Research Article - Journal of Clinical Pathology and Laboratory Medicine (2023) Volume 5, Issue 2
Evaluation of different metastasis sites in large intestine adenocarcinoma based on a case
Alptekin Sen*Department of Pathology, Istanbul Demiroglu Bilim University Faculty of Medicine, Istanbul, Turkey.
- *Corresponding Author:
- Alptekin Sen
Department of Pathology
Istanbul Demiroglu Bilim University Faculty of Medicine
Istanbul, Turkey.
E-mail: alptekinsen2000@gmail.com
Received: 29-Mar-2023, Manuscript No. AACPLM-23-95046; Editor assigned: 01-Apr-2023, PreQC No. AACPLM-23-95046(PQ); Reviewed: 15-Apr-2023, QC No. AACPLM-23-95046; Revised: 20-Apr-2023, Manuscript No. AACPLM-23-95046(R); Published: 27-Apr-2023, DOI:10.35841/aacplm-5.2.141
Citation: Sen A. Evaluation of different metastasis sites in large intestine adenocarcinoma based on a case. J Clin Path Lab Med. 2023;5(2):141
Abstract
Adenocarcinomas of the colon and rectum account for about 95% of all cholerectal carcinomas. In the Surveillance Epidemiology and End Results (SEER) Program of the National Cancer Institute, it has been reported that 4.1 percent of people may develop colorectal cancer during their lifetime. Metastatic colon adenocarcinoma is an advanced stage malignancy, and this metastasis occurs especially and in the first place, usually to the liver and lungs. However, the peritoneum, brain and distant lymph nodes are also places where adenocarcinoma often metastasizes. In addition, there may also be metastases to unexpected areas. Jaw, bladder, soft tissue, intramuscular and cutaneous metastases have been described. Metastases to the floor of the mouth, maxillary gum and palate can also be observed rarely. As in our case, buccal metastasis is limited to only a few cases in the literature.
Keywords
