Research Article - Otolaryngology Online Journal (2018) Volume 8, Issue 1
Experiences of Endocanalicular Laser Dacryocystorinostomy with Multi - Diode Laser
Seyfettin Erdem1*, Ayhan Kaydu2, Selahattin Balsak3, Umut Dağ3, Mehmet Emin Dursun3, Birgül Dursun3 and Sevin Söker Çakmak41Department of Ophthalmology, Diyarbakır Bismil State Hospital, Turkey
2Department of Anaesthesiology, Diyarbakır State Hospital, Turkey
3Department of Ophthalmology, Diyarbakır Training and Education Hospital, Turkey
4Department of Ophthalmology, World Eye Hospital, Turkey
- Corresponding Author:
- Seyfettin Erdem (MD)
Department of Ophthalmology
Diyarbakır Bismil State Hospital
Bismil, Turkey
Mobile: +904124152310
Email: serdem2147@hotmail.com
Received Date: January 29, 2018; Accepted Date: February 03, 2018; Published Date: February 09, 2018
Abstract
Purpose: Chronic dacryocystitis is a common disease in the population and usually affects middle-aged women. We aimed to evaluate the efficacy and clinical outcomes of dacryocystorhinostomy (DCR) operations by endoanalytic multi-diode laser.
Methods: Twenty-nine eyes of 28 patients diagnosed with chronic dacryocystitis with nasolacrimal duct obstruction were included retrospectively in this study. Silicone tube implantation was performed in all cases by endocanalcular laser dacryocystorhinostomy (EDCR) with multi-diode laser with the help of 30 ° nasal video endoscope. Demographic data, follow-up time, anesthesia method and success rates were recorded. The success was assessed as epiphora passage and absence of major laser-induced intranasal injury.
Results: Seven of the cases were male (24.14%) and 22 were female (75.86%). The mean age was 32.9 ± 20.77 years (8-82). The mean follow-up was 3 to 24 months (mean 15.67 ± 5.40 months). Endocanalicular laser DCR was successfully applied in 29 patients. 20 patients (68.9%) did not have epiphora complaints. The cause of failure in 9 patients was mucosal construction on the edge of the osteotomy. One of the unsuccessful case was dacryocystitis secondary to trauma and the other had primer nasolacrimal duct obstruction. External DSR was performed on 9 of the unsuccessful cases. In one case; the area of nasal osteotomy was covered with fibrotic tissue. The nasolacrimal duct was opened by exposing the fibrotic tissue using endonasal endoscopy. Eight of the cases were pediatric. In seven of them, the endocanalicular laser DCR did not develop any occlusion.
Discussion: Although the long-term success rate is not as high as external DCR, Endocanalicular laser DCR is an alternative surgical method that can be performed with low complication rates, which can be well tolerated by patients in treatment of chronic dacryocystitis.
Keywords
Endocanalicular laser; Dacryocystorinostomy; Multi-diode laser; Dacryocyctitis; Epiphora
Introduction
Chronic dacryocystitis is a common disease in the population and usually affects middle-aged women. The most common cause is occlusion of the nasolacrimal duct [1]. Chronic dacryocystitis trigger epiphora and occasional acute dacryocystitis episodes. At the same time, agents that affect chronic dacryocystitis make the eye vulnerable to external infections.
The treatment of chronic dacryocystitis is surgery. The purpose of the surgery is to create a permanent passage between the sac and the nasal mucosa [2]. External dacryocystorhinostomy (DCR) described by Toti in 1904 is the classical treatment method used for obstruction of the lacrimal system [[3]]. Nowadays, surgical method developed by Dupey-Dutemps and Bourguet is used[4]. The internal-approach DCR was described by Caldwell [5] in 1893, but has not been popular until the use of endoscopes in sinus surgery. The rigid nasal endoscope allows better visualization of the nasal cavity, while at the same time allowing safe manipulation [6],[7] Massero described the laserassisted endonasal DSR for the first time by using an argon laser to remove the bone block. In 1987, extensive research results on endoscopy by Wigand and Messerklinger were published and became popular in the following years [8]. Due to endocanalicular laser DCR is a mininal invasive surgery, there are some advantages such as short recovery time, lower risk of morbidity, orbicularis oculi pump mechanism and cosmesis [9].
In this study, we performed multi-diode laser endocanalicular dacryocystorhinostomy and bicanalicular silicone tube implantation by using nasolacrimal video endoscopy to patients with nasolacrimal duct obstruction which admitted to our clinic with a diagnosis of chronic dacryocystitis and epiphora. Patients undergoing endocanalicular laser dacryocystorhinostomy with multi-diode laser were retrospectively studied. It was aimed to evaluate the reliability, advantages and disadvantages of the method in terms of surgical success and complications.
Materials and Methods
Approval for the study was granted by the Institutional Ethical Committee. The researches obtained written informed consent from all patients. 29 eyes of 28 patients with epiphora who were diagnosed as chronic dacryocystitis with nasolacrimal duct obstruction were included in the study retrospectively. Patients’ data was retrieved from the file system. Demographic data, follow-up time, anesthesia method and success rates were recorded. The absence of epiphora and laser-induced intranasal major injury was considered a success.
Evaluation of patients
The complaints of the patients, the time of onset, history of medical and surgical treatments, comorbidities and the drugs were recorded. In all patients, visual acuity, bio microscopic examination, intraocular pressure measurement, eye examinations were recorded. Preoperatively all patients were treated by consultant ophthalmologist and otolaryngologist; palpation of the lacrimal duct, probing and irrigation of the lacrimal sac and duct, dye loss test and nasal endoscopy were performed. The eyelids were examined, the status of the punctures was evaluated, lavage with nasolacrimal cannula was performed and lavage ending was evaluated (soft, hard). Endocanalicular laser dacryocystorhinostomy with multi diode was planned to patients with not any nodal pathology (polyp, tumor, severe septal deviation, hypertrophic median concha), hard ending with lavage, with nasolacrimal duct obstruction without punctum, canalicule and common canalicular obstruction. Nasal endoscopic examination was performed by the otolaryngologist in all cases preoperatively. Hemogram, biochemistry and bleeding and coagulation time tests were measured. The headlamp was used to view the surgical field.
The device used in surgery (Multidiode S30 OFT from INTERMEDIC, Spain) had a laser probe flex with Semiconductors 400- 600 μ fiber. This laser probe had Wavelength 980 nm, Power 1-30 watts. The optical laser apparatus has a fiberoptic probe with dimensions of 36 × 46 × 21 cm, a weight of 12 kg, 600 μ silica-fluoropolymer-tefzel and 600 μ silica-silicapolyamide.
Surgical procedure
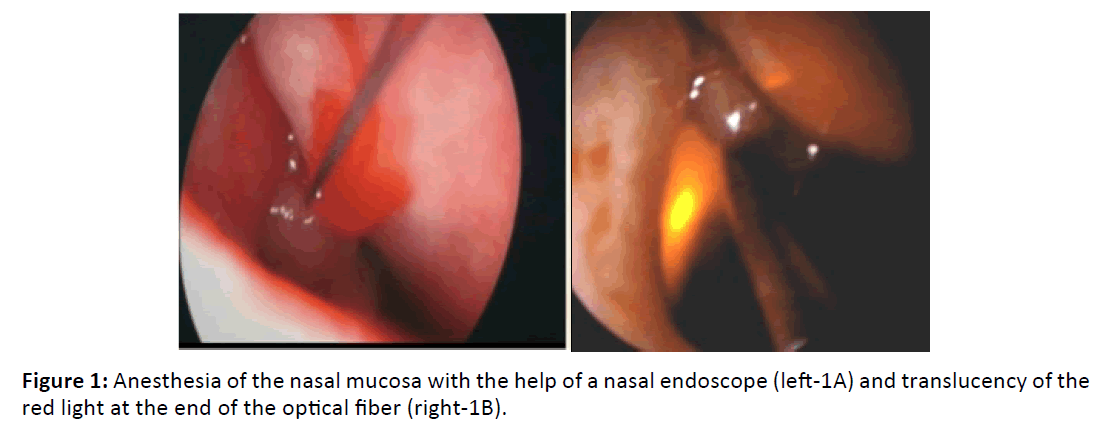
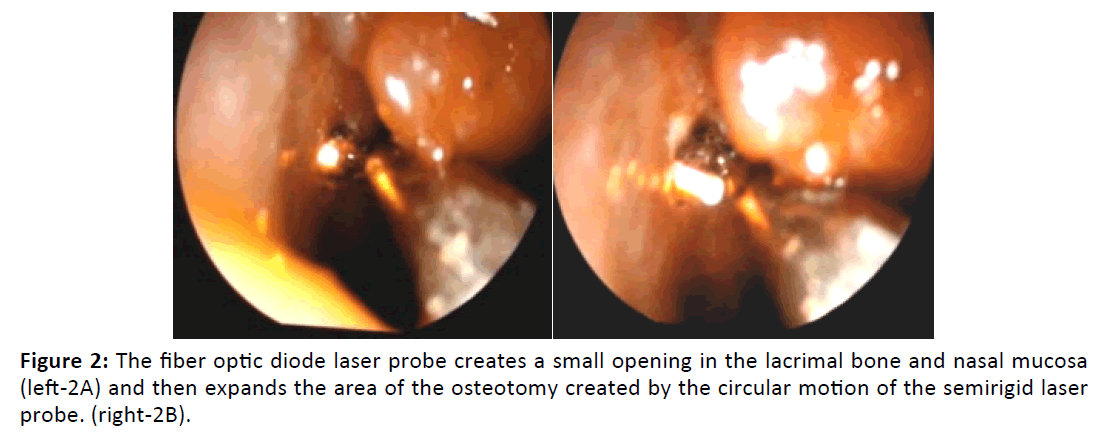
The operation was performed under local anesthesia in adult patients and under general anesthesia in children. Periorbital area was sterilized with povidone iodine, as local anesthetic agent 3 ml mixture of 2% mepivacaine and 0.75% bupivacaine was applied to the infratrochlear nerve and to the nasociliary nerve which is the branch of the infraorbital nerve. 4% lidocaine and 1/100.000 epinephrine impregnated with cotton sponges were applied to the nasal cavity for topical anesthesia and benefit effects of vasoconstriction 15 minutes before the operation. The punctures were dilated with a punctum dilator and medialized with a periosteal elevator. The multidiode laser is set to average 10 watts, continuous energy and contact mode. Cotton in the nasal cavity was removed. A 600 μm flexible fiber optic multidiode laser probe was passed through the lower canal to the lacrimal bone. The nasal passages were visualized with the help of a 30 ° nasal video endoscope, and the red beam translucency of this optical fiber was seen Figures 1A and 1B. The middle chunk was mediated. After a small opening in the lacrimal bone and nasal mucosa with the help of the laser probe, the osteotomy area was enlarged by 8 to 10 mm with the circular movement of the semi rigid laser probe Figures 2A and 2B. The coagulation and necrotic tissue were removed with the help of an aspirator. In all cases except one case, the silicone tube was sent to the nasal cavity under the nasal endoscope guidance from the upper and lower cannulas. Biconical silicone tube intubation was performed by attaching the free ends of the silicone tube in the nasal cavity. In one case, silicone tube intubation was performed by sending a Mono - K silicone tube through the lower canal and the operation was terminated.
After the operation, cold compress was applied for 15 minutes/hour for one day. The patients were discharged one day after the operation after surgery; patients were given tobramycin/dexamethasone drops and 0.025% flunisolide nasal spray 4 × 1. Treatment was stopped gradually by reducing until 12 weeks. The patients were seen at postoperative 1st day, 1st week, 1st month, 3rd month, 6th month and 12th month controls. Nasolacrimal irrigation was performed and the area of nasal osteotomy was cleaned endoscopically.
Statistical analysis
Data analysis was performed using SPSS 15 (Statistical Package for the Social Sciences, Chicago, Illinois, USA). Data of both groups were given as mean and (±) standard deviation, whereas categorical variables as frequencies and percentages. A p level of <0.05 was taken as statistically significant.
Results
Twenty-nine eyes of 28 patients diagnosed with chronic dacryocystitis were included in our study. Twenty-two of the eyes were female (75.86%) and 7 were male (24.14%). The mean ages were 32.9 ± 20.77 years (8-82). The follow-up period was 3- 24 months (mean 15.67 ± 5.40 months). The general anesthesia were performed in ten surgeries (34.48%), and 19 of patients with local anesthesia (65.52%). 14 cases of the cases were intervened in left eyes (48.28%) and 15 cases were in the right eyes (51.72%). Seven of operated patients (24.13%) had a previous surgical intervention history Table 1. There were no epiphora complaints in 20 patients these cases were accepted as successful cases and the success rate was 68.9%. In 9 unsuccessful cases, mucosal constriction, fibrosis, and synechiae in the middle concha were noted at the edge of the osteotomy. One of the cases of failure was dacryocystitis secondary to trauma, external DCR was applied to these patients. In other cases, primer nasolacrimal duct obstruction was present. In one case, there was adhesion between the middle concha and the osteotomy area. Adhesions were resolved by the otolaryngologist, removing the top of the middle concha. In 3 unsuccessful cases, the lavage test was open until 7 months after the operation, but then closed off. Although the otolaryngologist had endoscopically cleaned the granulation tissue and scar tissue, external lavage DCR was performed when the lavage test was closed. External DCR was also applied to the remaining 5 failed cases. Because of the closed lavage, all patients who underwent external DCR were successful. The overall success rate with the external DCR was 100% On the other hand, two failed unsuccessful external DCR were operated successfully with endocanalcular laser DCR.
| Characteristics | |
| Age (Years) | 32,9± 20,77 (8- 82) |
| Gender | |
| •Female | 22 |
| • Male | 7 |
| Anesthesia type | |
| •General | 10 |
| • Local | 19 |
| Eyes | |
| • Right | 15 |
| • Left | 14 |
| Mean follow-up time (months) | 15.67 ± 5.40 (3-24) |
Table 1: Demographic data of the patients.
The eight of our cases were between 8 and 16 years of age. Of these, 5 cases had been applied with unsuccessful silicone tube intubation previously. In pediatric cases, successful results were obtained after endocanalicular laser DCR except one patient. This failed pediatric case had traumatic dacryocystitis and this case was successfully operated with external DCR. Two patients had a silicone tube spontaneously prolapsed 2 months after surgery. In a case with upper punctum agenesis, Mono-K silicone tube intubation was performed from the lower canal. Surgery was performed bilaterally in the same session in one patient. Silicone tube was removed in two patients because of punctum erosion at 4 months after surgery. In other cases silicone tube was removed at the end of 6th month by nasally withdrawing the upper tip without the need for anesthesia. As a complication, there was a punctum prolapse of the bicanalicular silicone tube in a postsurgical case (3.44%). The silicone tube was revised with topical anesthesia with the help of a nasal endoscope. In two cases (6.89%), the bicanalicular silicone tube was observed to be prolapsed from punctum. In these cases, when these knots were observed in the pouch, silicone tubes were removed and a new silicone tube was implanted
Discussion
In our study, we found the success rate of operation of patients who underwent multi-diode endocanalicular laser dacryocystorhinostomy operation as 68.9%. In other cases, the success was achieved with external dacryocystorhinostomy in cases with closed lavage.
Dacryocystorhinostomy is a method of treating chronic dacryocystitis resulting from nasolacrimal duct obstruction. Currently, external DCR is mostly used in the treatment of chronic dacryocystitis. The success rate in the external surgical approach is reported as 79-99% [10-12]. Despite these success rates, this method has disadvantages such as skin incision scarring, severe intraoperative bleeding, disruption of the medial canthus anatomy, long surgical time and high morbidity [13].
Endocanalicular laser DCR was first applied by Levin in 1992 on cadavers [14]. Christenbury applied this method for the first time [15]. Diode laser has flexible fiberoptic proper for normal anatomical pathway and postoperative edema is not observed. Endocanalicularly, fiber is applied to lacrimal sac, then a bone window is created by a laser and a fistula is formed between the nasal cavity and the lacrimal sac. Endoanalicular laser, which only requires nasal endoscope, is safe due to DCR ray reaching directly from the sac to the nasal cavity and protects from orbital perforation
In multi-diode laser technique, the principle is to absorb the energy of the target tissue and then transform it into heat energy to form a fistula between the lacrimal sac and the nasal cavity by creating an incision in the bone and mucosa [16]. Fiberoptic laser is used in contact mode for lacrimal sac vaporization, for the initial stage of endocanalicular rhinostomy, and to expand the endonasal pathway. With the use of a diode laser, tissue damage in the area of osteotomy and debris remain in large quantities. Therefore, clearing the area of osteotomy frequently postoperatively increases the success rate. Postoperatively, washing and cleaning osteotomy site accelerates wound healing by reducing inflammatory response [17]. Mitomycin C, an antimetabolite, prevents scar development and prevents occlusion and constriction at the osteotomy margin [18-21]. Mitomycin C was also used in the DCR to keep the osteotomy open until [18-21] weeks. In our study, we performed postoperative nasolacrimal duct irrigation and osteotomy site cleaning with nasal endoscope
Goel R performed transcanalicular laser assisted dacryocystorhinostomy to patients of nasolacrimal duct obstruction with 12 month follow-up and achieved 90% success [22]. Henson found mucosa construction at the edge of the osteotomy in 5 unsuccessful cases at the end of the 6th month and 12th month follow-up17. In one of our unsuccessful cases, we identified adhesions and constructions in the osteotomy area of the mid-concha.
Two of our cases were previously treated with external DCR and the operations were unsuccessful. We performed multi-diode endocanalic laser DCR in these cases and in these two cases we succeeded [23]. In cases with 15 failed external DCR, they performed transcranial laser DCR with semiconducting diode laser. In 12 of these cases (80%) they achieved success. They argued that the transcranial laser DCR would be a successful method with minimal invasion in the failed external DCR [23]. Diode laser can provide effective tissue dissection with minimal damage and is a good alternative technique for patients with failed EDCR with membranous obstruction [24].
The success rates of transcranial laser DCR were 60- 85% in different studies [25-27]. In our study, our multidiode laser DCR success rate was 68.9%. One of the unsuccessful cases had adhesion and the other was a trauma story, in which case the concha bullosa was detected. We performed external DCR to these cases. In another unsuccessful case, we saw fibrotic tissue developed in the area of osteotomy. Nasolacrimal duct obstruction was opened endoscopically by excision of fibrotic tissue.
In our study, 8 pediatric cases successfully were underwent dacryocystorhinostomy with multidiode laser. Of these, 5 cases had been done unsuccessful silicone tube intubation previously. In pediatric cases, successful results were obtained after endocanalicular laser DCR except one. Doyle et al. reported that patients with congenital nasolacrimal duct obstruction were treated with KTP laser and in 6 patients, the recurrence were reported [28]. Çakmak showed the 8 endocanalicular laser DCR cases successfully performed at pediatric ages and in 7 of them, the complaints of epiphora disappeared [29]. Holmium YAG laser was performed in 5 children with dacryocystitis by Choudhary [30].
Conclusion
The gold standard in the treatment of chronic dacryocystitis is external DCR. However, as an alternative procedure, such as in cataract surgery, microinvasion surgery has begun to be preferred in the treatment of chronic dacryocystitis. Multidiode endocanalicular laser DSR, which has become popular with endoscopic surgery, although the long-term success rate is not as high as external DCR, is an alternative surgical method that can be applied in the treatment of chronic dacryocystitis with advantages such as short recovery time, lower risk of morbidity, orbicularis oculi pump mechanism and cosmesis. Despite the fact that endocanalicular laser DCR is an effective technique with a low complication rate which can be well tolerated by patients, the necessity of expensive surgical instruments such as endoscopes and lasers is a limiting factor for surgical application. Postoperative irrigation and clearing of osteotomy area and intraoperative application of mitomycin c are factors that increase the success rate. However, comparative studies are needed to evaluate the success of this surgical procedure.
References
- Önerci M (2002) Dacryocystorhinostomy diagnosis and treatment of nasolacrimal canal obstructions. Rhinology 40: 49-65.
- Özkayaa, Gürcan Z ÖS (2007) Long-term comparison of primer external dacryocystorhinostomy operations with and without silicone tube intubation. Turkey Klin J Ophthalmol 16: 77-81.
- Toti A (1904) New conservative method of radical cure of chronic suppurations of the lacrimal sac (dacriochistoricostomy) e. Clin Mod 10: 385-387.
- Dupuy-Dutemps L (1921) Plastic process of dacryocystorhinostomy and its results. Ann Ocul 158: 241-261.
- Caldwell GW (1893) Title two new operations for obstruction of the nasal duct with preservation of the canaliculi and an incidental description of a new lachrymal probe. NY Med J 57: 581.
- Anadolu Y, Akturk T (1998) Adjunctive use of mitomycin C on endoscopic lacrimal surgery. Br J Ophthalmol 82: 63-66.
- Massero BM, Gonnering RS, Harris GJ (1990) Endonasal laser dacryocystorhinostomy. Arch Ophthalmol 108: 1172-1176.
- Kapadia MK, Freitag SK, Woog JJ (2006) Evaluation and management of congenital nasolacrimal duct obstruction. Otolaryngol Clin North Am 39: 959-977.
- Athanasiov PA, Prabhakaran VC, Mannor G, Woog JJ (2009) Transcanalicular approach to adult lacrimal duct obstruction: a review of instruments and methods. Ophthalmic Surg Lasers Imaging 40: 149-59.
- Nowinski TS, Flanagon JC (1985) Pediatric dacryocystorhinostomy. Arch Ophthalmol 1985: 1226-1228.
- Warren JF, Seiff SR KM (2005) Long-term results of external dacryocystorhinostomy. Ophthalmic Surg Lasers Imaging. Ophthalmic Surg Lasers Imaging 36: 446-450.
- Tarbet KJ, Custer PL (1995) External dacryocystorhinostomy: Surgical success, patient satisfaction, and economic cost. Ophthalmology 102: 1065-1070.
- Piaton JM, Keller P, Limon S QS (2002) First line endonasal dacryocystorhinostomy technique and results. Comparison between diode laser and electrocautery instrument. Study based on 422 procedures. J Fr Ophtalmol 25: 135-145.
- Levin PS, Stormogipson DJ (1992) Endocanalicular Laser-Assisted Dacryocystorhinostomy: An Anatomic Study. Arch Ophthalmol 110: 1488-1490.
- JD C ( 1992) Translacrimal laser dacryocystorhinostomy. Arch Ophthalmol 110: 110.
- Yilmaz BM, Yilmaz T, Taskin U (2015) Prospective comparison of 3 dacryocystorhinostomy surgeries: External versus endoscopic versus transcanalicular multidiode laser. Ophthal Plast Reconstr Surg 31: 13-18.
- Fernandez MA, Fernandez FJ, Fernandez MA, Lara MC, Domínguez R et al. ( 2004) Endonasal and endocanalicular dacryocystorhinostomy by diode laser. Preliminary results. Acta Otorrinolaringol Esp 55: 171-176.
- Henson RD, Henson RG, Cruz HL, Camara JG (2007) Use of the diode laser with intraoperative mitomycin C in endocanalicular laser dacryocystorhinostomy. Ophthal Plast Reconstr Surg 23: 134-137.
- Camara JG, Bengzon AU, Henson RD (2000) The safety and efficacy of mitomycin C in endonasal endoscopic laser-assisted dacryocystorhinostomy. Ophthal Plast Reconstr Surg 16: 114-118.
- Selig YK, Biesman BS, Rebeiz (2000) EE Topical application of mitomycin-C in endoscopic dacryocystorhinostomy. Am J Rhinol 14: 205-207.
- You YA, Fang CT (2001) Intraoperative mitomycin C in dacryocystorhinostomy. Ophthal Plast Reconstr Surg 17: 115-119.
- Goel R, Nagpal S, Kumar S, Meher R, Kamal S, et al. (2016) Transcanalicular laser-assisted dacryocystorhinostomy with endonasal augmentation in primary nasolacrimal duct obstruction: our experience. Ophthal Plast Reconstr Surg 33: 408-412.
- Narioka J, Ohashi Y (2008) Transcanalicular-endonasal semiconductor diode laser-assisted revision surgery for failed external dacryocystorhinostomy. Am J Ophthalmol 146: 60-68.
- Lee J, Choi SY, Lee H, Chang M, Park M et al. (2015) The clinical effectiveness of transcanalicular diode laser-assisted revision surgery for failed endoscopic endonasal dacryocystorhinostomy. Br J Ophthalmol 99: 1130-1133.
- Basmak H, Cakli H, Sahin A (2011) Comparison of endocanalicular laser dacryocystorhinostomy with and without endonasal procedures. Graefe’s Arch Clin Exp Ophthalmol 249: 737-743.
- Kaynak P, Ozturker C, Yazgan S (2014) Transcanalicular diode laser assisted dacryocystorhinostomy in primary acquired nasolacrimal duct obstruction: 2-year follow up. Ophthal Plast Reconstr Surg 30: 28-33.
- Uysal IÖ, Özçimen M, Yener HI, Kal A (2011) Pediatric endocanalicular diode laser dacryocystorhinostomy: Results of a minimally invasive surgical technique. Eur Arch Oto-Rhino-Laryngology 268: 1283-1288.
- Doyle A, Russell J, O’Keefe M (2000) Paediatric laser DCR. Acta Ophthalmol Scand 78: 204-205.
- Cakmak SS, Yildirim M (2010) Use of endocanalicular dacryocystorhinostomy with multidiode laser in children. Int J Pediatr Otorhinolaryngol 74: 1320-1322.
- Choudhary A, Deans JAJ, Moriarty BJ (2006) Modified laser DCR for paediatric nasolacrimal duct obstruction. Eye 20: 347-350.