Cholesterol
Many researchers suggest that vitamin D deficiency is associated with type 2 diabetes, cardiovascular diseases, cancers etc. It is hypothesized that low serum 25- hydroxyvitamin D3 [25(OH)D3] concentrations with type 2 diabetes may be mediated through glucose homeostasis or is the outcome of a direct effect of vitamin D on the beta cell function and insulin resistance [90].
In another study conducted with three groups: OHA group (oral hypoglycemic agent), insulin taking group and control group. It was found that the levels of 25(OH) was affected due to the diabetes. The levels of 25(OH) was highest in the control group followed by the OHA group and least in the insulin taking group. It concluded that diabetes is affecting all the major organs and has a major role in various dysfunctions. Diabetic people have significantly low plasma HDL compared to the non-diabetic people [90,91].
In a study conducted on type 2 diabetic patients in elderly group. Various measures were evaluated such as Epworth Sleepiness Scale (ESS) and Pittsburgh Sleep Quality Index (PSQI). It was concluded in the study that the low vitamin levels and disorders in sleep have an effect on the HbA1c levels [92].
Dietary supplements rich in vitamin D may help in management of type 2 diabetes. Since, diabetes is a dietary disorder which may be reversed with the help of holistic diet and health and active life style.
Conclusion
Even though several medications are available for symptomatic treatment of diabetic complications, there is always a chance of reoccurrence. Therefore, dietary regulation and monitoring of blood glucose level seems to be the most effective way to prevent any further complications. Regular physical activity or exercise is known to confer the entry of glucose into the muscle cells by an alternate mechanism similar to that facilitated by insulin, thus normalizing hyperglycaemia. Cardiovascular disease is the single largest cause of mortality worldwide with dietary causes. Therefore, immediate attention needs to be given for any symptoms associated with cardiovascular complication arising out of diabetes. Apart from that diabetes in both forms (type 1 and type 2) was either found to be influenced by other diseases or other pathological conditions were found to modulate diabetic condition. Type 1 and type 2 diabetes may provoke pathological complications like neuropathy, retinopathy, and nephropathy. Subjects with type 2 diabetes have also reported for foot and gum problems. Sexual dysfunction is another major complication of diabetes mostly in the form of erectile dysfunctioning in men. Apart from males, diabetes also influences the sexual life of females. The disease also has a modulatory effect on sleep cycle of the patients. Most of the patients with diabetes usually complains about insomnia (sleeplessness or too much of sleep). Thyroid gland is one of the major endocrine gland. Type 2 diabetes is mostly associated with thyroid dysfunction. Many researchers suggest that vitamin D deficiency is associated with type 2 diabetes, cardiovascular diseases, cancers etc. It is hypothesized that low serum 25-hydroxyvitamin D3 [25(OH)D3] concentrations with type 2 diabetes may be mediated through glucose homeostasis or is the outcome of a direct effect of vitamin D on β-cell function and insulin resistance. This review briefly summarizes the pathological comorbidities that may arise due to diabetes. In most of the cases, management of the disease is based on life style modulation with some first line medication to control the glucose level. Apart from that, other complications which may arise as comorbidity is treated separately with their specific first line of treatment. In the coming years, we believe that clinicians will come up with better understanding of the disease and with optimized and advanced treatment strategies, the disease can be handled in a more comprehensive manner.
References
- Williams G, Pickup JC. Handbook of diabetes. Wiley-Blackwell. 2004.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33:62.
- Tuso P. Prediabetes and lifestyle modification: time to prevent a preventable disease. Permanente J. 2014;18:88.
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414-1431.
- Fowler MJ. Microvascular and macrovascular complications of diabetes. Clin Diabetes 2008;26:77-82.
- Min TZ, Stephens MW, Kumar P, Chudleigh RA. Renal complications of diabetes. Brit Med Bulletin. 2012;104.
- Scott GI. Ocular complications of diabetes mellitus. Brit J Ophthalmol. 1953;37:705.
- Al-Rubeaan K, Al Derwish M, Ouizi S, Youssef AM, Subhani SN, Ibrahim HM, Alamri BN. Diabetic foot complications and their risk factors from a large retrospective cohort study. PloS One. 2015;10:e0124446.
- Al-Maskari AY, Al-Maskari MY, Al-Sudairy S. Oral manifestations and complications of diabetes mellitus: a review. Sultan Qaboos Univ Med J. 2011;11:179.
- Papazoglou D, Edmonds M. Complications of diabetes. J Diabetes Res 2016;6989453.
- Henry WL. The complications of diabetes mellitus. J Natl Med Assoc. 1987;79:677-680.
- Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endocrinol. 2016;4:537-547.
- Cryer PE, Axelrod L, Grossman AB, Heller SR, Montori VM, Seaquist ER, Service FJ. Evaluation and management of adult hypoglycemic disorders: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2009;94:709-728.
- Resnick HE, Howard BV. Diabetes and cardiovascular disease. Annual Rev Med. 2002;53:245-267.
- Creager MA, Luscher TF, Cosentino F, Beckman JA. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: Part I. Circulation. 2003;108:1527-1532.
- The American Heart Association. Diabetes mellitus: A major risk factor for cardiovascular disease circulation. Circulation. 1999;100:1132-1133.
- Huang D, Refaat M, Mohammedi K, Jayyousi A, Al Suwaidi J, Abi Khalil C. Macrovascular complications in patients with diabetes and prediabetes. BioMed Res Int. 2017;2017.
- Beckman JA, Creager MA. Vascular complications of diabetes. Circ Res. 2016;118:1771-1785.
- Janghorbani M, Hu FB, Willett WC, Li TY, Manson JE, Logroscino G, Rexrode KM. Prospective study of type 1 and type 2 diabetes and risk of stroke subtypes: the Nurses’ Health Study. Diabetes Care. 2007;30:1730-1735.
- Dokken BB. The pathophysiology of cardiovascular disease and diabetes: beyond blood pressure and lipids. Diabetes Spectrum. 2008;21:160-165.
- Pappachan JM, Varughese GI, Sriraman R, Arunagirinathan G. Diabetic cardiomyopathy: Pathophysiology, diagnostic evaluation and management. World J Diabetes. 2013;4:177.
- Tripoliti EE, Papadopoulos TG, Karanasiou GS, Naka KK, Fotiadis DI. Heart failure: diagnosis, severity estimation and prediction of adverse events through machine learning techniques. Comput Structural Biotechnol J. 2017;15:26-47.
- Maganti K, Rigolin VH, Sarano ME, Bonow RO. Valvular heart disease: diagnosis and management. InMayo Clin Proceedings. 2010;85:483-500.
- Hayat SA, Patel B, Khattar RS, Malik RA. Diabetic cardiomyopathy: mechanisms, diagnosis and treatment. Clin Sci. 2004;107:539-557.
- Leon BM, Maddox TM. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes. 2015;6:1246.
- Jahangir MA, Imam SS, Kazmi I. Type 2 diabetes current and future medications: a short review. Int J Pharm Pharmacol. 2017;101.
- Deli G, Bosnyak E, Pusch G, Komoly S, Feher G. Diabetic neuropathies: diagnosis and management. Neuroendocrinology. 2013;98:267-280.
- Uppari DJ. A short note on diabetic neuropathy-diagnostic and therapeutic approach. RRJHMS. 2015;4:2015.
- Sigal RJ, Kenny GP, Wasserman DH, Castaneda-Sceppa C. Physical activity/exercise and type 2 diabetes. Diabetes Care. 2004;27:2518-2539.
- Thent ZC, Das S, Henry LJ. Role of exercise in the management of diabetes mellitus: the global scenario. PloS One. 2013;8:e80436.
- Javed S, Petropoulos IN, Alam U, Malik RA. Treatment of painful diabetic neuropathy. Therap Advances Chronic Dis. 2015;6:15-28.
- Nentwich MM, Ulbig MW. Diabetic retinopathy-ocular complications of diabetes mellitus. World J Diabetes. 2015;6:489.
- Yorston D. Anti-VEGF drugs in the prevention of blindness. Community Eye Health. 2014;27:44.
- Bolinger MT, Antonetti DA. Moving past anti-VEGF: novel therapies for treating diabetic retinopathy. Int J Mol Sci. 2016;17:1498.
- Neubauer AS, Ulbig MW. Laser treatment in diabetic retinopathy. Ophthalmologica. 2007;221:95-102.
- Charles S. Vitrectomy techniques for complex retinal detachments. Taiwan J Ophthalmol. 2012;2:81-84.
- Smiddy WE, Flynn HW. Vitrectomy in the management of diabetic retinopathy. Survey Ophthalmol. 1999;43:491-507.
- Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care. 2003;26:1902-1912.
- Kalra S, Mukherjee JJ, Venkataraman S, Bantwal G, Shaikh S, Saboo B, Das AK, Ramachandran A. Hypoglycemia: The neglected complication. Indian J Endocrinol Metab. 2013;17:819.
- Levey AS, Becker C, Inker LA. Glomerular filtration rate and albuminuria for detection and staging of acute and chronic kidney disease in adults: a systematic review. JAMA. 2015;313:837-846.
- Moen MF, Zhan M, Walker LD, Einhorn LM, Seliger SL, Fink JC. Frequency of hypoglycemia and its significance in chronic kidney disease. Clin J Am Soc Nephrol. 2009;4:1121-1127.
- Abraham P, Rabi S, Francis DV, Natarajan K, Amaladass A. Increased hepatic gluconeogenesis and decreased glucose uptake, and increased hepatic de novo lipogenesis in rat model of maternal diabetes. Biomed Res. 2016;27.
- American Diabetes Association. Economic costs of diabetes in the US in 2012. Diabetes Care. 2013;36:1033-1046.
- Parthasarathi D, Gajendra C, Dattatreya A, Sree Venkatesh Y. Analysis of pharmacokinetic and pharmacodynamic models in oral and transdermal dosage forms. J Bioequiv Availab. 2011;3:268-276.
- Sai YRKM, Dattatreya A, Anand SY, Suresh Babu D, Sandeep Heni RS. Biomarkers of internal origin and their significance in diabetes and diabetic complications. J Diabetes Metab. 2011.
- Adapa D, Sarangi TK. A Review on diabetes mellitus: complications, management and treatment modalities. J Med Health Sci. 2015;4.
- Sircar M, Bhatia A, Munshi M. Review of hypoglycemia in the older adult: clinical implications and management. Canadian J Diabetes. 2016;40:66-72.
- Frier BM. Hypoglycaemia in diabetes mellitus: epidemiology and clinical implications. Nature Rev Endocrinol. 2014;10:711.
- Ayodele OE, Alebiosu CO, Salako BL. Diabetic nephropathy-a review of the natural history, burden, risk factors and treatment. J Natl Med Assoc. 2004;96:1445.
- Pecoits-Filho R, Abensur H, Betônico CC, Machado AD, Parente EB, Queiroz M, Salles JE, Titan S, Vencio S. Interactions between kidney disease and diabetes: dangerous liaisons. Diabetol Metab Syndrome. 2016;8:50.
- Kramer H, Molitch ME. Screening for kidney disease in adults with diabetes. Diabetes Care. 2005;28:1813-1816.
- Jaar BG, Khatib R, Plantinga L, Boulware LE, Powe NR. Principles of screening for chronic kidney disease. Clin J Am Soc Nephrol. 2008;3:601-609.
- King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414-1431.
- Kramer H. Screening for kidney disease in adults with diabetes mellitus: Don’t forget serum creatinine. Am J Kidney Dis. 2004;44:921-923.
- Kumar S, Dietrich N, Kornfeld K. Angiotensin converting enzyme (ACE) inhibitor extends Caenorhabditis elegans Life Span. PLoS Genet. 2016;12:e1005866.
- Barreras A, Gurk-Turner C. Angiotensin II receptor blockers. InBaylor Univ Med Center Proceedings. 2003;16:123-126.
- Ahad A, Al-Mohizea AM, Al-Jenoobi FI, Aqil M. Transdermal delivery of angiotensin II receptor blockers (ARBs), angiotensin-converting enzyme inhibitors (ACEIs) and others for management of hypertension. Drug Delivery. 2016;23:579-590.
- Haneda M, Utsunomiya K, Koya D, Babazono T, Moriya T, Makino H, Kimura K, Suzuki Y, Wada T, Ogawa S, Inaba M. A new classification of diabetic nephropathy 2014: a report from Joint Committee on Diabetic Nephropathy. J Diabetes Invest. 2015;6:242-246.
- Gross JL, De Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care. 2005;28:164-176.
- Hahr AJ, Molitch ME. Management of diabetes mellitus in patients with chronic kidney disease. Clin Diabetes Endocrinol. 2015;1:2.
- Sridevi P, Budde P, Neeraja T, Bhagavan Raju M, Adapa D. Anti-oxidants and their role in disease management. Int J Med Res Health Sci. 2018;7:175-190.
- Choudhury A, Chakraborty I, Banerjee TS, Vana DR, Adapa D. Efficacy of Morin as a potential therapeutic phytocomponent: insights into the mechanism of action. Int J Med Res Health Sci. 2017;6:175-194.
- Choudhury A, Bhattacharjee R, Adapa D, Chakraborty I, Banerjee TS, Vana DR. Understanding the role of resveratrol in major neurological and lifestyle diseases: an insight into molecular mechanisms and druggability. Pharm Bioprocess 2018;6:064-083.
- Prasad VSS, Hymavathi A, Babu VR, Longvah T. Nutritional composition in relation to glycemic potential of popular Indian rice varieties. Food Chemistry. 2018;238:29-34.
- Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, Wright AD, Turner RC, Holman RR. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321:412-419.
- Garg A, Vaya RK, Chaturvedi H. Effect of herbal medicine “diabetocure” on clinical and biochemical parameters of diabetes. Int J Pharm Pharmacol. 2017;1:120.
- Pothamsetty A, Janarthan M, Faheemuddin M. Evaluation of anti-diabetic activity of the plant leaves of Verbascum thapsus in alloxan induced diabetic rats. Int J Pharm Pharmacol. 2017;1:118.
- Kim MK. Treatment of diabetic kidney disease: current and future targets. Korean J Internal Med. 2017;32:622.
- Faheemuddin M, Janardhan M, Hassan M. Protective effect of Cleome viscosa extract on diet induced atherosclerosis in diabetic rats. Int J Pharm Pharmacol. 2017;1:103.
- Khare J, Srivastava P, Khare J. Microbiological profile of diabetic foot ulcers-experience from a tertiary care centre in South India. Int J Gen Med Surg. 2017;1:109.
- Mauricio D, Jude E, Piaggesi A, Frykberg R. Diabetic foot: current status and future prospects. J Diabetes Res. 2016.
- Ghosh P, Mukherjee S, Hossain C. Exploring antioxidant potential of some common marketed non-steroidal anti-inflammatory drugs. Int J Pharm Pharmacol. 2017;1.
- Alharthi S, Adair M, Das C. Robot offers no advantages in Roux-En-Y gastric bypass: analysis of the NIS database. Int J Gen Med Surg. 2017;1:112.
- Preshaw PM, Alba AL, Herrera D, Jepsen S, Konstantinidis A, Makrilakis K, Taylor R. Periodontitis and diabetes: a two-way relationship. Diabetologia. 2012;55:21-31.
- Otsuka T, Hayashi Y, Sasaguri K, Kawata T. Correlation of hypothalamic activation with malocclusion: An fMRI study. Biomed Res. 2015;26.
- Jahangir MA, Bhisht P, Muheem A, Imam SS. Diabetes: pharmacological history and future management strategies. Pharm Bioprocessing. 2017;5:54-65.
- Jahangir MA, Khan R, Sarim Imam S. Formulation of sitagliptin-loaded oral polymeric nano scaffold: process parameters evaluation and enhanced anti-diabetic performance. Artificial Cells Nanomed Biotechnol. 2017;8:1-3.
- Siddiqui MA, Ahmed Z, Khan AA. Psychological impact on sexual health among diabetic patients: A review. Int J Diabetes Res. 2012;1:28-31.
- Corona G, Giorda CB, Cucinotta D, Guida P, Nada E. Sexual dysfunction in type 2 diabetes at diagnosis: progression over time and drug and non-drug correlated factors. PloS One. 2016;11:e0157915.
- Maiorino MI, Bellastella G, Esposito K. Diabetes and sexual dysfunction: current perspectives. Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy. 2014;7:95.
- Mobley DF, Khera M, Baum N. Recent advances in the treatment of erectile dysfunction. Postgraduate Med J. 2017.
- Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A. The international index of erectile function (IIEF): a multidimensional scale for assessment of erectile dysfunction. Urology. 1997;49:822-830.
- Sridhar GR, Madhu K. Prevalence of sleep disturbances in diabetes mellitus. Diabetes Res Clin Practice. 1994;23:183-186.
- Hage M, Zantout MS, Azar ST. Thyroid disorders and diabetes mellitus. J Thyroid Res. 2011;2011.
- Bhat K, Sharma S, Sharma K, Singh RK. Assessment of thyroid function in critically ill patients. Biomed Res. 2016;27.
- Dahiya K, Verma M, Dhankhar R, Ghalaut VS, Ghalaut PS, Sachdeva A, Malik I, Kumar R. Thyroid profile and iron metabolism: mutual relationship in hypothyroidism. Biomed Res. 2016.
- Ohtsuki Y, Kimura M, Lee GH, Hirokawa M. A purely trabecular follicular adenoma of the thyroid gland, harboring extraordinarily long trabeculae. Biomed Res. 2015;26.
- Gupta SP, Mittal A, Jha DK, Raj D. Association of fatty pancreas and diabetes. A case control study from Kathmandu valley. Biomed Res. 2015;26.
- Srihardyastutie A, Soeatmadji DW, Fatchiyah A. Relation of elevated serum lipase to Indonesian type 2 diabetes mellitus progression. Biomed Res. 2015.
- Bilge U, Bilgin M. A comparison of 25 (OH) vitamin D levels in patients with type 2 diabetes on oral hypoglycemic agents and insulin treatment. Biomed Res. 2016;27.
- Babikr WG, Alshahrani AS, Hamid HG, Abdelraheem AH, Shalayel MH. The correlation of HbA1c with body mass index and HDL-cholesterol in type 2 diabetic patients. Biomed Res. 2016;27.
- Keskin A, Bilge U, Kili S, Yildiz P, Bilgin M. Effects of sleep disorders and 25-OH Vitamin D levels on HbA1c levels in geriatric type 2 diabetic patients. Biomed Res. 2016;27.