Adenocarcinoma, Colon, Metastasis, Buccal region.
Introduction
Colon adenocarcinoma both in the USA and in our country is known as the 3rd most common cancer observed in both men and women and the 3rd cancer that causes the most deaths. Metastasis it is the most important cause of death for cholerectal carcinomas. Studies shows that 22% of cholecliptal carcinomas are metastatic when diagnosed and metastases may develop in approximately 70% of patients [1-3]. Although it is a fact that distant metastases reduce survival, the relationship between distant metastasis sites and survival is complex [4-8]. In our case, it is important for colorectal cancers because it has a metastasis area that is not very often defined.
Methods
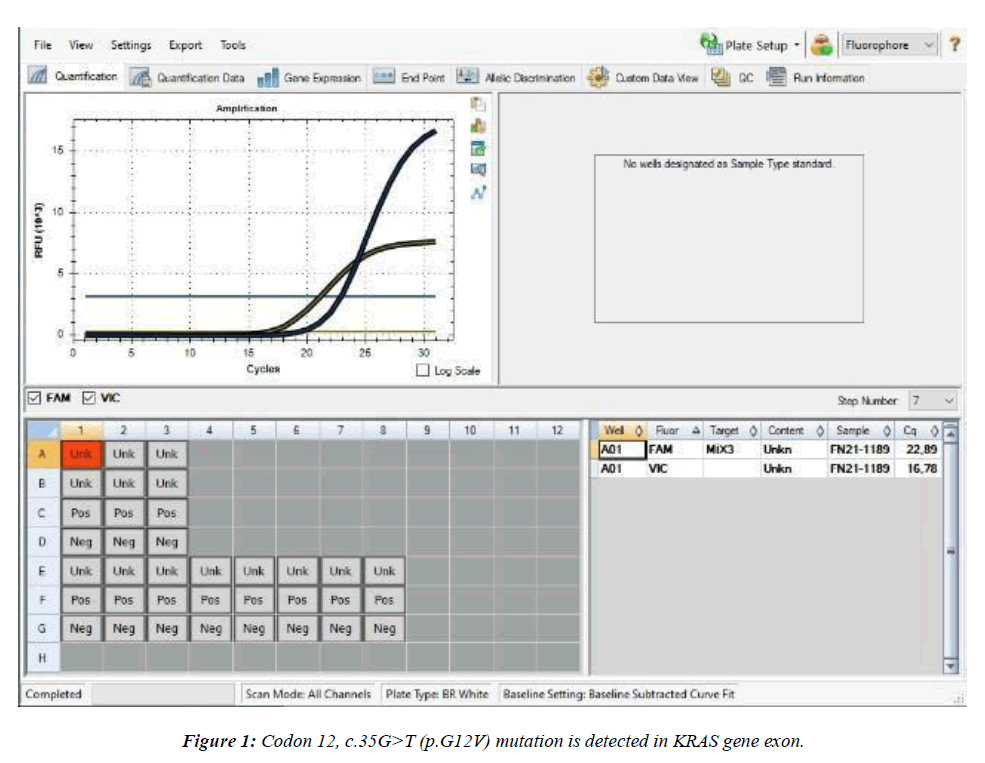
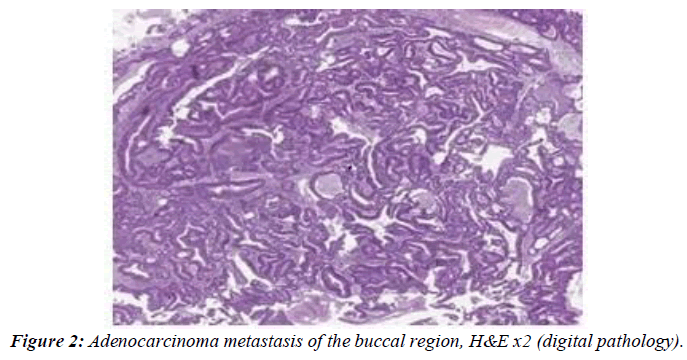
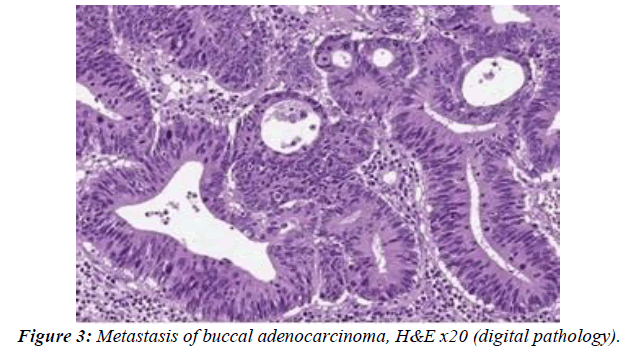
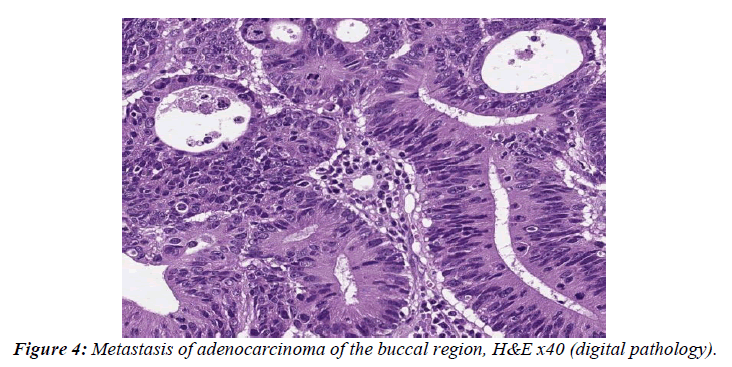
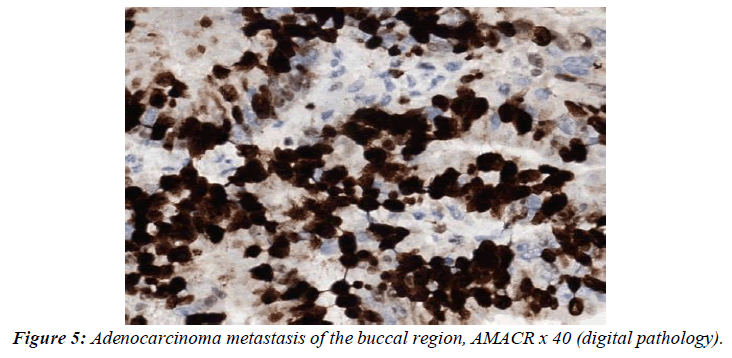
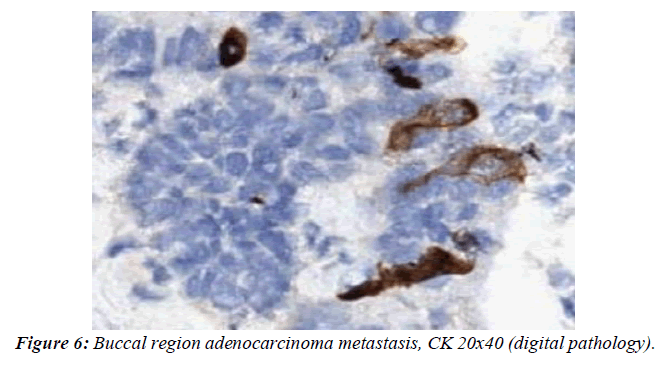
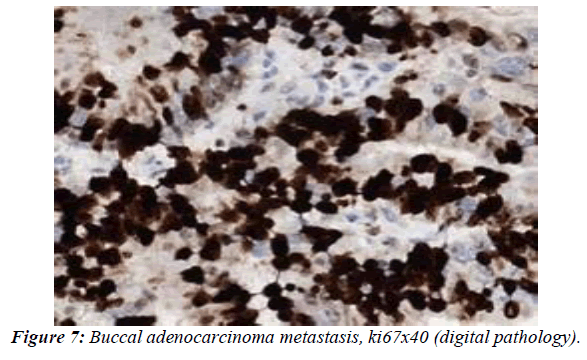
Our patient was a 47-year-old man, in the colonoscopy performed by the gastroenterology specialist who applied due to complaints of the gastrointestinal system a 5- 6 cm diameter mass blocking the lumen is detected in the proximal rectum and biopsy is taken [9-12]. This biopsy example is evaluated by a special pathology laboratory and diagnosed as 'moderately differentiated adenocarcinoma'. Phenomenon as a result of the PET/CT performed in our hospital following the diagnosis, it is stated that a mass in the proximal rectum, left paratracheal lymph node metastasis, metastatic nodule in the lower lobe of the left lung were observed. Following this, the patient is able to 4 cycles of chemotherapy followed by preoperative intensity modulated radiotherapy. Then the patient underwent intraoperative procedure (frozen) from paratracheal lymph nodes and left lobectomy for the lesion in the lung. Examination of both paratracheal lymph nodes and lobectomy material provides the pathological diagnosis of colonic type adenoraccinoma metastasis. In the study conducted in the DNA obtained from the tumoral tissue in the pathology preparations Codon 12, c.35G>T (p.G12V) mutation is detected in KRAS gene exon 2 Figure 1. In our case during the period when he is hospitalized for treatment in our hospital, he complains of gum infection [13-16]. Although antibiotic therapy is applied for this, the treatment remains unresponsive and a growing mass is detected in the buccal region. On top of that the existing mass was excised and sent to our laboratory for examination, the material reaches our Pathology Laboratory it consisted of 2 pieces of bleeding, irregular-surfaced, fragile mucosal tissue of 4x2x1.5 and 2.5x2x1 cm in size, taken from both areas of the buccal region(right-left). Fragments were taken from both tissue fragments for microscopic evaluation. After the follow-up of tissue fragments, in microscopic H&E painted sections prepared by cutting, it is observed that both pieces of tissue are completely infiltrated by tumoral cells. These cells consist of atypical epithelial cells with large-hyperchromatic nuclei organized to form irregular gland structures and cords Figures 2-4. We also performed an immunohistochemical study of our case, taking into account the previous diagnosis. (CK20, AMACR and ki67) Figures 5-7, that 67 proliferation index, the histopathology of our patient was quite high (75- 80%), consistent with high mitosis. At the end of all these histopathological and immunohistochemical findings, we diagnosed our case as Adenocarcinoma metastasis.
Conclusion and Discussion
Colorectal cancers are life-threatening cancers, especially when their diagnosis is made late. Approximately 1/5 of all cholectal cancers have metastases when they are first diagnosed, and in 3/4 of them, it is stated that metastasis may develop over the years even if there is no metastasis when diagnosed. In this study involved multiple cases. It has been found that cholectal cancers metastasize mainly to intrathoracic organs, in the second place to the nervous system, and in the third to intraperitoneal organs (especially when they are stony ring cell and mucinous). In another study it is pointed out that cholectal cancers constitute distant organ metastases long before they are diagnosed with current screening tests. In the study conducted the genetic profiles of the primary tumor and its metastatic tumors were compared and the presence of metastases in very short periods following diagnosis was shown at a rate as high as 80%. Except for the usual metastasis areas of colorectal carcinomas skin, muscle and bone metastases have been described as unusual metastasis areas. In the presence of metastases in this unusual area it is claimed that brain involvement occurs more frequently without lung or liver involvement and the prognosis is worse. In colorectal carcinomas metastases of the oral region; are very rare metastases that can be observed in oral soft tissue and jaw bones. In addition oral metastases are also rarely observed compared to primary tumors (Less than 1%). Moreover, most of them happen to the jawbone. Oral mucosal metastatic tumors are extremely rare. Previously in the oral region Maxillary gingiva and palate metastases of colorectal carcinoma have also been described and expressed as end-stage findings. As in our case, buccal cavity metastasis is extremely rare, and only a few cases are available in the literature. Our case after being diagnosed with colon adenocarcinoma in 2019, he is a patient who shows lung, paratracheal lymph node metastasis in the process of 2021-2022 despite treatment and then followed up with buccal region metastases. As such is presented both because of the settlement and because of the possibility that the presence of this unusual settlement may enrol the prognosis, as in previous published articles on this subject.
Compliance with ethical standards
Appropriate.
Funding
No.
Conflict of interest
No.
Contributions
There are no contributors other than me.
References
- Van Cutsem E, Oliveira J. Advanced colorectal cancer: ESMO clinical recommendations for diagnosis, treatment and follow-up. Ann Oncol. 2009;20:61-3.
- Ansa BE, Coughlin SS, Alema-Mensah E, et al. Evaluation of colorectal cancer incidence trends in the United States (2000–2014). J Clin Med. 2018;7(2):22.
- Littlejohns P, Tamber S, Ranson P, et al. Treatment for liver metastases from colorectal cancer. Lancet Oncol. 2005;6(2):73.
- Elias D, Liberale G, Vernerey D, et al. Hepatic and extrahepatic colorectal metastases: when resectable, their localization does not matter, but their total number has a prognostic effect. Ann Surg Oncol. 2005;12:900-9.
- Pulitano C, Bodingbauer M, Aldrighetti L, et al. Liver resection for colorectal metastases in presence of extrahepatic disease: Results from an international multi-institutional analysis. Ann Surg Oncol. 2011;18:1380-8.
- Carpizo DR, Are C, Jarnagin W, et al. Liver resection for metastatic colorectal cancer in patients with concurrent extrahepatic disease: results in 127 patients treated at a single center. Ann Surg Oncol. 2009;16:2138-46.
- Prasanna T, Karapetis CS, Roder D, et al. The survival outcome of patients with metastatic colorectal cancer based on the site of metastases and the impact of molecular markers and site of primary cancer on metastatic pattern. Acta Oncol. 2018; 57:1438-44.
- Nozue M, Oshiro Y, Kurata M, et al. Treatment and prognosis in colorectal cancer patients with bone metastasis. Oncol Rep. 2002;9(1):109-12.
- Damiens K, Ayoub JP, Lemieux B, et al. Clinical features and course of brain metastases in colorectal cancer: An experience from a single institution. Curr Oncol. 2012;19:254-8.
- Riihimaki M, Hemminki A, Sundquist J, et al. Patterns of metastasis in colon and rectal cancer. Sci Rep. 2016;6(1):1-9.
- Metastatic colorectal cancer may spread early in the disease, study find. 2019.
- Attili VS, Chandra CR, Dadhich HK, et al. Unusual metastasis in colorectal cancer. Indian J Cancer. 2006;43:93-5.
- Singh T, Amirtham U, Satheesh CT, et al. Floor-of-mouth metastasis in colorectal cancer. Ann Saudi Med. 2011;31(1):87-9.
- Meyer I, Shklar G. Malignant tumors metastatic to mouth and jaws. Oral surg oral med oral pathol. 1965;20(3):350-62.
- Dalirsani Z, Mohtasham N, Samiee N. Metastasis of colon adenocarcinoma to maxillary gingiva and palate. Iran J Otorhinolaryngol 2020;32(112):327.
- Romanet I, Lan R, Ordioni U, et al. A rare case of oral metastasis of colon adenocarcinoma. J Stomatol Oral Maxillofac Surg. 2018;119(3):229-31.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref