Research Article - Asian Journal of Biomedical and Pharmaceutical Sciences (2022) Volume 12, Issue 88
Management and outcome of cystocele with rectocele
Bhawana Dhanvij*
Nursing Tutor, Florence Nightingale Training College of Nursing, Sawangi (M), Wardha, India
- Corresponding Author:
- Bhawana Dhanvij
Nursing Tutor
Florence Nightingale Training College of Nursing
Sawangi (M), Wardha, India
E-mail: dhanvijbhawna788@gmail.com
Received: 05-April-2022, Manuscript No. AABPS-22-59547; Editor assigned: 07-April-2022, Pre QC No. AABPS-22-59547(PQ); Reviewed: 21-April-2022, QC No. AABPS-22-59547; Revised: 18-April-2022, Manuscript No. AABPS-22-59547(R); Published: 25-April-2022, DOI:10.35841/2249-622X.88.118
Citation: Dhanvij B. Management and outcome of cystocele with rectocele. Asian J Biomed Pharmaceut Sci. 2022;12(88):118
Abstract
Introduction: A cystocele is a condition in which a portion of the bladder wall protrudes the vaginal canal is a tube that connects the uterus to the vaginal. The bulge is caused by a hole in the wall between the bladder and the vaginal canal Cystocele. Nucleus Medical Media, Inc. is a company that specializes in medical publishing. A rectocele occurs when a portion of the rectum wall bulges into the vaginal canal. The pelvic organs are separated by connective tissue. Fascia is a connective tissue that connects neighboring muscles. The bladder, vagina, and rectum are all supported by fascia and muscles. Cystocele and Rectocele are both caused by defects in the fascia. A cystocele is a malformation of the fascia connecting the bladder and the vaginal canal. A portion of the bladder wall bulges the uterine canal is a tube that connects the uterus to the virginals a result of this. Cystocele is divided into three categories: mild, moderate, and severe cystocele. Grade 1—the mildest kind, in which the bladder merely protrudes partially into the vaginal canal. Grade 2: The bladder has descended far enough to reach the vaginal entrance in the moderate type. Grade 3—the most severe version, in which the bladder protrudes through the vaginal opening. Present Complaints and Investigation: Something coming out of vagina not feeling bladder relief immediately, frequent urinary tract infection, heaviness in vagina. Past History: No history of medical and surgical illness, no history previous hospitalization. The main diagnosis, therapeutic intervention and outcome: A case was diagnosed after a physical examination and investigation Cystocele and rectocele with precedential with cervical elongation for further management included inj. c-tax, inj. pan, inj. metro, t-bact ointment, tab-iron, tab-calcium, inj. pause, She was took all treatment and outcomes was good. Conclusion: In order to treat cystoceles successfully, both lateral and central flaws must be evaluated, as poor treatment of either defect will result in recurrence. Rectocele is a more difficult condition to treat.
Keywords
Cystocele, Rectocele, Vagina, Prolapse.
Introduction
The pelvic floor's muscles and connective tissues keep the pelvic organs in place, including the bladder, uterus, and intestines. Anterior prolapsed when the pelvic floor gets weak or overused, this happens. This might occur over time, for example, following vaginal childbirth, long-term constipation, a hard cough, or heavy lifting. Anterior prolapsed can be treated. Nonsurgical treatment is generally helpful for mild or moderate prolapsed. Surgery may be required in more severe situations to retain the vaginal and other pelvic organs in their normal locations.
Pain is the most prevalent and unavoidable complication of surgery, and it might suggest cardiac (tachycardia, hypertension), respiratory (atelectasis, pulmonary infections, and arterial hypoxia), and gastrointestinal (decreased stomach uptake, decreased stomach uptake, and decreased stomach uptake, decreased stomach uptake, decreased stomach uptake, decreased stomach uptake, decreased stomach uptake, decreased stomach uptake, decreased stomach uptake, decreased stomach uptake, decreased paralysed intestine) issues movement, and ileus), and finally urinary incontinence. Identifying and controlling the source of pain after surgery is one of the most difficult challenges [1]. The levatorani muscle and the apical descent abnormalities have been linked to prolapse of the anterior and posterior vaginal walls.
The proportional roles of these factors to descending pathophysiology in distinct vaginal compartments, however, are unknown. In addition, the symptoms of prolapse in these compartments are not well understood [2]. Rectocele and cystocele surgery is typically performed in a hospital setting under a regional (spinal or epidural) or general anaesthetic, with patients spending one or two days. It's enticing to undertake the operation as an outpatient treatment with less bleeding and pain, no surgical support, quick discharge, and, most significantly, no compromise in postoperative results. There have been no research that we are aware of looked into the relationship between rectocele and cystocele. Cystoceles, rectoceles, and enterocytes (all other cystoceles, rectoceles, and enterocytes), uterine and vaginal cysts, and Rectoceles, enterocytes, and uterine and vaginal rectoceles are all examples of rectoceles cysts were also excluded. Cystocele and rectocele recur in the mid-vaginal plane were the most important outcome factors [3,4].
Female patients over the age of 30 who were having cystocele and rectocele repair surgery, treatment, or oral contraceptive pills were included in the study. Chronic diseases include diabetes, hypertension, hepatic or renal failure, and cancer [5]. Different alternatives Depending on the topography of the access route, helical needles, curved needles, plastic sheets, and sheaths are available for situating the mesh arms to assure tissue-sparing insertion. There is currently little long-term evidence on whether the theoretical assumptions that support mesh interposition transfer to successful prolapse repair. Short-term findings, on the other hand, show that the concept is workable, but that 5.3% of women, despite permanent tissue replacement, develop recurrent prolapse within three months following surgery.
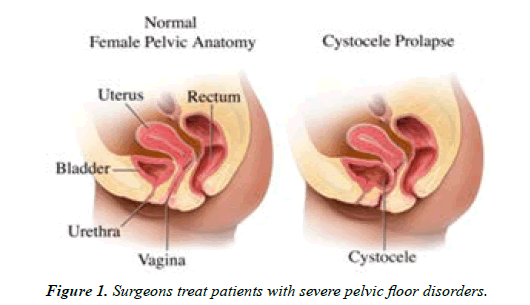
Based on previous experience with ultrasound evaluation of the polypropylene tape in women after tension-free vaginal tape (TVT) repair, we conducted the current study to determine son graphically the postoperative size of the mesh implant, compare it to the size of the implanted mesh, and evaluate whether full support of the anterior or posterior compartment is achieved [6]. Pelvic organ prolapse results in a slew of symptoms that get worse with time. Despite efforts to standardise clinical examinations, a variety of imaging modalities are employed. The purpose of this study was to see if dynamic pelvic magnetic resonance imaging and dynamic cystocele poprocto graph could help surgeons treat patients with severe pelvic floor disorders [7] Figure 1.
Patient information
A 30 years old married female admitted in AVBR Hospital on date 28/09/2021 with chief complaints of Something coming out of vagina not feeling bladder relief immediately, frequent urinary tract infection, heaviness in vagina.
Primary concern and symptoms of patient
Present case visited in AVBR Hospital in OPD base on dated 28/09/2021 with chief complaints of something coming out of vagina not feeling bladder relief immediately, frequent urinary tract infection, heaviness in vagina.
Medical and family and psychosocial history
Patient suffering from Cystocele and rectocele with precedential with cervical elongation for further management Present case belong nuclear family in her family belongs to middle class family. She was mentally stable, she was oriented date, time and place and she maintained good relationship with family members.
Habits
Watching TV, reading newspaper and sleeping and patient don’t have any bad habit like chewing tobacco and smoking. Relevant Past Intervention with Outcomes: Cystocele and rectocele with precedential with cervical elongation for further management for few days before admitted in AVBRH After investigation patients diagnosis is conformed, was observed she took treatment for that and her outcomes was good.
Physical Examination clinical findings
General Examination
30 years female patient have unhealthy, she was conscious and oriented to date, time and place patient body build was moderate and she was not maintain good personal hygiene, her haemoglobin was 9.7 gm, pulse rate is 68, blood pressure-120/90 mmhg, platlate-8l ac/cu mm
The patient was conscious and well oriented to date, time place. His body built was moderate and he maintained good personal hygiene.
• General Examination: state of health was unhealthy,
• Thin body built, but distension of necrosis the height of patient is 168 cm.
• Weight is 50 kg.
• Her vital parameters are normal.
Timeline
The patient was admitted for few weeks, that time patient general condition was poor, she took treatment in A.V.B.R. Hospital and she got the proper treatment. Taking proper medication and now she has been seen the improvement of condition.
Diagnostic assessment
After physical Examination and investigation (such as CBC, Per Vaginal examination, Ultrasonography, Pap’s Smear) Haemoglobin- 9.7 gm, cytopathology-smear shows and group of benign epithelium cells and flue cattle inflammatory cell.
Diagnosis
After all physical examination and investigation patient diagnosis is Cystocele and rectocele with precedential with cervical elongation.
Therapeutic Intervention
Medical intervention: Included Inj. C-tax, Inj. pan, Inj. Metro, T-bact ointment, Tab-iron, Tab-calcium, Inj. pauses, She was taken all treatment and outcomes were good.
Nursing perspective
IV fluid was provided to maintain the fluid and electrolyte monitored heart rate and vital sign per hourly.
Follow up and outcomes
Follow up
Patient advice to daily exercises, and avoids high cholesterol diet, salt diet, given healthy diet. Regular checked up, maintained the personal hygiene as well as take it properly medication by Dr. Order.
Outcomes
In-spite all care patient progress well, he was advised to strictly avoid heavy work, advised to take complete bed rest. Intervention adherence and tolerability: Patients took all prescribed medication regularly, he follow diet, No, any intervention adherence. Patient tolerated treatment properly
Discussion
The elevator muscle and the apical descent abnormalities have been linked to prolapse of the anterior and posterior vaginal walls. The proportional these individuals' contributions variables to the pathophysiology of descent in various compartments vaginal, however, are unknown remain uncertain. In addition, the symptoms of prolapse in these compartments are not well understood. Because of the elegance of trans obdurate or transischioanal access, the ease of application using the manufacturers' needles, the variable mesh sizes that can be cut to size intra operatively, the lack of a laparotomy, the option of permanent tissue replacement after facial reconstruction failure, and Ulmsten's excellent experience with similar materials [8]. The simultaneous treatment of cystocele and rectocele with protease polypropylene multifilament macro pore mesh via the tension-free Tran’s vaginal method it appears to be a secure and successful method surgery procedure. There are a variety of approaches that can be taken, and in the literature, there is currently no significant agreement. If the rectocele is isolated or affects the low or mid rectum, a Tran’s abdominal recto pixy is more appropriate, but if the rectocele is high and/ or connected to other conditions of If you have pelvic stasis, a Trans abdominal recto pixy is a better option appropriate [9]. The Pelvic organ prolapse is defined as a downward descent of the pelvic organs that results in a protrusion of the vagina (POP) is a frequent disease in the United States, accounting for 300,000 surgeries each year. After cystocele, rectocele, or rectum prolapse through the POP is the second most prevalent type of POP is posterior vaginal wall (PVW). Rectocele is typically seen in multi compartment pelvic floor disorders alongside other types of prolapse. Rectocele development mechanisms are still understood, making early detection and progression prediction difficult. Thanks to advances in imaging and computer modelling tools, a range vaginal prolapse has been studied using a variety of finite element (FE) models, providing for a better understanding of the dynamic interactions between pelvic organs and their supporting structures systems. The majority of research has so far concentrated little is known about anterior vaginal prolapse (or cystocele), and involvement of pelvic muscles and ligaments in rectocele's onset and progression. Based on full-scale magnetic resonance imaging, this research generated a three-dimensional (3D) computer model of the female pelvis (MRI) [10]. Studies on different aspects of rectal lesions were reviewed [11-15].
Conclusion
The laparoscopic pelvic floor repair treatment combines the benefits of with the decreased morbidity of a vaginal laparotomy operation. Although Suspension of the utero sacral ligament is the most natural anatomic restoration of abnormalities and thus the ones who are least likely to result in future deformities in vaginal function may be hampered by the anterior or posterior vaginal wall, sacrocol popexy was more popular in Europe. To assess the technique's utility, more research on its long-term efficiency and reliability is required. Sacrocol popexy with mesh interposition is a method for vault prolapse that is both safe and effective. And rectocele repair. To uncover any late issues, as it is necessary to conduct long-term follow-up. Contrary to popular opinion, pelvic organ prolapse is not always chronic and progressive, as our findings show. Patients with grade 1 prolapse frequently have spontaneous regression.
References
- Vahabi S, Karimi A, Beiranvand S, et al. Comparison of the effect of different dosages of celecoxib on reducing pain after cystocele and rectocele repair surgery. Open Anesthesia J. 2020;14(1).
- Berger MB, Kolenic GE, Fenner DE, et al. Structural, functional, and symptomatic differences between women with rectocele versus cystocele and normal support. Am J Obstetrics Gynecol. 2018;218(5):510-e1.
- Durnea CM, Khashan AS, Kenny LC, et al. Prevalence, etiology and risk factors of pelvic organ prolapse in premenopausal primiparous women. Int Urogynecol J. 2014;25(11):1463-70.
- Sand PK, Koduri S, Lobel RW, et al. Prospective randomized trial of polyglactin 910 mesh to prevent recurrence of cystoceles and rectoceles. Am J Obstetrics Gynecol. 2001;184(7):1357-64.
- Vahabi S, Abaszadeh A, Yari F, et al. Postoperative pain, nausea and vomiting among pre-and postmenopausal women undergoing cystocele and rectocele repair surgery. Korean J Anesthesiol. 2015;68(6):581.
- Tunn R, Picot A, Marschke J, et al. Sonomorphological evaluation of polypropylene mesh implants after vaginal mesh repair in women with cystocele or rectocele. Ultrasound in Obstetrics and Gynecology: The Official J Int Society Ultrasound Obstetrics Gynecol. 2007;29(4):449-52.
- Kaufman HS, Buller JL, Thompson JR, et al. Dynamic pelvic magnetic resonance imaging and cystocolpoproctography alter surgical management of pelvic floor disorders. Dis Colon Rectum. 2001;44(11):1575-83.
- Aubert M, Mege D, Nho RL, et al. Surgical management of the rectocele–an update. J Visceral Surgery. 2021;158(2):145-57.
- Chanda A, Meyer I, Richter HE, et al. Vaginal changes due to varying degrees of rectocele prolapse: A computational study. J Biomechanical Engineering. 2017;139(10).
- BhojrajN SG. The effect of Panchagavya formulations in the case of CA Rectum. Int J Ayurvedic Med. 2020;11(3):572-4.
- Khandare K, Ghormode P. Prolapsed rectal submucosal hematoma in pediatric case. The Pan African Med J. 2020;37.
- Sreedhar R, Jajoo S, Yeola M, et al. Role of Tumour Markers CEA and CA19-9 in Colorectal Cancer. J Evolution Med Dent Sci. 2020;9(46):3483-9.
- Thomas S, Bhake A. Expression of K-Ras, p53 and Ki-67 in Precancerous and Cancerous Lesions of Colorectum. J Evol Med Dental Sci. 2020;9(32):2261-6.
- Tote D, Domakunti R, Tote S. Scenario of Rectal Carcinoma Cases in a Rural Setting of Central India. J Evolution Med Dent Sci. 2020 Nov 16;9(46):3434-9.
- Borgaonkar AP. Passage of Gangrenous Small Bowel Per Rectum Following Superior Mesenteric Vessel Thrombosis. J Clinical Diagnostic Res. 2019;13(12).
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref