Review Article - Journal of Clinical Pathology and Laboratory Medicine (2022) Volume 4, Issue 4
Influence of urinary tract infections in renal sturvite stone.
Sheena Aliyas1*, Murugan K1, Thanga Mariappan K21Department of Biotechnology, Manonmanium Sundaranar University, Tirunelveli, Tamilnadu, India
2Professor in Laboratory Medicine, Vivek Institute of Laboratory Medicine, Nagercoil, Tamilnadu, India
- *Corresponding Author:
- Sheena Aliyas
Department of Biotechnology
Manonmanium Sundaranar University
Tirunelveli – 627 012, Tamil nadu, India
E-mail: sheenaaliyas025@gmail.com
Received: 29-Jun-2022, Manuscript No. AACPLM -22-69698; Editor assigned: 01-Jul-2022, PreQC No. AACPLM-22-69698 (PQ); Reviewed: 15-Jul-2022, QC No. AACPLM -22-69698; Revised: 20-Jul-2022, Manuscript No. AACPLM-22-69698 (R); Published: 27-Jul-2022, DOI:10.35841/aacplm-4.4.119
Citation: Aliyas S, Murugan K, Mariappan TK. Influence of urinary tract infections in renal sturvite stone. J Clin Path Lab Med. 2022;4(4):119
Abstract
Struvite stones refers to calculi that form following Urinary Tract Infections (UTIs) caused by urease-producing organisms. Renal struvite stones consist of magnesium ammonium phosphate, carbonate apatite and monoammonium urate. Alkaline urine plays a pivotal role in stone formation. Urinalysis and urine culture are essential for laboratory diagnosis. The relationship between urinary stones and UTIs is well known and shows two different clinical pictures stones that develop following UTIs (infection stones) which play a key role in stone pathogenesis, and stones complicated by UTIs (stones with infection) which are metabolic stones that passively trap bacteria from coexistent UTIs and may consist of calcium or non- calcium. This review article reveals the general characterization of kidney stones, impact of UTIson pathogenesis and Pathophysiology of struvite stone formation and their clinical features
Keywords
Urinary tract infection, Renal struvite stone, Pathogenesis, Clinical significance.
Introduction
Kidney performs several functions that are relevant to health. Of these, the most important of which are to dispatch waste products from the body and to regulate the chemicals levels. It also plays a vital role in keeping the acid-base balance in the body and regulating electrolyte balance and blood pressure. Ureters are long, narrow tubes that hold the filtered substances and water (urine) from the kidneys to the bladder. Urolithiasis (mineral formation) is one of the urologic diseases in Asia. It is a disease of the genitourinary system as a result of formation of urinary stones at any place in the renal tract [1]. Thus, it has a profound impact on value of life and socioeconomic factors. Kidney stones are also called as renal calculi, nephrolithiasis or urolithiasis as these are hard deposits made of minerals and salts that form inside kidneys. Urinary stones are solid concretions or crystal aggregations formed in the kidneys from dietary minerals in the urine. Kidney stone is usually called as “Silent Disease".
Calcium Oxalate [Ca(COO)2], (70–80%), calcium phosphate [CaHPO4.2H2O] (5–10%), uric acid (5–10%), struvite [(NH4) MgPO4- 6(H2O)] (5–10%) and cysteine [C6H12N2O4S2 ] (1–5 %.) are found to be the major constituents of urinary stones as reported by several analytical studies [2].
Renal system and stones
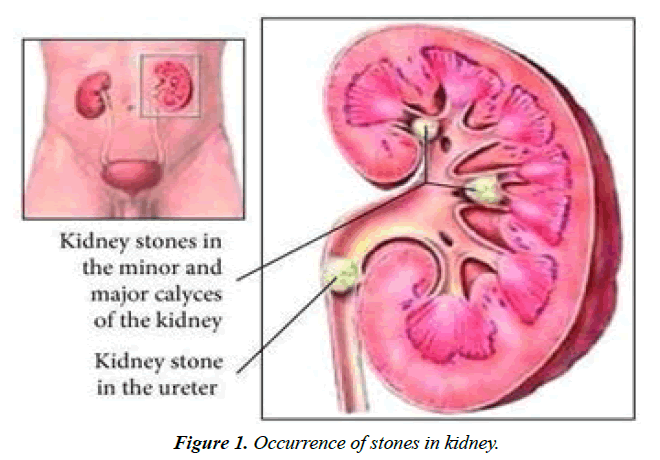
The urinary filtrate is formed in the glomerulus and passes into the tubules where the volume and content are altered by reabsorption or secretions. Alterations in urine composition take place in the distal tubule and collecting ducts. The loop of Henle makes urine concentrated including of 95% water, 2.5% urea, 2.5% mixture of minerals, salts, hormones, and enzymes [3]. Subsequently, glucose, sodium, chloride, and water are reabsorbed in the proximal tubules, and returned to the blood stream along with essential nutrients such as amino acids, proteins, bicarbonate, calcium, phosphate, and potassium. In the distal tubule, the salt and acid-base balance of blood is regulated. The position of stones in kidney may vary as depicted in Figure 1.
Stone formation is a multifaceted process and it results as a sequence of events, including crystal nucleation, growth, and aggregation, and crystal retention within the renal tubules [4]. It is a hard, crystalline mineral material, formed within the kidney or urinary tract. Men tend to be affected more often than women Table 1. But, it is relatively rare in children as it is associated with inborn error of metabolism. Usually, small stones are passed out from the body with either a small or large degree of pain, but, larger stone may lodge in the ureters, bladder or urethra, blocking urine flow and causing extreme pain [5].
| S.NO. | Composition | Rate of Incidence (%) |
Appearance | Causative Factors |
|---|---|---|---|---|
| 1. | Calcium | 70–80 | High densities and gross morphologies | Numerous, including primary hyper parathyroidism, chronic diarrhea, and distal renal tubular acidosis |
| 2. | Magnesium ammonium phosphate (struvite) |
15–20 | A struvite calculus involving the renal Pelvis and extending into at least two calyces |
Urinary infection with urease-producing bacteria |
| 3. | Uric acid | 5–10 | Pure uric acid stones are Radiolucent on radiography |
Dietary purine excess, uric acid overproduction or over excretion |
| 4. | Cystine | 1–3 | Contain low-attenuation foci (voids) on CT | Impaired renal cysteine reabsorption |
| 5. | Medications And their metabolites |
1 | Indinavir can be radiolucent even on CT | Due to excessive use of some medications |
Table 1. Causes and different types of urinary stone.
Occurrence of renal stone disease in India
In overview of India, renal stone disease is prevalent, with an expectancy of 12% in a total population reported to be prone to urinary stones. Among these 12%, 50% of the populations are severely affected by renal damage, which even leads to a loss of kidneys. Unlike in South India, where a few reported percentages affected by Urolithiasis, in North India, there is a steep 15% of the population within the realm of renal stone disease [6]. Therefore, considering the prospects of the kidney stone belt, which are affected by renal stone disease in India, a proper corollary needs to be developed. This renal stone belt occupies the part of Maharashtra, Gujarat, Rajasthan, Punjab, Haryana, Delhi, Madhya Pradesh, Bihar, and West Bengal.
General pathways for renal stone formation
The genesis of urinary stone formation is the end result a multi-factorial processes including urinary saturation, super saturation, nucleation, crystal growth, aggregation of crystals, crystal retention, and, to end with stone formation in inside renal tubules. Crystalluria is usually observed in individual, but if crystals remain apart from each other. Some chemical and electrical forces in crystals could give rise to the process of aggregation on epithelium, which turns to stones [7]. These urinary stone particles can be retained in the kidney and act as a nucleus for the formation of future stones. In certain cases, urinary stones become very large and cause the obstruction of the kidney drainage system resulting in severe pain, bleeding, and infection or kidney failure. Overall observations on kidney stone formation concluded that the process required three broad conceptual categories such as excessive concentration of solutes in excess of their solubility in the urine, imbalance of modifiers (promoters and inhibitors) and crystallization in the urine and epithelial abnormalities that allow attachment and subsequent growth of these crystals in to stone [8]. Dietary habit is found to be an important cause of the increasing incidence in the pathogenesis of urinary stone in the last few decades. The emergence of Urolithiasis may be due to a systemic disorder associated with a group of cardiometabolic conditions such as obesity, diabetes, hypertension, metabolic syndrome and coronary artery disease, all of them in turn related to nutritional inadequacies.
Factors involved in urinary stone formation
Stone formation is a complex process. It depends on the interaction of various factors including urinary concentration of stone forming ions, urinary pH, and urinary flow rate, the balance between promoter and inhibitory factors of crystallization and anatomic factors that encourage urinary stasis. Of these, super saturation of one or more urine mineral components and their crystallization by sticking together are the principal crystallization mechanisms in stone development. After crystallization, they are retained in the urinary tract by aggregation and adhesion to urothelial cells [9]. Urease producing bacteria such as Proteus sp., Klebsiella sp., E.coli, Corynebacterium sp., and Pseudomonas sp., also plays an important role in the development of struvite stone by means of enhancing the alkalization of urine.
General constituents of urinary stones
In view of making ease of treatment decisions, categories of patients with kidney stone are grouped into two major types as non-calcium stones and calcium stones. The group non calcium stones including struvite stones, Matrix stones, uric acid stones, other purine stones (xanthine and 2,8 – dihydroxyadenine), cysteine stones and drug stones [10]. Similarly, calcium stones compiled with single and sporadic stone formers (who are not at risk of chronic kidney disease), single and sporadic stone formers (who are at risk of chronic kidney disease) and recurrent stone formers.
Further, calcium stones have been sorted out according to their mineral composition including calcium oxalate stones composed of calcium oxalate or calcium oxalate mixed with calcium phosphate, pure calcium phosphate stones, uric acid stones, cysteine stones are associated with cystinuria struvite stones which are the result of chronic urinary tract infections caused by specific strains of bacteria. These stones are usually scaled as <5 mm, 5-10 mm, 10-20 mm, and >20 mm [11]. S According to their anatomical position, kidney stones can also be classified as the upper, middle and lower calyx; the renal pelvis; the upper, middle and distal segment of the ureter; or the urinary bladder.
Properties of Different Urinary Stones based on Chemical Composition
Calcium based urinary stones
It account for 70– 80% of urinary tract calculi. Calcium oxalate is the most common type of calcium-based stone comprising 60% of all types of calculi. It measures as high as 1700 HU on CT and composed of calcium hydrogen phosphate dihydrate. Hypercalciuria is due to intestinal over absorption of calcium leading to transient elevation of serum calcium, increased filtered load of calcium, and suppressed serum Para Thyroid Hormone (PTH), with subsequent increased the risk of renal calcium based stone formation.
Magnesium ammonium phosphate based stones
These are also called as struvite stones and account for 15– 20% of all urinary stones. This may occur only in association with urinary infection by urea-splitting bacteria such as Proteus sp., Pseudomonas sp, Klebsiella sp., and Enterococci. However, Escherichia coli are found to be a major causative agent of struvite formation, despite of not urease producing one. Under infected conditions, urinary urea is hydrolyzed to ammonia by bacterial urease, resulting in alkaline urine that further promotes phosphate dissociation and allows formation of magnesium ammonium phosphate stones [12].
Uric acid based stones
It account for 5-10% of all urinary stones. The formation of uric acid stones is promoted by hyperuricosuria and acidity in urine. The common causative factors include gout and chronic diarrhea. Patients with a high body mass index or diabetes have become more prone to form uric acid stones when compared to general population.
Cystine based stones
It account for 1–3% of all urinary stones and result in a consequence of cystinuria, is an autosomal recessive disorder characterized by a defect in intestinal and renal tubular transport of dibasic amino acids, resulting in excessive urinary excretion of cystine. Cystine is relatively insoluble in urine and, therefore, precipitation of cysteine and subsequent stone formation occur at physiologic urine conditions. These are often referred to as “ground-glass” stones and can be radiolucent [13].
Drug induced stones
Excessive use of drugs such as Indinavir (52.9%), Triamterene (18.1%), Sulfonamides (12.2%), and Amorphous silica (10.1%) can lead to increased risk of stone formations. Changes in medication, dose adjustment, increased diuresis, and possibly agents to alter urine pH are to be associated with drug induced stone formation. Further, common herbal supplements that may induce renal calculi include ephedrine, a stimulant and weight loss product, as well as guaifenesin, an expectorant. The metabolites of drugs can result in the formation of matrix stones.
Struvite stones
Struvite stones are composed of magnesium ammonium phosphate, are also known as ‘infection stones’, and account for 15%-20% of all stones. An infected kidney stone is an infection as a result of Urinary Tract Infections (UTIs) with urease-producing bacteria. It is characterized to obstruct the urinary tract leading to pyelonephritis. These stones are mainly composed of magnesium ammonium phosphate (struvite) and/or calcium carbonate apatite result from chronic infections with urease producing bacterial pathogens. The incidence of infected stones is more common in women (10 to 11%) and elderly patients. It accounts for only 4% in male [14].
Pathogenesis of struvite stones
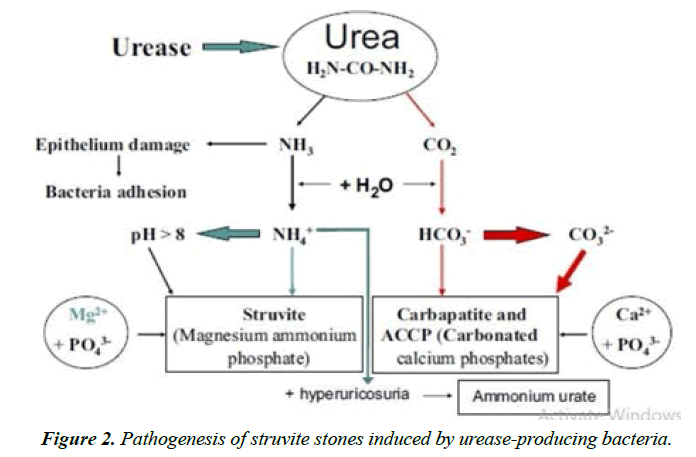
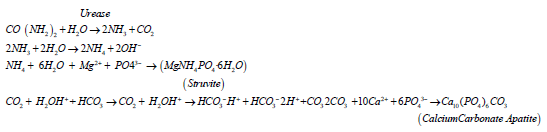
In the presence of urease of urinary pathogens, urea splits into ammonia and carbon dioxide. Ammonia is then reacted with water to become ammonium and hydroxide ions, which makes an alkaline milieu. Under this alkaline nature, the ammonium combined with magnesium, phosphate, and water to produce magnesium ammonium phosphate stones. Carbon dioxide eventually is then broken down into carbonate, which combines with calcium and phosphate to form calcium carbonate apatite stones.
Urease-producing bacterial pathogens such as Proteus spp, Klebsiella spp., Providencia spp., Morganella morganni, and Staphylococcus aureus are found to be the major causative agents of struvite stones. Infection stones are usually asymptomatic or present with UTIs, flank or abdominal pain, fevers, gross hematuria, or less commonly with sepsis or renal insufficiency. Patients with indwelling catheters, neurogenic bladder, and urinary diversion play an important role in developing infection stones due to chronic bacterial colonization. It has been found that these stones are associated with progressive morbidity and mortality between the cases of nonsurgical (28%) and non surgical treatments (7%) for 10years. Urease negative bacterial pathogens including Escherichia coli and Enterococcus spp, are the predominant organisms colonizing these metabolic stones.
Chemistry of struvite stones
Incidence of Ammonium ion and trivalent phosphate in urine plays a vital role in the development of infected stone. This may be a result of non-physiological condition which sourced by infection. The renal tubule makes ammonium only when the organism needs to excrete an acid load. In acid urine without abnormal bicarbonate losses, the excreted acid can be described by the empirical equation.
In which, acid is largely univalent phosphate [HPO4]2−. Trivalent phosphate (PO43-) is virtually absent in acid urine when the kidney is making ammonia. When the urinary pH is high enough to contain significant amounts of trivalent phosphate, tubular production of ammonia has stopped.
For infected stone to form, non-physiological conditions such as urea-splitting infections are required. Hydrolysis of urea is catalyzed by urease at pH 7. It is measured that ureases catalyze the breakdown of urea into ammonia and carbamate ions or equivalently into ammonia and carbonic acid at a rate 1014 to 1015 times earlier than the non-catalyzed reaction.
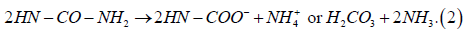
Then, ammonia combined with water to yield ammonium hydroxide:
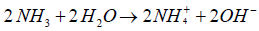
In such alkaline condition, carbonic acid is linked with bicarbonate and carbonate ions causes alkalization of the urine, favoring trivalent phosphate, formation of ammonium ion and formation of carbonate ion. It also enhanced the emergence of both mineral components of triple phosphate stones, struvite and carbonate apatite. Adding ammonium hydroxide in normal urine may rapidly cause precipitation of amorphous struvite. Urease producing Proteus sp. will cause infection stones, while Escherichia coli which do not split urea, will not. Struvite formation by Proteus sp. can be halted by using a urease inhibitor. Struvite crystals can be generated in vitro under acidic as pH 6.0, but the morphology of these crystals differed from those formed at higher pH values.
Microbiology of struvite stones
UIS in resulting of chronic infections caused by bacteria with urease production and regularly involved in urinary tract obstruction. They required approximately 4 to 6 weeks for forming an infection stone. UIS consist of monoammonium urate, struvite (magnesium ammonium phosphate) and/ or carbonate apatite. Several diseases including obesity, childhood onset asthma, and cardiovascular disease are associated with disruptions to the microbiota that inhabit the human body. As far as infected stone formations, In stone formation, Intestinal micro flora act as major causative agent. Emerging evidence indicates that bacteria are present in and contribute to vascular calcifications Therefore; it is possible that bacteria also are present in and contribute to urinary calcifications. The stone containing kidney is infected with Proteus sp., Staphylococcus a/bus (two cases), and E.coli. It was observed that the urine contained increased quantities of cellular debris and protein that infected with the Proteus sp., and Staphylococcus sp. These two strains were able to split urea, and the stones from these infected patients were composed of struvite and carbonate-apatite. The urine from the kidney infected with E. coli was acidic, and the stone from this kidney was composed of uric acid and urates.
Urinary tract infections and struvite stones
Several published reports attest to the difficulty (and oftentimes impossibility) of eradicating urinary infection in the presence of a stone. Residual stones and/or residual or persistent infection set the stage for recurrent stone formation. Thus, UTI causes growth of the stone namely, struvite and carbonate-apatite stones form only as a consequence of the hydrolysis of urea by urease. Only bacteria that produce urease form such stones. The role of non-urease-producing bacteria in the pathogenesis of other types of urinary stones (i.e., calcium oxalate, hydroxyapatite, etc.) is incompletely defined. . The role of non- urease-producing bacteria in stone disease has generally been considered of secondary importance. E. coli associated with struvite stones have been reported, however, but in these cases the struvite has often been mixed with oxalate content. E. coli is the most commonly isolated species from the patients infected with UTI due to the fact that its short replication rate results in it outcompeting and outgrowing other bacterial species. This is especially true in the high pH environment associated with the presence of ureasepositive bacteria, which tends to be inhibitory for bacterial growth, including P. mirabilis The reason that urease-positive bacterial species can still be isolated from stone cultures despite the unfavorably high pH of the urine is that they are protected from a potentially unfavorable urinary environment by the surrounding stone, allowing them to survive. However, both clinical and laboratory-based, are required to further evaluate coexistence and relationship among common urinary pathogens and urease-producing organisms in the setting of infection stones.
Effect of urease producers on struvite stones formation
Infected stone formation is solely associated with bacteria that positive for urease enzyme production, belonging to both gram-positive and gram-negative species such as Proteus sp., Staphylococcus sp., Pseudomonas Staphylococcus sp., Providencia Staphylococcus sp., and Klebsiella sp. Triple phosphate stones are mostly caused by Proteus sp., and Klebsiella sp. About 90% of these organisms split urea. Proteus mirabilis alone accounts for more than half of all urease-positive infections. In addition, Pseudomonas sp., Klebsiella sp., and Providencia species are found as important causative agents. In the formation of infected stones, biofilm matrix producing bacteria which form staghorn stone tends to create an isolated microenvironment for the organisms from being shed into the surrounding urine and such gelatinous material may increase the risk for the culture practices to assess the true situation. Some of these stones may be caused by Ureaplasma urealyticum. It was observed that the bacterial pathogens namely Klebsiella spp. and Staphylococcus spp (55%) from patients with complicated UTIs exhibited a less efficiency in urease production when compared to Proteus spp and Morgenalla morganii spp. E. coli and Pseudomonas spp. were the most common bacteria isolated from stone cultures, followed by the urease-splitting bacteria typically involved in struvite stone formation.
The clinical observation that urea-splitting infection is associated with increased quantities of urinary colloids has not, to my knowledge, been studied experimentally. The source of these mucoproteins and their role in calculogenesis is incompletely delineated. Different factors including obesity, childhood onset asthma, and cardiovascular disease are related with disruptions to the microbiota that inhabit the human body. Therefore, it is possible that bacteria also are present in and contribute to urinary calcification and carbonateapatite, which results in crystal formation. These changes are associated with an increase in urinary proteins, which may also play a role in calculogenesis Figure 2. The bacterial isolates such as Proteus, Klebsiella, and Pseudomonas and Staphylococcus species are reported as the most important urease producers. A rare association has been found with E.coli in stone formation. Bacteria both in the urinary and gastrointestinal tracts have been associated to USD through both gain and loss of function mechanisms. Urinary Tract Infections (UTIs) are caused by diverse bacteria primarily from the Enterobacteriaceae family. Some UTI-associated bacteria produce urease, which breaks down urea, increases pH, and can lead to struvite stone. Accordingly, the UTI pathogens are standardized on basis of their ability in producing enzyme and depicted in Table 2.
| S.No. | Organism | % positives |
|---|---|---|
| 1. | P. vulgaris | 99.6 |
| 2. | P. mirabilis | 98.7 |
| 3. | P. morganii | 91.8 |
| 4. | P. rettgeri | 99.0 |
| 5. | Providencia al cahfaciens | 99.0 |
| 7. | Kiebsiella pneumoniae | 63.6 |
| 8. | Pseudomonas aeruginosa | 32.6 |
| 9. | Serratia marcescens | 29.0 |
| 10. | Serratia liquefaciens | 5.0 |
| 11. | Enterobacter aerogenes | 2.6 |
| 12. | Citrobacterfreundii | 0 |
| 13. | E. coli | 0 |
Table 2. List of urease producers.
Clinical Significance of Struvite Stones
Risk factors to formation of struvite stones
Risk factors for stone formation are generally grouped into non-dietary, dietary, and urinary.
Non-dietary risk factors
Comparatively, patients belonging to stone-forming family members have a 2.5 times greater risk of developing stones than those without stone-forming family members. The genetic basis of renal stone disease may be due to derangement of a metabolic pathway, diversion to an insoluble product,failure of transport and renal tubular acidosis in relation to the disorders of Adenine Phospho Ribose Transferase (APRT) deficiency, primary hyperoxaluria, cystinuria and autosomal dominant distal renal tubular acidosis. Besides, a number of medical conditions have high association with kidney stone disease. Any type of chronic diarrhea state including Crohn’s disease, gastric bypass, and inflammatory bowel disorder, primary hyperparathyroidism, obesity, and gout have increased the risk of kidney stone disease.
Dietary risk factors
The normal chemical composition of urine depends on the volume intake, diet, and kidney regulation of metabolites. Dietary risk factors include meals high in animal protein, oxalate, and salt. Low calcium intake and low urine volumes are implicated as other dietary causes of stone disease. Therefore, all kidney stone patients should restrict their daily animal protein (in particular red meat) to less than 10-12 ounces/day and decrease their salt (sodium) intake to less than 3,000 mg/day, if not < 2,400 mg/day Table 3.
| S.No. | Particulars | Concentration | |
|---|---|---|---|
| Male | Female | ||
| 1. | Calcium (mmol per 24 h) | ≥7.5 | ≥6.2 |
| 2 | Oxalate (mmol per 24 h) | ≥420 | ≥360 |
| 3. | Sodium (mmol per 24 h) | ≥250 | ≥250 |
| 4. | Urate (mmol per 24 h) | ≥4.5 | ≥4.2 |
| 5. | Cystine (mmol/L) | ≥1500 | ≥1500 |
| 6. | Citrate (mmol per 24 h) | ≤1.68 | ≤1.68 |
| 7. | Magnesium (mmol per 24 h) | ≤2.3 | ≤2.3 |
| 8 | Urine volume (L per 24 | ≤1 | ≤1 |
Table 3. Concentration of kidney stones.
Biochemical risk factors
It has been observed that approximately 97% of kidney stone patients have one or more identifiable urinary risk factors for stones include high urinary calcium (hypercalciuria), high oxalate (hyperoxaluria), high uric acid (hyperuricosuria), low urine citrate (hypocitrituria), and/or urinary tract infection Table 4.
| S.No. | Category | Factors |
|---|---|---|
| 1. | Anatomic abnormalities | Calyceal diverticulum or cyst |
| Horseshoe kidney Medullary sponge kidney (tubular ectasia) |
||
| Ureteral stricture | ||
| Ureterocele | ||
| Ureteropelvic junction obstruction | ||
| Vesicoureteral reflux | ||
| 2. | Diseases | Gastrointestinal diseases and bariatric surgery (e.g., Crohn disease, enteric hyperoxaluria after urinary diversion, intestinal resection, jejunoileal bypass, malabsorptive conditions) |
| Hyperparathyroidism | ||
| Nephrocalcinosis | ||
| Sarcoidosis | ||
| 3. | General factors | Calcium phosphate stones |
| Early onset of urolithiasis (especially children and teenagers) | ||
| Family history of stone formation | ||
| Infection-associated stones (struvite or carbonate apatite stones) | ||
| Solitary kidney | ||
| Uric acid– and urate-containing stones |
Table 4. Other risk factors for kidney stone recurrence.
Symptoms of urinary stones
Usually, no symptoms caused by a kidney stone. However, stones typically do cause symptoms while passing through the urinary tract including a gripping pain in the back blood (red, pink, or brown urine) and urine that smells bad and looks cloudy, frequent need to urinate, vomiting, nausea, fever and chills, and a burning feeling when urinate Table 5. The main symptoms of stone passage are “flank pain” and it makes radiation of the pain around to the lower abdomen on the affected side.
| S.No. | Medication Particulars | Examples |
|---|---|---|
| 1. | Antibiotics | Ampicillin,amoxicillin,ceftriaxone (Rocephin),furans (e.g.,nitrofurantoin), pyridines, quinolones, sulfonamides (e.g., sulfamethoxazole) |
| 2. | Carbonic anhydrase inhibitors | Acetazolamide, Topiramate (Topamax) |
| 3. | Diuretics | Furosemide (Lasix), Triamterene (Dyrenium) |
| 4. | Ephedra alkaloids | Herbal products used as stimulants and appetite suppressants |
| 5. | Laxatives, especially if abused (specific to ammonium urate stones) |
Overuse of any laxative resulting in electrolyte loss |
| 6. | Potassium channel blockers | Amiodarone, Dalfampridine (Ampyra;multiple sclerosis therapy), Sotalol(Betapace) |
| 7. | Reverse transcriptase inhibitors and protease inhibitors | Efavirenz (Sustiva),Indinavir (Crixivan), Nelfinavir (Viracept), Raltegravir (Isentress) |
| 8. | Sulfonylureas | Therapies for type 2 diabetes mellitus |
| 9. | Others | Aluminum magnesium hydroxide, ascorbic acid,calcium,dexamethasone, guaifenesin, phenytoin (Dilantin), vitamin D |
Table 5. Influence of Medications with Kidney Stone Formation.
Diagnostic evaluation of urinary stones
Standard evaluation of urinary stones includes a detailed medical history and physical examination. Patients with urethral stones may have the symptoms of loin pain, vomiting, and sometimes fever, but may also be asymptomatic in some cases. Stones at the ureterovesical junction can cause urgency and suprapubic discomfort. Physical evaluation is typically non- specific for urinary stones but is important for evaluating for other conditions. Blood and urine studies can also access renal function and hematologic status. Especially, elevated levels of WBC count, the hemoglobin, electrolyte, blood urea nitrogen, and creatinine levels reflect renal and metabolic status Table 6.
| S.No. | Evaluation Option | Considerations |
|---|---|---|
| 1. | History | Symptoms like flank pain, abdominal pain, fevers, chills, gross hematuria, dysuria, hematuria, urgency, frequency. |
| 2. | Urologic history | UTI, pyelonephritis, Urolithiasis, Urinary diversion and/or Neurogenic bladder, Anatomic abnormalities, Chronic indwelling catheters, Urethral strictures, Prior urologic surgeries |
| 3. | Physical examination | Fever/hypothermia, vital signs, costovertebral angle tenderness, abdominal/suprapubic tenderness and Musculoskeletal deformities |
| 4. | Laboratory tests | urinalysis; and urine culture, basic metabolic panel, complete blood count, coagulation pane and Blood cultures |
| 5. | Radiology | Noncontrast Computed Tomography scan (gold standard) Kidney ureter bladder radiography and/or renal US (best used for follow-up) and Reno gram. |
Table 6. Preliminary Examination of patients suspected with infection stones.
Diagnostic evaluation of infected stones
Patients with infection stones exhibits vague abdominal o back pain, recurrent UTIs, and/or gross hematuria. A focused history and physical examination should be done as a preliminary diagnostic evaluation.
Conclusion
Kidneys stone is one of most common problems in developing countries of the world and the incidence appears to be growing more. It depends upon various intrinsic and extrinsic factors such as like metabolic, environmental, and nutritional factors. Some clinical conditions including high fat diet, inadequate nutrition, and addition of food that contains oxalate crystals, high protein diet and post-surgery defects are found to be associated with kidney stone formation. Several clinical reports revealed that the multiple co-morbidities have been found in patients with struvite stones.
It also described that several risk factors are associated with struvite stone formation and UTIs. Kidney stone disease is a complicated problem. The overall incidence of these stones is low, but the potential morbidity for an individual patient is quite high. Mostly, struvite stones are heterogeneous in both composition and bacterial examinations. Bacteria and kidney stones are clinically associated as they often present in the same patients. Patients with struvite stones often have shown positive for urine and/or stone cultures. Thus, it should be elaborated that the reason behind clinical kidney stones and bacteria associations as emerging research topic. The study should also be extended towards sequencing a larger number of stones to determine if the bacteria present are consistent between stone composition and other covariates such as sex and age. Currently, different modern diagnostic and treatment methods have led to a better understanding of the kidney stone disease. Among many methods, herbal therapy has been found to be a preferred one for removal of kidney stones.
References
- Griffith DP. Struvite stones. Kidney Int. 1978;13(5):372-82.
- Fontenelle LF, Sarti TD. Kidney stones: treatment and prevention. American family physician. 2019;99(8):490-6.
- Zampini A, Nguyen AH, Rose E, et al. Defining dysbiosis in patients with urolithiasis. Sci Rep. 2019;9(1):1-3.
- Flannigan RK, Battison A, De S, et al. Evaluating factors that dictate struvite stone composition: a multi-institutional clinical experience from the EDGE Research Consortium. Can Urol Assoc J. 2018;12(4):131.
- Holmgren K, Danielson BG, Fellstrom B, et al. The relation between urinary tract infections and stone composition in renal stone formers. Scand j urol nephrol. 1989;23(2):131-6.
- Tasian GE, Copelovitch L. Evaluation and medical management of kidney stones in children. J Urol. 2014;192(5):1329-36.
- Jayaraman UC, Gurusamy A. Review on uro-lithiasis pathophysiology and aesculapian discussion. IOSR J Pharm. 2018;8(2):30-42.
- Hulton SA. Evaluation of urinary tract calculi in children. Arc Dis Childh. 2001;84(4):320-3.
- Tasian GE, Copelovitch L. Evaluation and medical management of kidney stones in children. J Urol. 2014;192(5):1329-36.
- Flannigan R, Choy WH, Chew B, et al. Renal struvite stones—pathogenesis, microbiology, and management strategies. Nat Rev Urol. 2014;11(6):333-41.
- Evan AP. Physiopathology and etiology of stone formation in the kidney and the urinary tract. Pediatr Nephrol. 2010;25(5):831-41.
- Alelign T, Petros B. Kidney stone disease: an update on current concepts. Advances in urol. 2018;2018.
- Dhole AR, Yeligar VC, Dist-Kolhapur K. Urolithiasis and its herbal remedies. Int J Sci Res Sci Technol. 2018;4(11):150-6.
- Ganesamoni R, Singh SK. Epidemiology of stone disease in Northern India. InUrolithiasis 2012;39-46.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref