Review Article - Asian Journal of Biomedical and Pharmaceutical Sciences (2022) Volume 12, Issue 86
Exploring unconventional virulence factors of Bacillus anthracis.
Vatika Gupta*, Kanika Jain, Anshu Malik, Rakesh Bhatnagar
Molecular Biology and Genetic Engineering Laboratory, School of Biotechnology, Jawaharlal Nehru University, New Delhi, India
- Corresponding Author:
- Vatika Gupta
Molecular Biology and Genetic Engineering Laboratory
School of Biotechnology, Jawaharlal Nehru University
New Delhi, India
Tel: +91-9953236585
E-mail: vatikagupta12@gmail.com
Received: 01-Feb-2022, Manuscript No. AABPS-22-53003; Editor assigned: 02-Feb-2022, Pre QC No. AABPS-22-53003(PQ); Reviewed: 16-Feb-2022, QC No. AABPS-22-53003; Published: 23-Feb-2022, DOI:10.35841/2249-622X.86.106
Citation:Vatika G, Kanika J, Anshu M, et al. Exploring unconventional virulence factors of Bacillus anthracis. Asian J Biomed Pharmaceut Sci. 2022;12(86):106
Abstract
The surprising correlation between sporadic anthrax breakouts and global warming has raised concern among health authorities of several geographical regions worldwide. The permafrost harbors dormant Bacillus anthracis bacteria causing anthrax. The bacilli possess numerous mechanisms to infect and survive inside the host. To suppress the host immune system, it employs the classical virulence factors: anthrax toxins (lethal & edema toxins) and anti-phagocytic capsule. Although these are primary factors for cytotoxicity and systemic spread, other secreted and nonsecreted factors are also critical to initiate and establish the disease. These secondary factors are non-classical virulence factors of B. anthracis. A plethora of such factors exist including— chaperones, ABC transporters, proteases, chitinases, siderophores, and surface proteins. The non-classical virulence factors are crucial for host-microbe molecular interactions required for pathogenesis. These factors are considered promising candidates for the development of new avenues for diagnostics and therapeutics against anthrax. While many review articles hitherto focused on the classical virulence factors, the literature lacks a comprehensive review detailing the virulence mechanism and therapeutic relevance of non-classical factors. Indeed, this article serves as a resource for comprehensive information about these ancillary virulence factors of B. anthracis with an emphasis on their mechanism of action. Moreover, the article provides insight into anthrax management with respect to each factor. We anticipate paving way for new ideas for prophylactic treatment in the event of future global warming related anthrax outbreaks.
Keywords
Anthrax, Bacillus anthracis, Virulence factors, Proteases, ABC transporters.
Introduction
Climate change poses an unprecedented threat to human existence being a predominant cause for the resurfacing of infectious diseases [1]. Release of anthrax spores from the thawed permafrost was recently reported in Russia and other geographical regions causing the death of several animals [2]. The circumpolar north region has lately witnessed culling of more than 2000 reindeer and the death of a human due to an anthrax outbreak [3]. The warming temperatures in the arctic northern latitudes create suitable geographic conditions for an anthrax outbreak and put the pastorial communities at great risk [4]. Other factors such as soil properties (nutrient composition, alkalinity, type and moisture content), humidity and ambient temperature promote the viability of its spores in wider geographical areas. Anthrax is endemic in Russia [5], high ranked priority zoonotic disease in Kenya, Uganda and disease of important public health in other sub-Saharan Africa [6]. Anthrax is caused by Gram-positive, spore forming bacteria, Bacillus anthracis and the disease is prevalent since biblical times and continues to challenge public health authorities in the modern world. Owing to its extremely resistant spore, it is considered a highly potent bioweapon. Ever since the use of anthrax spores in the bioterror attacks of USA in 2001[7], it is considered a threat to human life.
The prophylactic management of anthrax is to vaccinate people with high risk of exposure. However, the licensed vaccines— Biothrax and AVP— lack a defined composition, contain anthrax toxins (cause reactogenicity), and have a cumbersome dosing schedule. Moreover, hundreds of adverse events are reported for these vaccines that jeopardize its mass administration. The post-exposure therapy with antibiotics is dependent on timely diagnosis of the disease and immediate administration. The early symptoms of anthrax resemble common cold and the common diagnosis methods are not ideal for rapid detection. The present limitations of the diagnostic methods and therapies to treat anthrax intensify the need to better understand the pathogenesis of B. anthracis.
The perennial spores of B. anthracis are the main infectious agent and enter the host via cutaneous, gastrointestinal, or inhalation routes, where they germinate to rapidly dividing vegetative cells [7]. Upon germination, bacteria express its virulence factors, anthrax exotoxins and capsule encoded by plasmids pXO1 and pXO2 respectively [8]. The exotoxins constitute lethal factor (LF), edema factor (EF) and protective antigen (PA) along with the capsule [8]. The infectious cycle is primarily initiated when PA aids the translocation of LF and EF into the host cell. Once inside the cell, LF, a zincdependent metallo protease, inactivates kinases and causes cell apoptosis. EF is a calmodulin-dependent adenylate cyclase which affects the balance of cAMP homeostasis and in turn helps bacteria to evade host immune system [8]. Poly- D-glutamic acid capsule shields bacteria from phagocytosis [9]. Action of these exotoxins at multi spatial levels helps in systemic spread of the disease and is considered main culprits for the disease pathology & high morbidity rates. However, recent in silico studies propose the presence of other proteins that can be essential for anthrax pathogenesis [10, 11]. A large number of extracellular proteins encoded by B. anthracis are proven virulence determinants and potential vaccine candidates such as chaperone HtrA, superoxide dismutase, MntA (manganese transporter), siderophores, proteases [12- 14]. Additionally, surface proteins present on B. anthracis including S-layer protein (EA1), BslA and Isd proteins are also regarded as prospective virulence factors [15]. The striking homology of these proteins with the virulence factors from other pathogens suggests their instrumental role in the development and progression of anthrax.
The quest for a complete understanding of its pathogenic mechanism for the development of better treatment modalities has garnered interest of researchers. This review attempts to summarize the non-conventional virulence factors in B. anthracis pertaining to their functional role for survival, adaptation, proliferation, and infection inside the host. Exhaustive research is needed to fill the knowledge gap about their mode of action, immunogenic potential, and suitability for developing inhibitory molecules. We have highlighted the key areas unexplored for each of these factors for advancements in which would safeguard against threat for bio warfare.
Non-classical virulence factors
For decades, anthrax research primarily focused only on exotoxins and capsule to understand the host-pathogen interactions and develop therapeutics. Recent research shows that other factors also participate in the infection cycle. Such virulence factors of B. anthracis are delineated in Table 1 broadly categorized based on their functional roles.
| Non-classical virulent factors | Functional category | Localization | Function (s) | Immunogenic potential in BA |
|---|---|---|---|---|
| pXO1-130 (AdcA) | Transport | Membrane | Zn uptake and virulence | Yes [31]. |
| Serine protease (HtrA) | Protein folding, stress response | Cytosol/Secreted | Maintenance of protein conformation, membrane and stress and virulence | Yes. |
| Heat shock proteins (DnaK and GroEL) | Protein folding, stress response | Cytosol | Protein repair, invasion, proliferation and stimulate immune response. | Yes[49] |
| Endopeptidase (NlpC/P60) | Cell wall hydrolysis | Membrane | Cell wall hydrolases, cell growth, Sporulation (B.anthracis) | Yes [91] |
| Enolase (Eno) | Metabolism | Membrane | Spores germination, Cell Adhesion and virulence | No |
| Gamma phage receptor (GamR) | Transport | Membrane | Nutrient uptake and ecological adaptation | No |
| Lipoprotein (VanW) | Cell envelope | Membrane | Antibiotic resistance, chemotaxis (B.anthracis) | No |
| Lipoprotein diacylglyceryltransferase (Lgt) | Cell envelope | Membrane | Spores germination, TLR2 based immune response and virulence | Yes [92]. |
| Carboxypeptidase (VanY and LdcB) | Cell envelope | Membrane | Antibiotic resistance, peptidoglycan degradation, maintain cell shape, immune signaling and virulence | No |
| ABC transporters (MntA) | Transport | Membrane | Uptake of nutrients, protection against oxidative stress, virulence | Yes [31]. |
| S-layer proteins (Sap, EA1 and Bsl) | Cell envelope | Membrane | Adhesion and invasion to host cell, Protection from phagocytosis and virulence | Y [31]. |
| Iron-regulated surface determinant (IsdC, IsdK, IsdJ) | Transport | Membrane | Iron acquistion, adhesion to platelets, bacterial growth | No |
| Proteases (InhA1, NprB, Camelysin, TasA and ClpX) | Protein degradation | Secreted | Degradation of host extracellular layer and immune response, acquistion of nutrients, process and stabilize virulence factors, virulence | Yes [31]. |
| Nitric oxide synthase | Metabolism | Cytosol | Protection against oxidative stress and antibiotics action and virulence. | No |
| Sulfatase (YvgJ, YflE) | Cell envelope biogenesis | Secreted | Host cell adhesion and invasion, cell envelope biogenesis | No |
| Superoxidase dismutase (SodA-2) | Detoxification, oxidative stress response | Cytosol | Protection against oxidative stress, inhibit host immune response, Spores structure maintenance (B. anthracis), virulence | No |
| Chitinase | degradation of polysaccharides | Membrane/Secreted | Host cell invasion, toxin activation (B. thruringiensis), nutrient acquistion (B. anthracis) | No |
| Nucleotidase | Metabolic enzyme | Membrane/Secreted | Impairment of host immune responses, prevent platelet aggregation | No |
| Peptidases (BA1449 and BA0165) | Degradation of proteins | Secreted | Collagen degradation, penetration into host cell, virulence | No |
| Siderophores (Petrobactin and bacillibactin) | Iron-chelating agent | Secreted | Survival in iron-restricted environment, virulence | No |
| Anthrolysins | Cytolysins | Secreted | Degradation of host cell, invasion in cell and virulence (B. anthracis) | Yes[65]. |
BA: Bacillus anthracis Vollum strain [12].
Table 1. Overview of the non-classical virulent factors of B. Anthraci.
Nutrient Uptake
Proteases
Proteases are well established virulence factors in many pathogens that hydrolyze host matrix proteins and degrade immune molecules and avails— nutrient acquisition, invasion, and host evasion [16]. B. anthracis encodes an array of proteases hypothesized to perform crucial functions in pathogenesis [17,18].
Among these, Immune inhibitor A1 (InhA1) and neutral protease B (NprB) extensively degrade the host extracellular matrix and promote cellular adhesion during infection [19]. InhA1 and NprB also assist bacilli to cross blood-brain barrier by proteolyzing zonula occulden (ZO-1) protein present in the tight junctions [20]. They aid in the acquisition of essential nutrients by proteolysis of hemoglobin [19] and together, they account for 80-90% of B. anthracis secretome [21]. Interestingly, deletion of these proteases from B. anthracis cause degradation of exotoxins PA, EF and LF and attenuate its virulence [22]. InhA also controls expression levels of other proteins such as BslA protein, ABC transporters, chaperones, sulphates and other proteases [23]. It also affects sporulation by regulating proteins involved in the digestion of chitin present in the soil [22]. Thus, InhA is crucial for the progression of anthrax.
Another protease found in the secretome of B. anthracis is camelysin. It shares homology with surface metallo protease camelysin of B. cereus and Cyt2Ba of B. thuringiensis [22]. In B. anthracis, camelysin degrades InhA1 and maintain stable levels of protective antigen in the culture supernatant. Hence, it plays an imperative role in the pathogenesis of B. anthracis [24].
ClpX is another virulent protease that assists in proper protein folding [25]. Post infection ClpX expression determines the viability and lethality of B. anthracis by degrading host cathelicidin peptides important component of innate host defense mechanism. In absence of ClpX, bacilli become more susceptible to the action of cathelicidin and other antimicrobial peptides. [26]. Recent microarray analysis with ClpX- deficient strains confirmed that ClpX affects the expression of 119 genes mostly involved in metabolic, transport or regulatory functions in B. anthracis [27].. Effective neutralization of B. anthracis ClpX activity could be a potential way to directly kill the pathogen and thereby treating anthrax
Peptidases
Peptidase is an enzyme that primarily breaks down a peptide sequence into individual amino acids. Peptidases of pathogenic organisms support their virulence via contributing in facilitating variety of functions like host-pathogen interactions, regulation of gene expression etc. Tc80 propyl oligo peptidase in Trypanosoma cruzi hydrolyses the host fibronectin to facilitate its penetration for the infection [28]. B. anthracis also secretes such peptidases —propyl oligo peptidase BA0165and peptidase M23/M37 (BA1449) [12]. Role of these peptidases in pathogenicity of B. anthracis is yet unknown.
Chitinase
A glycosyl hydrolase (a Chitinase that mediates the depolymerisation of chitin) is present in bacteria, arthropods, yeast, fungi, plants and humans. Pathogens utilize Chitinase to disrupt host’s chitinaceous structures to facilitate invasion [29]. During aerobic metabolism, B. anthracis also secretes high levels of multiple Chitinase. These levels decrease when the concentration of CO2/bicarbonate increases in the host environment [12]. This indicates the possible role of chattiness in the survival of B. anthracis in soil. Chitinase levels are also affected by the change in expression of InhA1 metallo protease. Chitinase is a putative substrate for InhA1 and thus, may play an important role in nutrient acquisition by B. anthracis. Thus, InhA modulates the survival and sporulation of the bacteria by changing the levels chattiness secreted in the environment [22]. Further research to determine the function and regulation of Chitinase in B. anthracis is required to ascertain its role in pathogenesis.
