Case Report - Immunology Case Reports (2018) Volume 2, Issue 2
Henoch-schonlein purpura vasculitis revealing human immunodeficiency virus infection.
- *Corresponding Author:
- Emna Bahloul
Department of Dermatology, Hedi Chaker Hospital 3029, Sfax, Tunisia
Tel: +21692020209
E-mail: emnabahloul86@gmail.com
Accepted date:November 12, 2018
Citation: Bahloul E, Koubaa M, Fatma F, et al. Henoch-schönlein purpura vasculitis revealing human immunodeficiency virus infection. Immunol Case Rep 2018;2(1):11-15.
DOI: 10.35841/immunology-case-reports.2.2.11-13
Visit for more related articles at Immunology Case ReportsAbstract
Henoch-Schönlein purpura vasculitis, characterized by purpura, arthralgia, abdominal pain, and renal disease, can rarely reveal HIV infection. We present here a new case of Henoch-Schönlein purpura vasculitis in a 42-year old man revealing HIV infection with complete remission after antiretroviral treatment.
Keywords
Purpura, Vasculitis, Henoch-schönlein purpura, HIV.
Introduction
Next to the blood and lymphatic systems, the skin in Human Immunodeficiency Virus (HIV) infection is the most commonly affected organ. Cutaneous manifestations can help stage HIV infection and may be the first sign of this disease. Henoch-Schönlein purpura vasculitis, characterized by purpura, arthralgia, abdominal pain, and renal disease, can rarely reveal HIV infection. We present here a new case of Henoch- Schönlein purpura vasculitis in a 42-year old man revealing HIV infection with complete remission after antiretroviral treatment.
Case Report
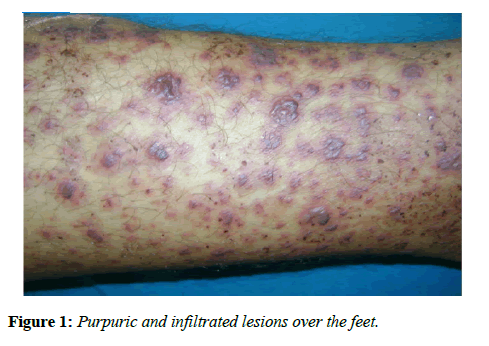
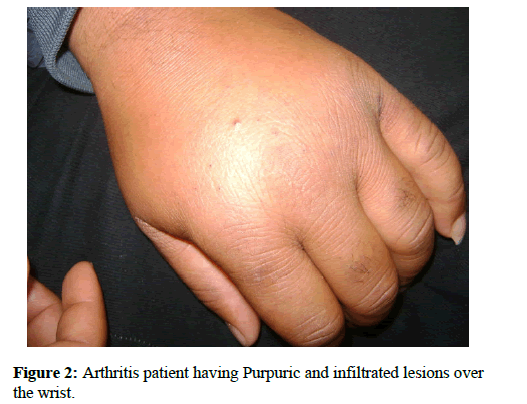
NZ, a healthy 42-year-old man, presented to the department of dermatology with a fifteen-day history of cutaneous lesions, appearing 15 days after a sore throat. The patient complained about arthralgia and reported two episodes of rectal bleeding. There was no history of medication use. The physical examination was remarkable for the presence of multiple pinhead size, purpuric and infiltrated lesions over the feet (Figure 1). The patient had wrist and knee arthritis (Figure 2). His temperature was 38°C; other vital signs were normal.
Laboratory analyses showed a white blood cell count of 7970 cells/mL with lymphopenia of 1420 cells/mL and normal platelet counts. His C-reactive protein was 93 mg/mL and serum creatinine level was 71 μmol/L. A urinalysis showed a red cell count of 249000 cells/min, and 24 h urine collection revealed 0.48 g of protein. The liver function and coagulation analysis were normal. The skin biopsy performed on a purpuric lesion revealed leukocytoclastic vasculitis of the small vessels, characterized by the presence of upper dermal perivascular infiltrates, primarily consisting of neutrophils with karyorrhexis. Deposition of IgA and complement C3 in the vessel walls was noted on direct immunofluorescence staining.
Based on the association of palpable purpura, arthralgia, abdominal pain, renal disease and leukocytoclastic vasculitis, the diagnosis of Henoch-Schönlein Purpura (HSP) wasthus made.
Once the patient presented a purpura with fever, infectious and immunologic investigations were done. The serologic tests for Epstein Barr Virus (EBV), Cytomegalovirus (CMV) revealed ahealed old infection, hemoculture and tests for detection of hepatitis (HBV, HCV) were negative. Nuclear antibodies were positive at 1/160. Anti-neutrophilic cytoplasm anti-bodies were weakly positive. Rheumatoid factor, cryoglobulinemia and tests for circulating immune complex were all negative. However, HIV serology was positive, the HIV-RNA viral load was 80200 copies/mL (log 3.4) and the T CD4-cell count was 236/mm3 (11%).
On resumption of the questioning the patient reported having unprotected sex. Antiretroviral Therapy (ART) was initiated and he achieved complete remission of the initial symptoms and his laboratory values resumed to normal levels 2 weeks later.
Discussion
Our patient presented a HSP-like vasculitis revealing HIV infection. ART completely resolved the vasculitis. Many infectious agents including viral, bacterial or fungal agents, or microbial antigens have been reported in the literature to be associated with vasculitis However, a causal relationship has only been firmly established in a few instances of vasculitis [1]. In our patient, many infectious diseases had been ruled out and HIV infection is more likely to be associated with this vasculitis.
The incidence of vasculitis associated with HIV infection is less than 1% [2,3]. HIV-associated vasculitis can affect vessels of various sizes but most HIV-infected patients develop smallsized- vessel vasculitis [4,5].
The HSP is a systemic disorder characterized by leukocytoplastic vasculitis involving small vessels of the skin, gastrointestinal tract, joints, and kidneys with the deposition of immunoglobulin (Ig)A immune complexes [6]. The pediatric form of the disease is more frequent than the adult form (33 times more common in children than adults) [7]. Only a few reported studies have focused on the disease in adults [8].
Our patient presented two of the four diagnostic criteria of HSP according to the 1990 criteria for the classification of HSP: palpable purpura, less than 20 years of age at disease onset, diffuse abdominal pain, and histologic changes showing granulocytes in the walls of arterioles or venules. The presence of two criteria like in our patient yields a sensitivity of 87.1% and a specificity of 87.7%. Since, there is a risk of misdiagnosis of HSP; Michel and a1 delineated new criteria in 1992. Based on these criteria, the present case had 4 criteria (palpable purpura, gastrointestinal bleeding, hematuria and absence of medications). The presence of 3 criteria or more yields a correct classification of Henoch-Schonlein purpura cases of 87.1% [9].
HSP in adults can reveal or be associated with HIV, few cases have been reported [10-16]. The pathogenesis of HSP in patients with HIV infection remains hypothetic. The role of increased circulation of immune complexes associated with the HIV infection or local replication of HIV itself has been suspected but never demonstrated. HIV infection causes polyclonal hypergammaglobulinemia with a particular elevation of IgG and IgA. Hypergammaglobulinemia is hypothesized to result from chronic antigenic stimulation leading to B-cell hyperplasia [17,18]. A high plasma viral load and a decreased CD4 count were mentioned recently by Isnard et al., viral load varied between 4.5 and 7.9 log/mL and the median CD4 count reported 337 cells/mm3 (range 30/mm3 to 462/mm3) [9-15].
HSP in adults is usually severe and require aggressive therapy. Steroids, other immunosuppressive treatment with azathioprine or cyclophosphamide, therapeutic plasma exchange, and more recently rituximab are used without definitive evidence of effectiveness [19].
The treatment of HSP in HIV infected patients is not well codified and it is based on case reports. The use of ART was efficacious leading to disappearance of cutaneous articular and abdominal signs in some reported cases [12,15,16]. Complete remission of our patient after ART can also support the above mentioned pathogenic mechanism of HSP in HIV infection (increased circulation of immune complexes and local replication of HIV). Therefore, Zaid et al. reported a case report with HSP associated with adult HIV infection after ART treatment. The pathogenesis of HSP in that case was not very well understood. The patient developed a Clostridium difficile associated diarrhoea and cytomegalovirus colitis and died after plasma exchange with haemodialysis and embolization [13]. It’s important to mention that it is possible that the HSP can be resolved over time by itself and the timeline happens to coincide with ART therapy initiation.
Conclusion
Our patient presented a HSP-like vasculitis revealing HIV infection. The Treatment of HSP in HIV infected patients is not well codified. Complete remission of our patient after ART supports the pathogenic mechanism of HIV infection.
References
- Teng GG, Chatham WW. Vasculitis related to viral and other microbial agents. Best Pract Res Clin Rheumatol. 2015; 29: 226?43.
- Guillevin L. Vasculitides in the context of HIV infection. AIDS Lond Engl. 2008; 22: S27-33.
- Satta R, Biondi G. Vasculitis and infectious diseases. G Ital Dermatol E Venereol Organo Uff Soc Ital Dermatol E Sifilogr. 2015; 150:211?20.
- Gisselbrecht M, Cohen P, Lortholary O, et al. HIV-related vasculitis: clinical presentation and therapeutic approach on six patients. AIDS Lond Engl. 1997;11:121?3.
- Chetty R. Vasculitides associated with HIV infection. J Clin Pathol. 2001; 54: 275?8.
- Sheth K, Bockorny M, Elaba Z, et al. Adult Onset Henoch-Schönlein Purpura: Case Report and Review of Literature. Conn Med. 2015; 79: 81?5.
- Piram M, Mahr A. Epidemiology of immunoglobulin. A vasculitis (Henoch-Schönlein): current state of knowledge. Curr Opin Rheumatol. 2013; 25: 171?8.
- Uppal SS, Hussain MA, Al-Raqum HA, et al. Henoch-Schönlein?s purpura in adults versus children/adolescents: A comparative study. Clin Exp Rheumatol. 2006; 24: S26-30.
- Michel BA, Hunder GG, Bloch DA, et al. Hypersensitivity vasculitis and Henoch-Schönlein purpura: a comparison between the 2 disorders. J Rheumatol. 1992; 19: 721?8.
- Hidaka H, Okada T, Matsumoto H, et al. Henoch-Schönlein purpura nephritis in a patient infected with the human immunodeficiency virus. Nihon Jinzo Gakkai Shi. 2003; 45: 387?92.
- Braun S, Ramaker J, Dippel E, et al. Schonlein-Henoch purpura associated with hepatitis B in a patient with HIV infection. Dtsch Med Wochenschr 2001; 126:103?7.
- Bunupuradah T, Puthanakit T, Pancharoen C, et al. Henoch-Schönlein purpura and thrombocytopenia after planned antiretroviral treatment interruption in a Thai girl with HIV infection. Int J Infect Dis IJID Off Publ Int Soc Infect Dis. 2009; 13:e31-33.
- Zaid M, Tan K, Smitasin N, et al. Henoch-Schönlein purpura associated with adult human immunodeficiency virus infection: case report and review of the literature. Ann Acad Med Singapore. 2013; 42: 358?60.
- Saito A, Okiyama N, Maruyama H, et al. Immunoglobulin: A vasculitis associated with HIV infection. J Dermatol. 2016; 43: 444?5.
- Isnard C, Fardet L, Duriez P, et al. Henoch-Schönlein purpura-like vasculitis revealing HIV infection. Med Mal Infect. 2016; 46: 322?5.
- Brandy-García AM, Santos-Juanes J, Suarez S, et al. Vasculitis IgA como forma de presentación de la infección por el virus de inmunodeficiencia humana. Reumatol Clínica. 2018.
- Doria-Rose NA, Connors M. Antibody-secreting B cells in HIV infection. Curr Opin HIV AIDS. 2009; 4: 426?30.
- Soong J, Riley R, Mcpherson R. Oligoclonal Bands of Immunoglobulins in Serum Leading to Diagnosis of Human Immunodeficiency Virus 1 Infection. Am J Clin Pathol. 2016; 145 :277?81.
- Hamilton P, Ogundare O, Raza A, et al. Long-Term Therapeutic Plasma Exchange to Prevent End-Stage Kidney Disease in Adult Severe Resistant Henoch-Schonlein Purpura Nephritis. Case Rep Nephrol. 2015; 269895.