ABC transporters
(BA1191, BA0656, BA0855, BA1197, BA0855, BA0908, BA5220, BA3645, and BA3189)
ATP-binding cassette (ABC) transporters are ubiquitous proteins that enable organisms to survive in diverse environmental conditions. In bacteria, solute binding proteins (SBP) is the subunit of ABC transporter that facilitates the delivery of incoming alacrities [30]. ABC transporters in the pathogenic bacteria are involved in the uptake of essential nutrients and metal ions indispensable for growth and survival. Interestingly, B. anthracis encode approximately 55SBPs of ABC transporters of which 25% are immunogenic and include BA0175, BA0314, BA2848, BA3189 (MntA) and Fe compound binding transporters (BA4597, BA4766) [31]. Recently, BA1191, BA0656, BA0855, BA1197, BA0855, BA0908, BA5220, BA3645, and pXO1-130 are also identified as immunogenic [31].
MntA is the most extensively studied SBP which is required for manganese uptake. It shares homology with Pneumococcal surface antigen A (PsaA) of S. pneumonia that protects the bacteria against oxidative stress [32]. In B. anthracis, MntA plays several roles ranging from growth to protection of bacteria from oxidative stress created by the host immune cells [33,34]. ABC transporters of B. anthracis use siderophores to acquire higher uptake of iron. The photo reactive catechol ate siderophores, petro bactin, determines the survival of B. anthracis in host macrophages [35]. Considering the active participation of SBPs in pathogenesis of anthrax, other SBPs must be characterized, and their immunogenic potential should be validated as candidates for therapeutics and diagnostics.
pXO1-130
pXO1-130, a lipoprotein encoded by the virulence plasmid pXO1, was identified as potential anthrax vaccine candidates owing to its high immunogenicity [10]. pXO1-130 is homologous to AdcA, an SBP transporter involved in zinc uptake in bacteria [10,36]. In pathogens like Brucella, AdcA is linked with virulence [37]. These proteins help in intracellular growth by increasing zinc uptake and utilization. Interestingly, in B. anthracis, the pXO1-130 is elevated at 37°C during the onset of stationary phase [38] that also favors the expression of lethal factor (zinc-dependent metallo protease). This signifies the importance of zinc and its uptake in B. anthracis during pathogenesis [39]. Although these studies implicate the role of pXO1-130 in B. anthracis lifecycle, further research is required to define its precise role and application in anthrax management.
Gamma phage receptor (GamR)
GamR is a bacterial cell wall anchored protein which is usually involved in binding with the phages [40]. In B. anthracis, GamR is identified as a LPXTG (a conserved motif in cell surface proteins) protein bound to its cell wall with the help of sortase A. Sortase catalyses covalent anchoring of LPXTG-harboring proteins to the peptide component of peptidoglycan GamR is involved in binding of B. anthracis with γ phage which contains fosphomycin- resistance protein, soil antibiotic resistance mode. This binding interaction plays a significant role in the survival of vegetative cells of B. anthracis in the soil thereby promoting its ecological adaptation [41].
Iron-regulated surface determinant (Isd)
Pathogenic bacteria require essential nutrients such as iron to survive inside the host cell. Most of the iron molecules inside the mammalian host are sequestered in the porphyrin heme often bound to hemoglobin. Gram-positive bacteria express several surface proteins for transportation of extracellular heme reservoir to intracellular iron-dependent pathways [42]. These proteins are generally iron-regulated surface determinant (IsDs) proteins and work along with secreted homophobes (scavenge heme from hemo proteins) [42]. IsDs by acting as an iron uptake system facilitate survival and virulence of many pathogens like B. cereus (IlsA) and Aureus (IsdB and IsdA). IsdB promotes adhesion of bacteria to platelets and IsdA protects cells from bactericidal lipids [43,44]. B. anthracis produces three different type of IsDs (IsdC, IsdK, and IsdJ) containing NEAT (Near Transporter; bind and transport heme) domain proteins, which remove heme from the haemoglobin of the host cell and acquisition of iron required for bacterial growth [45]. We speculate that suppression of these iron-regulated surface proteins will inhibit iron-regulated metabolic pathways and are expected to suppress virulence.
Host Invasion
DnaK (Hsp70) and GroEL (Hsp60)
Heat shock proteins (HSPs) are actively synthesized during stress conditions and assist in the repair of damaged proteins [46]. GroEL mediates protein folding while DnaK protects the mis folded protein from proteolysis cleavage [47]. Pathogenic bacteria up regulate expression of these HSPs that enables their survival upon encountering a hostile environment in the host. In B. anthracis, GroEL is adsorbed on the exosporium and DnaK is a component of spore which imparts those potential antigenic properties [48]. DnaK and GroEL are indeed immunogenic and provide significantly high protection against anthrax infection [49]. Therefore, these proteins are potential vaccine candidates and further research may advocate their use in conjugated vaccine against anthrax.
S-layer proteins
(Sap, EA1and Bsl)
Many pathogenic bacteria have a proeteinacous protective layer on their surface, commonly known as S-layer. S-layer comprises of specific motifs referred as S-layer homology (SLH) which interact with secondary cell wall polysaccharide to mediate their assembly on the bacterial S-layer. S-layer maintains cell shape, protects bacteria from its environment and facilitates association with the host. [15]. B. anthracis encodes 22 SLH proteins and 50% of them are immunogenic in nature [50]. Expression of these proteins is regulated by levels of CO2.
Surface array protein (Sap) and extracellular antigen 1 (EA1) are the most widely studied SLH proteins that bind with the cell envelope and anchor surface proteins) to the host surface [15]. Vegetative form of B. anthracis produces more Sap S-layers while encapsulated bacilli produce EA1 [15]. Deposition of Sap ad EA1 in the S-layer also facilitates chain formation of partially separated vegetative cells of B. anthracis, thus provide resistance to phagocytosis [51]. Recently, Nano bodies were shown to inhibit S-layer domain of SAP and thereby the growth and pathology of B. anthracis [52].
Bacillus S-layer associated proteins (Bsl) are immunogenic and contain SLH domains. A BslO attack the linkage septal zone between the daughter cells thereby catalyzes the separation of daughter cells [53]. Spores with mutated BslA exhibit delayed replication and decreased dissemination of bacteria within the host [15]. Evidently, pathogenic organisms depend on S-layer associated proteins to invade the host and escape phagocytosis [15]. Additional information about its incorporation/deposition mechanism into cell envelope and role in virulence establishment will help in anti-anthrax therapy development.
Enolase
Enolase is a remarkably conserved enzyme involved in glycolysis and gluconeogenesis pathways [54]. Enolase -deficient bacterial cells lack sporulation activity and encounter a long lag phase in ATP production during germination [55]. Enolase has been found on the cell surface of some bacterial and fungal pathogens such as Leis mania, Trypanosoma brucei and T. cruzi and also controls their virulence and viability [54]. Similar to other pathogens, Enolase is present on the outer surface of B. anthracis where it interacts with plasminogen on the host surface and facilitates the entry of the bacilli into the host. [56]. In B. anthracis, overproduction of Enolase decreases spore germination [57]. Thus, Enolase is crucial for survival in nutritional stress, maintenance of germination and invasion of B. anthracis into the host cell. Its potential role in virulence can be exploited for the development of drug targets if bacterial enzyme selectivity could be achieved.
Sulfatase
(BA5470, BA2947 and BA1436)
Sulfatase catalyses the hydrolysis of sulfate esters present in the biological reactions. Its substrates vary from small molecules like steroids to large complex cell layer carbohydrates. Sulfotransferases and sulfatases regulate hostpathogen interactions possibly by enzymatic exposure of the adhesion sites [58]. Opportunistic pathogens, P. aeroginosa and Burkholderia cepacia, invade lung tissues by eliminating the protective sulfate groups from the mucin-binding motifs using sulfatases like mucin-desulfating Sulfatase MdSs enzymes [59] Sulfatases modify their binding sites on the host membrane which in turn facilitate the efficient infection of pathogens like Yersinia pestis, B. anthracis, and Streptococcus agalactiae [60]. Extracellular proteome analysis of B. anthracis revealed that sulfatases are highly expressed proteins in its secretome [12]. Annotated sulfatases —BA5470, BA2947 and BA1436—are involved in cell envelope biogenesis [12]. Although the exact role of these sulfatases is yet to be deciphered, the studies from other pathogens suggest a connection between sulfatases and pathogenicity.
Anthrolysins
Anthrolysins is a member of the highly conserved protein family— cholesterol-dependent cytolysin (CDC) — that generally invades host membrane. Its Interaction with cholesterol moieties present in animal membrane is sufficient to create large pores that ease the penetration of large toxins into the host [61]. Cytolytic and penetration properties of CDCs are conserved across the genome of both pathogenic and non-pathogenic Gram-positive organisms. Streptomycin O, listeriolysin, perfringolysin, and Pneumolysin are some widely known thiol-activated toxins of this group secreted by S. pyogenic, L. monocytogenes, C. perfringens, and S. pneumonia respectively [61]. Anthrolysins (ALO) share high homology with listeriolysin O [62].
Like other CDCs, Anthrolysins, secreted by B. anthracis, majorly contribute to its haemolytic activity and facilitate escape from the host cell. During pathogenesis, it is essential for the disruption of gut epithelial layer thereby passage of vegetative cells [63]. It also enables the release of toxins which are otherwise bound in membrane vesicle [64]. Immunization with both haemolytic and non-haemolytic variants of ALO protects against lethal infection [65]. Moreover, incorporation of monoclonal antibodies against Anthrolysins O showed enhanced survival rate in B. anthracis infected mice [66]. Anthrolysins exist as a monomer, unlike other CDCs which exist as a dimer or higher oligomeric state [67]. This structural diversity could be linked to the yet unexplored role in B. anthracis survival and pathogenesis, sketching the scope of more useful findings on this subject.
Stress Tolerance
High temperature requirement a (HtrA)
HtrA are heat shock serine proteases which are structurally and functionally conserved in both prokaryotes and eukaryotes. HtrA exhibits dual biological activities of chaperones and proteases, thus regulates protein quality in cell [68]. In addition, it prevents accumulation of mis folded proteins helps in coping stress, and enables penetration in the host by cleavage of the extracellular matrix and cell adhesion proteins such as cadherin, occulden, fibronectin, and proteoglycans [69]. Various pathogens deploy HtrA for infection, including —Yersinia enterocolitica, Shigella flexneri, Chlamydia trachomatis, Mycobacterium tuberculosis, haemophilic parasuis, and Helicobacter pylori [68]. Lately, B. anthracis HtrA was identified as an important biomarker for anthrax owing to its presence in the bloodstream of infected animals [70]. Further research showed its role in stress tolerance as it alters the secretion of various starvation-associated genes including neutral protease A (NprA), thereby affects spore germination and proliferation [71]. Proteolytic activity of HtrA is also indispensable for stress resilience, assembly of outer S-layer and virulence of B. anthracis [72]. These significant roles of HtrA make it a suitable candidate for improvisation of the live attenuated vaccine anthrax strain. A live attenuated anthrax spore vaccine based on deletion of the HtrA gene was successfully developed with high protection levels [73]. Incorporation of multiple DNA modifications of such kind in an attenuated strain might decrease the probability of genetic reversion. Advances in this domain could also open avenues for a novel attenuated vaccine strain development.
Vancomycin b-type resistance protein (VanW)
VanW is a lipoprotein which prevents glycopeptide-based antibiotics like vancomycin from inhibiting the assembly of bacterial cell wall. VanW replaces D-Alanine in the usual peptidoglycan cell wall with the D-lactate imparting resistance to antibiotics [74]. In B. anthracis VanW lipoprotein is also implicated in chemo taxis [75]. Many tandem repeats of the chemo taxis protein gene are found in other pathogenic species like Xanthomonas [76]. Further studies are required to explore its role in the pathogenesis of anthrax.
Vany- d-alanyl-d-alanine Carboxypeptidase
Vancomycin attacks N-Acyl-D-Ala-D-Ala linkage in the cell wall to prevent peptidoglycan formation. Bacteria have evolved multiple enzymes that protects from antibiotics. Amongst them, VanY functions as DD-Carboxypeptidase and DD-carboxyesterase, and cleaves D-alanine residue of the Uridine diphosphate muramyl pentapeptide (UDP), to eliminate the antibiotic target from the bacterial surface [77]. LD-Carboxypeptidase B (LdcB), a protein characterized from S. pneumonia, B. subtilis, and B. anthracis, play a vital role in the recognition of peptidoglycan. LdcB is vital for correct cell wall synthesis and thereby plays significant part in cell viability and virulence of pathogen. Targeting these carboxyl peptidases might weaken the protective shield of bacteria, making the cells more prone to antibiotics [78].
Nitric oxide synthase
Nitric oxide (NO) is a highly reactive free radical synthesized by nitric oxide synthase (NOS) by oxidizing L-Arginine. NOS are present in both mammals (mNOS) and bacteria (bNOS). BNOS protects bacteria from oxidative stress, detoxify antimicrobials and modulates various macromolecules, specifically the ones involved in toxin biosynthesis, oxidative stress repair, and radiation damage regulation [79]. NOS in the pathogens Staphylococcus aureus and Bacillus anthracis synthesize NO, activate catalase, and halt Fenton chemical reaction to protect them from oxidative stress inside macrophage [79, 80]. Moreover, these pathogens use bNOS to escape the antibacterial action of various antibiotics [81]. B. anthracis strain lacking bNOS proteins reduces virulence in mouse by affecting viability in macrophages [80, 82]. These results indicate the role of bNOS in the survival of bacterial pathogens in the host oxidative environment and suggest its potential implication in anthrax treatment.
Superoxide dismutase (SOD)
SODs are metallo enzymes which catalyse the dismutation of superoxide radical (O2·−) into hydrogen peroxide and molecular oxygen. The scavenging activity of SODs prevents oxidative damage to biomolecules from reactive oxygen species (ROS). These enzymes are highly conserved in all aerobic and some anaerobic organisms [83]. SODs are differentiated on the basis of their metal cofactors and are commonly categorized as copper-zinc, manganese or iron, and nickel SOD. Gene’s sodA, sodB, and sodC encode Mn- SOD, Fe-SOD, and Cu/Zn-SOD respectively [84].
SODs contribute to a major defense mechanism in various animal pathogens— Bordet Ella spp., Brucella abortus, Shigella Flexner, Salmonella enterica serovar typhimurium, Staphylococcus aureus, Yersinia enterocolitica, Neisseria meningitides, Haemophilic influenza, and Streptococcus pneumonia [85].
B. anthracis encounters oxidative environment inside host and in the soil [86] therefore, protection against oxidative stress is imperative to its survival. B. anthracis genome encodes four SODs: SODA1, SOD15, SODC and SODA2. Proteomic studies confirm the presence of two SODs— SODA1 and SOD15—in B. anthracis spores. SODA1 shares highest homology (~77%) with sodA enzyme of B. subtilis and protects against endogenous superoxide stress [13]. Thus, SODA1 supports the survival of B. anthracis during aerobic conditions. B. anthracis sodA1 strain decreases the mortality in mouse model remarkably [13]. SOD15 is presumed to maintain cell morphology. SOD15 and SODA1 also determine the vigor of B. anthracis during lung infection. SODA2 forms an active heterodimer with SODA1and that protects B. anthracis from antioxidants. Although sodC gene also transcribes actively, but more research is needed to determine it’s a significant function [13]. Cybulski et al. created a 40-fold attenuated strain of B. anthracis carrying sod15 sodA1 sodC sodA2 mutations in mice model. Thus, expression of SODs in B. anthracis is worth exploring for developing a treatment against anthrax.
Siderophores
Siderophores are high-affinity iron chelating compounds present in bacteria and plants that scavenge insoluble Fe3+ complexes from foreign sources and transform it to a soluble complex to facilitate its transportation. Siderophores are classified into different groups based on the ligands involved in chelating the ferric iron. Catecholate (e.g., Enterobactin, Bacillibactin), hydroxamates (eg: Ferrochrome, Desferrioxamine B) and carboxylates are some examples of such groups [87]. Pathogenic bacteria secrete several siderophores that allow them to proliferate in iron-deficient atmosphere inside host cell [88].
B. anthracis contains two catecholate siderophores differing in their catechol hydroxylation patterns [88]. First is petrobactin (uses 3,4-dihydroxybenzoyl as a chelating compound) and second is Bacillibactin (carries 2,3-dihydroxybenzoyl (2,3- DHB) catechol units) [88]. Bacillibactin are synthesized by a five gene operon bacACEBF, while petrobactin are encoded by asbA and asbB genes [88]. Single deletion of either of them significantly reduces catechol secretion in B. anthracis [14]. Besides their role in petrobactin synthesis, AsbA and AsbB proteins also facilitate growth and virulence of B. anthracis in macrophages [14]. Thus, siderophores are crucial for B. anthracis pathogenesis and could become key targets to inhibit infection.
Sporulation
NlpC/P60 Endopeptidase
N1pC/P60 end peptidase are a large protein family comprising of domain folds similar to the papain-like peptidases, trans glutaminases and aryl-amine acetyl transferase [89]. They act as cell wall hydrolases in several bacteria and control vital functions like: peptidoglycan formation for cell growth and division, host invasion, and autolysis [90]. NlpC/P60 end peptidase is exclusively found in the secretome of B. anthracis from infected animals and hence is a potential biomarker of the disease [70]. NlpC/P60 contains one catalytic domain and three Src homology (SH3b) domains, associated with maintenance of cell wall dynamics (in vegetative and spore forms) [91]. Additional research is required to NlpC/P60 in B. anthracis to delineate its involvement in the pathogenesis of B. anthracis.
Lipoprotein diacylglyceryl transferase (Lgt)
Lipoproteins are essential for bacterial cell surface for dispersal and germination of the spores. Knockout studies of lgt (BA5391) gene (a lipoprotein synthesizer) in B. anthracis revealed the role of lipoproteins in the various processes such as spores germination, and generation of TLR2 based immune response [92]. Lgt attaches the pro lipoproteins to lipid anchor presenting it to the cell surface. Deletion of Lgt affects lipoprotein synthesis, and in turn attenuate virulence in the murine model organism [92]. This indicates the indispensable role of lipoprotein in the survival and virulence of B. anthracis inside the host.
Host Immune Impairment
Nucleotidases
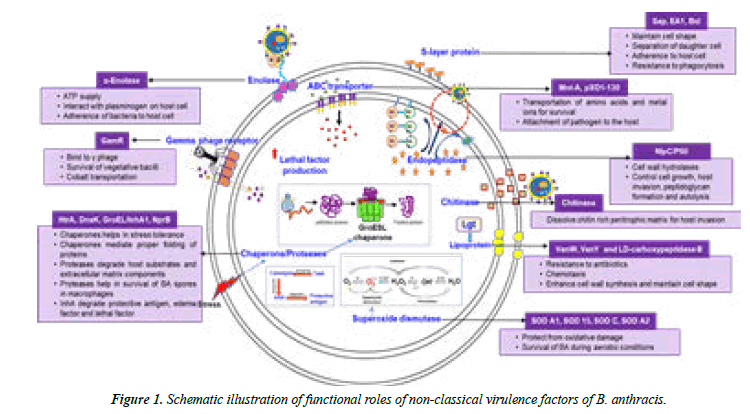
Nucleotidases mediates hydrolytic cleavage of a nucleotide to nucleoside and phosphate. During an infection, cellular damage increase levels of ATP which in turn activates the innate immune response and promotes the release of cytokines [93]. The nucleotidases cleave ATP into adenosine that inhibits the effect of ATP and thereby controls the levels of an inflammatory response [94,95]. Pathogenic bacteria have emerged with the strategy to take advantage of this pathway and encode for several nucleotidases in their extracellular proteome. Staphylococcus aureus expresses membrane anchored enzyme adenosine synthase A (AdsA), which produces adenosine in host blood, to help it escape the host immune responses [96]. Presence in B Anthracis secretome [12] and a familiar connection with infection establishment, demands further analysis of nucleotides in B. Anthracis (Figure 1).
Conclusion
Anthrax is dreadful owing to its high mortality rate (inhalational infection) and plausible weaponization of its spores for global terrorism [7]. The current modalities for its detection and management are based on the classical virulence factors, lethal and edema toxin. Approved vaccines have a gamut of complications which limit their accessibility to the general population [7]. Lately, the post-exposure therapy using antibiotics have concerns due to the development of resistant strains [97]. Inadequacies of the present vaccination program and antibiotics therapy stipulate newer management strategies. Continuous research efforts are conducive to find alternate immunogens for sensitive diagnosis and improved prophylactic and post-exposure control measures.
The plethora of non-classical proeteinacous factors reviewed here plays a significant role in B. anthracis virulence. These molecules exploit various pathways for pathogenesis and enhance toxicity as summarized. Several evidences support their unequivocal role in an infection process and their potency as vaccine candidates. Further studies are required to unravel the mechanism of action of these molecules. Extensive research identifying their precise role in virulence establishment, immune response and their clinical outcomes will substantiate their action in diagnostics and treatment of anthrax. Filling these gaps in knowledge will help generate an inventory of inhibitors against these molecules that may be advantageous in combating anthrax.
Future outlook
The broad implication of the present review is the identification and development of some futuristic therapeutics to tackle anthrax. Interesting questions for future research can be derived from an intense functional characterization of the non-classical virulent factors highlighted in this review and understanding their interaction maps. Further attempts on the toxicity profiling and examining immunogenic response in more realistic settings could prove quite beneficial to the drug development sector. These discoveries will not just fill the void in B. anthracis literature but also disentangle the complexities associated with various pathogenic organisms, as witnessed by the high conservation of these molecules across species.
The functional and immunogenic properties of these factors can be explored in multiple applications such as:
Combinatorial use of these virulent proteins with other antigens for enhancing immunogenic responses. This method has been employed with CDCs secreted by an invasive pathogen, S. pneumonia. Pneumolysin, when used along with other pneumococcal antigens showed an effective response [98].
Bacteriophage based delivery of drugs is another open avenue for anthrax destruction. This methodology has been exploited earlier in Staphylococcus where chloramphenicol drug was penetrated in the pathogen using bacteriophages mediator.
Additionally, these molecules can serve as therapeutics against other pathogens.
(d) DNA-vaccination, protein-antigen based immunization or small-molecules inhibitors- based treatments, are some of the alternatives that could eliminate the dependence on serotypebased vaccines and their associated complications.
Conflict of Interest
None. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Sonne C, Letcher RJ, Jenssen BM, et al. A veterinary perspective on One Health in the Arctic. Acta Veterinaria Scandinavica. 2017;59(1):1-1.
- Timofeev V, Bahtejeva I, Mironova R, et al. Insights from Bacillus anthracis strains isolated from permafrost in the tundra zone of Russia. PloS one. 2019;14(5):e0209140.
- Hueffer K, Drown D, Romanovsky V, et al. Factors contributing to Anthrax outbreaks in the circumpolar north. EcoHealth. 2020;17(1):174-80.
- Walsh MG, de Smalen AW, Mor SM. Climatic influence on anthrax suitability in warming northern latitudes. Sci rep. 2018;8(1):1-9.
- Cherkasskiy BL. A national register of historic and contemporary anthrax foci. J applied microbiol. 1999;87(2):192-5.
- Muturi M, Gachohi J, Mwatondo A, et al. Recurrent anthrax outbreaks in humans, livestock, and wildlife in the same locality, Kenya, 2014–2017. Am j tropical med hygiene. 2018;99(4):833.
- Pohanka M. Bacillus anthracis as a biological warfare agent: infection, diagnosis and countermeasures. Bratislava Med J. 2020;121(3):175-81.
- Pilo P, Frey J. Pathogenicity, population genetics and dissemination of Bacillus anthracis. Infection, genetics and evolution. 2018;64:115-25.
- Leppla SH, Robbins JB, Schneerson R, et al. Development of an improved vaccine for anthrax. J clinic investigation. 2002;110(2):141-4.
- Ariel N, Zvi A, Grosfeld H, et al. Search for potential vaccine candidate open reading frames in the Bacillus anthracis virulence plasmid pXO1: in silico and in vitro screening. Infection and immunity. 2002;70(12):6817-27.
- Ariel N, Zvi A, Makarova KS, et al. Genome-based bioinformatic selection of chromosomal Bacillus anthracis putative vaccine candidates coupled with proteomic identification of surface-associated antigens. Infection and immunity. 2003;71(8):4563-79.
- Chitlaru T, Gat O, Gozlan Y, et al. Differential proteomic analysis of the Bacillus anthracis secretome: distinct plasmid and chromosome CO2-dependent cross talk mechanisms modulate extracellular proteolytic activities. J bacteriol. 2006;188(10):3551-71.
- Passalacqua KD, Bergman NH, Herring-Palmer A, et al. The superoxide dismutases of Bacillus anthracis do not cooperatively protect against endogenous superoxide stress. J bacteriol. 2006;188(11):3837-48.
- Cendrowski S, MacArthur W, Hanna P. Bacillus anthracis requires siderophore biosynthesis for growth in macrophages and mouse virulence. Mol microbiol. 2004;51(2):407-17.
- Missiakas D, Schneewind O. Assembly and function of the Bacillus anthracis S-layer. Annual review of microbiol. 2017;71:79-98.
- Ullán RV, Barreiro C. Bacterial proteases as targets to control bacterial growth. InNew Weapons to Control Bacterial Growth 2016 (pp. 133-159). Springer, Cham.
- Popov SG, Popova TG, Hopkins S, et al. Effective antiprotease-antibiotic treatment of experimental anthrax. BMC infect dis. 2005;5(1):1-4.
- Gupta V, Chaudhary N, Aggarwal S, Adlakha N, Gulati P, Bhatnagar R. Functional analysis of BAS2108-2109 two component system: evidence for protease regulation in Bacillus anthracis. The Int J Biochem Cell Biol. 2017;89:71-84.
- Terwilliger A, Swick MC, Pflughoeft KJ, et al. Bacillus anthracis overcomes an amino acid auxotrophy by cleaving host serum proteins. J bacteriol. 2015;197(14):2400-11.
- Mukherjee DV, Tonry JH, Kim KS, et al. Bacillus anthracis protease InhA increases blood-brain barrier permeability and contributes to cerebral hemorrhages. PLoS One. 2011;6(3):e17921.
- Chung MC, Popova TG, Millis BA, et al. Secreted neutral metalloproteases of Bacillus anthracis as candidate pathogenic factors. J Biol Chem. 2006;281(42):31408-18.
- Pflughoeft KJ, Swick MC, Engler DA, et al. Modulation of the Bacillus anthracis secretome by the immune inhibitor A1 protease. J bacteriol. 2014;196(2):424-35.
- Tonry JH, McNichol BA, Ramarao N, et al. Bacillus anthracis protease InhA regulates BslA?mediated adhesion in human endothelial cells. Cellular microbiol. 2012;14(8):1219-30.
- Pomerantsev AP, Pomerantseva OM, Moayeri M, et al. A Bacillus anthracis strain deleted for six proteases serves as an effective host for production of recombinant proteins. Protein expression and purification. 2011;80(1):80-90.
- McGillivray SM, Ebrahimi CM, Fisher N, et al. ClpX contributes to innate defense peptide resistance and virulence phenotypes of Bacillus anthracis. J innate immunity. 2009;1(5):494-506.
- McGillivray SM, Tran DN, Ramadoss NS, et al. Pharmacological inhibition of the ClpXP protease increases bacterial susceptibility to host cathelicidin antimicrobial peptides and cell envelope-active antibiotics. Antimicrobial agents and chemotherapy. 2012;56(4):1854-61.
- Claunch KM, Bush M, Evans CR, et al. Transcriptional profiling of the clpX mutant in Bacillus anthracis reveals regulatory connection with the lrgAB operon. Microbiol. 2018;164(4):659-69.
- Grellier P, Vendeville S, Joyeau R, et al. Trypanosoma cruzi prolyl oligopeptidase Tc80 is involved in nonphagocytic mammalian cell invasion by trypomastigotes. J Biol Chemistry. 2001;276(50):47078-86.
- Hamid R, Khan MA, Ahmad M, et al. Chitinases: an update. J pharmacy & bioallied sci. 2013;5(1):21.
- Garmory HS, Titball RW. ATP-binding cassette transporters are targets for the development of antibacterial vaccines and therapies. Infection and immunity. 2004;72(12):6757-63.
- Chitlaru T, Gat O, Grosfeld H, et al. Identification of in vivo-expressed immunogenic proteins by serological proteome analysis of the Bacillus anthracis secretome. Infection and immunity. 2007;75(6):2841-52.
- Bajaj M, Mamidyala SK, Zuegg J, et al. Discovery of novel pneumococcal surface antigen A (PsaA) inhibitors using a fragment-based drug design approach. ACS chemical biol. 2015;10(6):1511-20.
- Gat O, Mendelson I, Chitlaru T, et al. The solute?binding component of a putative Mn (II) ABC transporter (MntA) is a novel Bacillus anthracis virulence determinant. Mol microbiol. 2005;58(2):533-51.
- Gupta V, Jain K, Garg R, et al. Characterization of a two component system, Bas1213?1214, important for oxidative stress in Bacillus anthracis. J Cellular Biochem. 2018;119(7):5761-74.
- Zawadzka AM, Kim Y, Maltseva N, et al. Characterization of a Bacillus subtilis transporter for petrobactin, an anthrax stealth siderophore. Proceedings of the National Acad Sci. 2009;106(51):21854-9.
- Hantke K. Bacterial zinc uptake and regulators. Current opinion in microbiol. 2005;8(2):196-202.
- Kim S, Watanabe K, Shirahata T, et al. Zinc uptake system (znuA locus) of Brucella abortus is essential for intracellular survival and virulence in mice. J Veterinary Med Sci. 2004;66(9):1059-63.
- Kim SK, Shahid S, Kim SH, et al. Comparative analysis of virulence factors secreted by Bacillus anthracis Sterne at host body temperature. Letters in applied microbiol. 2012;54(4):306-12.
- Klimpel KR, Arora N, Leppla SH. Anthrax toxin lethal factor contains a zinc metalloprotease consensus sequence which is required for lethal toxin activity. Mol microbiol. 1994;13(6):1093-100.
- Davison S, Couture-Tosi E, Candela T, et al. Identification of the Bacillus anthracis γ phage receptor. J bacteriol. 2005;187(19):6742-9.
- Koehler TM. Bacillus anthracis physiology and genetics. Mol aspects med. 2009;30(6):386-96.
- Gat O, Zaide G, Inbar I, et al. Characterization of Bacillus anthracis iron?regulated surface determinant (Isd) proteins containing NEAT domains. Mol microbiol. 2008;70(4):983-99.
- Zapotoczna M, Jevnikar Z, Miajlovic H, et al. Iron?regulated surface determinant B (IsdB) promotes S taphylococcus aureus adherence to and internalization by non?phagocytic human cells. Cellular microbiol. 2013;15(6):1026-41.
- Miajlovic H, Fallon PG, Irvine AD, et al. Effect of filaggrin breakdown products on growth of and protein expression by Staphylococcus aureus. J allergy clinical immunol. 2010;126(6):1184-90.
- Tarlovsky Y, Fabian M, Solomaha E, et al. A Bacillus anthracis S-layer homology protein that binds heme and mediates heme delivery to IsdC. J bacteriol. 2010;192(13):3503-11.
- Gophna U, Ron EZ. Virulence and the heat shock response. Int j med microbiol. 2003;292(7-8):453-61.
- Lund PA. Microbial Molecular chaperones. Adv Microb Physiol 2001;44:93-140.
- DelVecchio VG, Connolly JP, Alefantis TG, et al. Proteomic profiling and identification of immunodominant spore antigens of Bacillus anthracis, Bacillus cereus, and Bacillus thuringiensis. Applied and environmental microbiol. 2006;72(9):6355-63.
- Sinha K, Bhatnagar R. GroEL provides protection against Bacillus anthracis infection in BALB/c mice. Mol Immunol. 2010;48(1-3):264-71.
- Gat O, Grosfeld H, Ariel N, et al. Search for Bacillus anthracis potential vaccine candidates by a functional genomic-serologic screen. Infection and immunity. 2006;74(7):3987-4001.
- Nguyen-Mau SM, Oh SY, Schneewind DI, et al. Bacillus anthracis SlaQ promotes S-layer protein assembly. J bacteriol. 2015;197(19):3216-27.
- Fioravanti A, Van Hauwermeiren F, Van der Verren SE, et al. Structure of S-layer protein Sap reveals a mechanism for therapeutic intervention in anthrax. Nature Microbiol. 2019;4(11):1805-14.
- Kern VJ, Kern JW, Theriot JA, et al. Surface-layer (S-layer) proteins sap and EA1 govern the binding of the S-layer-associated protein BslO at the cell septa of Bacillus anthracis. J bacteriol. 2012;194(15):3833-40.
- Avilán L, Gualdrón-López M, Quiñones W, et al. Enolase: a key player in the metabolism and a probable virulence factor of trypanosomatid parasites—perspectives for its use as a therapeutic target. Enzyme Res. 2011;2011.
- Agarwal S, Kulshreshtha P, Bambah Mukku D, et al. α-Enolase binds to human plasminogen on the surface of Bacillus anthracis. Biochimica et Biophysica Acta (BBA) - Proteins and Proteomics 2008;1784(7):986-94.
- Virmani R, Sajid A, Singhal A, et al. The Ser/Thr protein kinase PrkC imprints phenotypic memory in Bacillus anthracis spores by phosphorylating the glycolytic enzyme enolase. J Biol Chem. 2019;294(22):8930-41.
- Mougous JD, Green RE, Williams SJ, et al. Sulfotransferases and sulfatases in mycobacteria. Chem biol. 2002;9(7):767-76.
- Hanson SR, Best MD, Wong CH. Sulfatases: structure, mechanism, biological activity, inhibition, and synthetic utility. Angewandte Chemie International Edition. 2004;43(43):5736-63.
- Beatty KE, Williams M, Carlson BL, et al. Sulfatase-activated fluorophores for rapid discrimination of mycobacterial species and strains. Proceedings of the National Academy Sci. 2013;110(32):12911-6.
- Palmer M. The family of thiol-activated, cholesterol-binding cytolysins. Toxicon. 2011;39(11):1681-1689.
- Read TD, Salzberg SL, Pop M, et al. Comparative genome sequencing for discovery of novel polymorphisms in Bacillus anthracis. Sci. 2002;296(5575):2028-33.
- Bishop BL, Lodolce JP, Kolodziej LE, et al. The role of anthrolysin O in gut epithelial barrier disruption during Bacillus anthracis infection. Biochem Biophysical Res Communications. 2010;394(2):254-9.
- Rivera J, Cordero RJ, Nakouzi AS, et al. Bacillus anthracis produces membrane-derived vesicles containing biologically active toxins. Proceedings of the National Academy Sci. 2010;107(44):19002-7.
- Cowan GJ, Atkins HS, Johnson LK, et al. Immunisation with anthrolysin O or a genetic toxoid protects against challenge with the toxin but not against Bacillus anthracis. Vaccine. 2007;25(41):7197-205.
- Nakouzi A, Rivera J, Rest RF, et al. Passive administration of monoclonal antibodies to anthrolysin O prolong survival in mice lethally infected with Bacillus anthracis. BMC microbiol. 2008;8(1):1-0.
- Bourdeau RW, Malito E, Chenal A, et al. Cellular functions and X-ray structure of anthrolysin O, a cholesterol-dependent cytolysin secreted by Bacillus anthracis. J Biol Chemistry. 2009;284(21):14645-56.
- Wessler S, Schneider G, Backert S. Bacterial serine protease HtrA as a promising new target for antimicrobial therapy?. Cell Communication and Signaling. 2017;15(1):1-5.
- Boehm M, Lind J, Backert S, et al. Campylobacter jejuni serine protease HtrA plays an important role in heat tolerance, oxygen resistance, host cell adhesion, invasion, and transmigration. European J Microbiol Immunol. 2015;5(1):68-80.
- Sela-Abramovich S, Chitlaru T, Gat O, et al. Novel and unique diagnostic biomarkers for Bacillus anthracis infection. Applied and environmental microbiol. 2009;75(19):6157-67.
- Chitlaru T, Zaide G, Ehrlich S, et al, Shafferman A. HtrA is a major virulence determinant of Bacillus anthracis. Mol microbiol. 2011;81(6):1542-59.
- Israeli MA, Elia U, Rotem S, et al. Distinct contribution of the HtrA protease and PDZ domains to its function in stress resilience and virulence of Bacillus anthracis. Frontiers in microbiol. 2019;10:255.
- Chitlaru T, Rotem S, Elia U, et al. A novel live attenuated anthrax spore vaccine based on an acapsular Bacillus anthracis Sterne strain with mutations in the htrA, lef and cya genes. Vaccine. 2017;35(44):6030-40.
- Arthur M, Quintiliani Jr R. Regulation of VanA-and VanB-type glycopeptide resistance in enterococci. Antimicrobial agents and chemotherapy. 2001;45(2):375-81.
- McKessar SJ, Berry AM, Bell JM, et al. Genetic characterization of vanG, a novel vancomycin resistance locus of Enterococcus faecalis. Antimicrobial agents and chemotherapy. 2000;44(11):3224-8.
- da Silva AR, Ferro JA, Reinach FC, et al. Comparison of the genomes of two Xanthomonas pathogens with differing host specificities. Nature. 2002;417(6887):459-63.
- Wright GD, Walsh CT. D-Alanyl-D-alanine ligases and the molecular mechanism of vancomycin resistance. Accounts of chemical research. 1992;25(10):468-73.
- Hoyland CN, Aldridge C, Cleverley RM, et al. Structure of the LdcB LD-carboxypeptidase reveals the molecular basis of peptidoglycan recognition. Structure. 2014;22(7):949-60.
- Gusarov I, Nudler E. NO-mediated cytoprotection: instant adaptation to oxidative stress in bacteria. Proceedings of the National Academy of Sci. 2005;102(39):13855-60.
- Shatalin K, Gusarov I, Avetissova E, et al. Bacillus anthracis-derived nitric oxide is essential for pathogen virulence and survival in macrophages. Proceedings of the National Academy of Sci. 2008;105(3):1009-13.
- Van Sorge NM, Beasley FC, Gusarov I, et al. Methicillin-resistant Staphylococcus aureus bacterial nitric-oxide synthase affects antibiotic sensitivity and skin abscess development. J Biol Chem. 2013;288(9):6417-26.
- Holden JK, Li H, Jing Q, et al. Structural and biological studies on bacterial nitric oxide synthase inhibitors. Proceedings of the National Academy Sci. 2013;110(45):18127-31.
- Holden JK, Li H, Jing Q, Kang S, et al. Structural and biological studies on bacterial nitric oxide synthase inhibitors. Proceedings of the National Academy Sci. 2013;110(45):18127-31.
- Clements MO, Watson SP, Foster SJ. Characterization of the major superoxide dismutase of Staphylococcus aureus and its role in starvation survival, stress resistance, and pathogenicity. J bacteriol. 1999;181(13):3898-903.
- Lynch M, Kuramitsu H. Expression and role of superoxide dismutases (SOD) in pathogenic bacteria. Microbes and infection. 2000;2(10):1245-55.
- Cybulski Jr RJ, Sanz P, Alem F, et al. Four superoxide dismutases contribute to Bacillus anthracis virulence and provide spores with redundant protection from oxidative stress. Infection and immunity. 2009;77(1):274-85.
- Hider RC, Kong X. Chemistry and biology of siderophores. Nat product rep. 2010;27(5):637-57.
- Wilson MK, Abergel RJ, Arceneaux JE, et al. Temporal production of the two Bacillus anthracis siderophores, petrobactin and bacillibactin. Biometals. 2010;23(1):129-34.
- Anantharaman V, Aravind L. Evolutionary history, structural features and biochemical diversity of the NlpC/P60 superfamily of enzymes. Genome biol. 2003;4(2):1-2.
- Xu Q, Mengin-Lecreulx D, Liu XW, et al. Insights into substrate specificity of NlpC/P60 cell wall hydrolases containing bacterial SH3 domains. MBio. 2015;6(5):e02327-14.
- Kim SK, Park YM, Jung KH, et al. Deletion of a putative NlpC/P60 endopeptidase BAS1812 affects germination, long-term survival and endospore formation in Bacillus anthracis. Microbiol. 2017;163(2):144-52.
- Okugawa S, Moayeri M, Pomerantsev AP, et al. Lipoprotein biosynthesis by prolipoprotein diacylglyceryl transferase is required for efficient spore germination and full virulence of Bacillus anthracis. Mol microbiol. 2012;83(1):96-109.
- Trautmann A. Extracellular ATP in the immune system: more than just a “danger signal”. Sci signal. 2009;2(56):e6.
- Gorini S, Gatta L, Pontecorvo L, et al. Regulation of innate immunity by extracellular nucleotides. Am j Blood Res. 2013;3(1):14.
- Haskó G, Cronstein BN. Adenosine: an endogenous regulator of innate immunity. Trends immunol. 2004;25(1):33-9.
- Thammavongsa V, Kern JW, Missiakas DM, et al. Staphylococcus aureus synthesizes adenosine to escape host immune responses. J Exp Med. 2009;206(11):2417-27.
- Ogunniyi AD, Folland RL, Briles DE, et al. Immunization of mice with combinations of pneumococcal virulence proteins elicits enhanced protection against challenge with Streptococcus pneumoniae. Infection and immunity. 2000;68(5):3028-33.
-
Yacoby I, Shamis M, Bar H, et al. Targeting antibacterial agents by using drug-carrying filamentous bacteriophages. Antimicrobial agents and chemotherapy. 2006;50(6):2087-97.
- Chitlaru T, Israeli MA, Bar-Haim E, et al. Next-Generation Bacillus anthracis Live Attenuated Spore Vaccine Based on the htrA-(High Temperature Requirement A) Sterne Strain. Sci rep. 2016;6(1):1-5.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref