Brief Report - Virology Research Journal (2022) Volume 6, Issue 3
Distribution of dengue virus serotypes during the COVID 19 pandemic in Sri Lanka.
Fernando MAY1, Wijewickrama RT1, Gunathilaka JPLT1, Madarasinghe NS1, Abeynayake CC2, Janaki Abeynayake1*
1Department of Virology, Medical Research Institute, Dr.Danister De SilvaMawatha (Baseline Road), Colombo 08, Western Province, Sri Lanka
2Ministry of Health, Suwasiripaya, Baddegama Wimalawansa Mawatha, Colomo10, Sri Lanka
- Corresponding Author:
- Janaki Abeynayake
Department of Virology
Medical Research Institute
Dr.Danister De SilvaMawatha( Baseline Road)
Colombo 08, Western Province, Sri Lanka
E-mail: janakiiabeynayake@yahoo.com
Received: 28-April-2022, Manuscript No. AAVRJ-22-59366; Editor assigned: 30-April-2022, PreQC No. AAVRJ-22-59366 (PQ); Reviewed: 14-May-2022, QC No. AAVRJ-22-59366; Published: 21-May-2022, DOI: 10.35841/AAVRJ-6.3.111
Citation: Abeynayake JI, Distribution of Dengue Virus serotypes during the COVID 19 pandemic in Sri Lanka. Virol Res J. 2022;6(3):111
Keywords
Dengue virus (DENV) infection, Incidence, Serotype distribution, COVID -19 pandemic.
Background
DENV infection is an expanding major public health burden which has rapidly spread over all WHO regions in the recent years. Many tropical and subtropical countries are profoundly affected by the DENV infection including Sri Lanka, in which it has been highly endemic in the past few decades with significant impact on health services [1].
DENV infection is caused by the DENV, a single stranded positive sense RNA virus belonging to the Family Flaviviridae. It is transmitted via the female Aedes mosquitoes, mainly Aedes aegypti and Aedes albopictus. Four distinct serotypes of the virus (DENV-1, 2, 3, and 4) have been identified with evidence of long-lasting homotypic and short-lasting heterotypic immunity following infection with a single serotype [2]. However, some studies have stated on cases of homotypic reinfections one to two years after the primary infection [3]. Re-infection with another serotype has more potential to cause severe infection due to the cross reactivity of the immune response caused against a specific serotype [4,5]. It is evident that all 4 serotypes of the virus can cause severe DENV infection, while some genotypes or clades within genotypes are linked to increased potential for clinical severity [6,7]. However, studies have shown more complicated disease to be associated with DENV-2 [8]. Further, co-infection with two different serotypes has shown to be associated with more severe infection in some studies [9].
Circulation of different DENV serotypes in a specified geographical location overtime as well as co-circulation of multiple serotypes during a single outbreak has been documented [10]. Yet, usually one serotype acts as the predominant circulating type leading to a major outbreak at one point. This leads to waning-off of immunity to the other serotypes among the population which head to another outbreak with another emerging serotype in future [11,12].
It is evident that all four serotypes of the DENV have been circulating in Sri Lanka for more than 30 years. Sri Lanka has experienced several epidemics of DENV infection in the past and the appearance of new genotypes and clades within serotypes have found to be responsible for the increase in the incidence and epidemics [13]. Thus, knowledge on the distribution of the DENV serotypes will provide important information on an impending epidemic in near future. Moreover, it is highly important to detect the re-emerging serotypes and the disease burden of DENV infection during the current COVID-19 pandemic, as the combined effect of COVID-19 and dengue epidemics will potentially result in a severe health impact [1]. The first case with COVID-19 infection in Sri Lanka was reported on the 27th of January 2020 with the detection of the virus in a foreign traveler from China. A significant impact on health services in Sri.
Lanka was experienced with the commencement of the first wave of COVID-19 infection in March, 2020 followed by the second and third waves in October, 2020 and April, 2021 respectively. Further, several correlations of Dengue virus infection with COVID-19 infection have also been identified such as similar clinical presentations, reports of co-infection and serological cross reactivity between the two viruses, leading to difficulties in the management. [14,15].
Objective
The objective of this study was to describe the incidence of DENV infection and the distribution of DENV serotypes among clinically suspected patients with DENV infection during the COVID-19 pandemic in Sri Lanka.
Study Design
This laboratory based retrospective study was carried out at the National Arbovirus/Dengue Laboratory at the Medical Research Institute, Sri Lanka. The study included samples received for testing of DENV RNA from throughout the country from patients clinically suspected with DENV infection which were collected within five days of the onset of illness. Clinically suspected DEV infection was defined as presence of two or more clinical findings in a febrile patient ranging from nausea, vomiting, rash, arthralgia, myalgia, leucopenia, abdominal pain/tenderness, signs of fluid accumulation, mucosal bleeding, lethargy, restlessness and liver enlargement. Severe dengue was defined as presence of severe plasma leakage, severe bleeding or severe organ impairment in a patient with DENV infection [16]. A total of 1796 plasma samples fulfilling the above criteria received from May 2019 to April 2021 were recruited for testing for the presence of DENV RNA and the serotypes. Demographic and clinical details were recruited from the accompanying request forms.
RNA extraction from the samples was carried out using the SpinStar viral nucleic acid extraction kit (ADT Biotech, Malaysia) and was performed according to the manufacturer’s instructions. Any remaining ethanol was removed prior to amplification with an additional step of centrifugation. An elution volume of 60μl was used for testing.
DENV RNA detection and serotyping were carried out using the RealStar® Dengue Type Kit 1.0, a commercially validated qualitative real time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) assay manufactured by Altona Diagnostics GmbH, Hamburg, Germany. Reverse transcription, amplification and realtime detection were done using the ABI 7500 platform. Validation of the assay and interpretation of results were performed adhering to the manufacturer’s instructions.
The results were analyzed using the SPSS version 23, using descriptive statistics and chi -square tests.
Results
DENV Viraemic Rate during the study period
A total of 1796 plasma samples were tested of which 69.2% (n=1243) became positive for DENV RNA. The vireamic rate ranged from 31.9% to 80.12% during different quarters of the two-year study duration, which has decreased from between 70.68 to 80.12% to between 31.9 to 48.14%. Table 1 illustrates the DENV viraemic rate detected over the study duration.
| Quarters of the year | Viraemic rate, n(%) | ||
|---|---|---|---|
| Year 2019 | Year 2020 | Year 2021 | |
| January to April | N/A | 383 (80.12%) | 43 (38.7%) |
| May to August | 464 (70.73%) | 39 (48.14%) | N/A |
| September to December | 299 (70.68%) | 15 (31.9%) | N/A |
N/A- No data available.
Table 1. DENV viraemic rate during the quarters of the study period.
Demographic characteristics of the DENV viremic samples
Of the vireamic samples 55.34% (n=688) belonged to patients under 16 years of age. Features of severe dengue were observed in 20.99% (n=261) while 0.24% (n=3) of patients had features suggestive of encephalitis. Majority of the viraemic samples belonged to patients from the Western province (66.21%, n=823) followed by the Southern province (22.36%, n=278). The demographic characteristics of the DENV viraemic samples are demonstrated in Table 2.
| Variable | Frequency, n(%) |
|---|---|
| Age | |
| Children (<16 years) | 688 (55.34%) |
| Adults (≥ 16 years) | 555(44.65%) |
| Clinical presentation | |
| Non severe dengue | 911 (73.29%) |
| Severe dengue without encephalitis Severe dengue with encephalitis |
261 (20.99%) 3 (0.24%) |
| No data | 68 (5.47%) |
| Georgraphical distribution | |
| Western Province | 823 (66.21%) |
| Southern Province | 278 (22.36%) |
| North-Eastern Province | 127 (10.21%) |
| Other Provinces | 15 (1.2 %) |
Table 2. The demographic characteristics of the DENV viraemic samples.
DENV serotype distribution during the study period
Among the DENV viraemic samples DENV-2 was detected in 40.2% (n=500) followed by DENV-3 (37.97%, n=472) and DENV-1 (15.44%, n=192). DENV-4 infections were detected only in 0.56% (n=7) of the samples. Co-infection with two different serotypes was observed in 5.79% (n=72) of the samples of which co-infection with DENV-1 and DENV- 3 was detected in a majority (4.74%, n=59). Co-infection with DENV-2 and DENV-3 was identified in 0.56% (n=7) while DENV-1 and DENV-2 and DENV-1 and DENV-4 coinfection were detected in 0.45% (n=5) and 0.08% (n=1) of the samples respectively. The serotype distribution of DENV infection over the study period is depicted in Table 3.
| DENV serotypes | Frequency, n (%) |
|---|---|
| DENV-1 | 192 (15.44%) |
| DENV-2 | 500 (40.2%) |
| DENV-3 | 472 (37.97%) |
| DENV-4 | 7 (0.56%) |
| DENV- 1& 3 | 59 (4.74%) |
| DENV- 2 & 3 | 7 (0.56%) |
| DENV- 1 & 2 | 5 (0.45%) |
| DENV-1 & 4 | 1 (0.08%) |
Table 3. The serotype distribution of DENV infection over the study period.
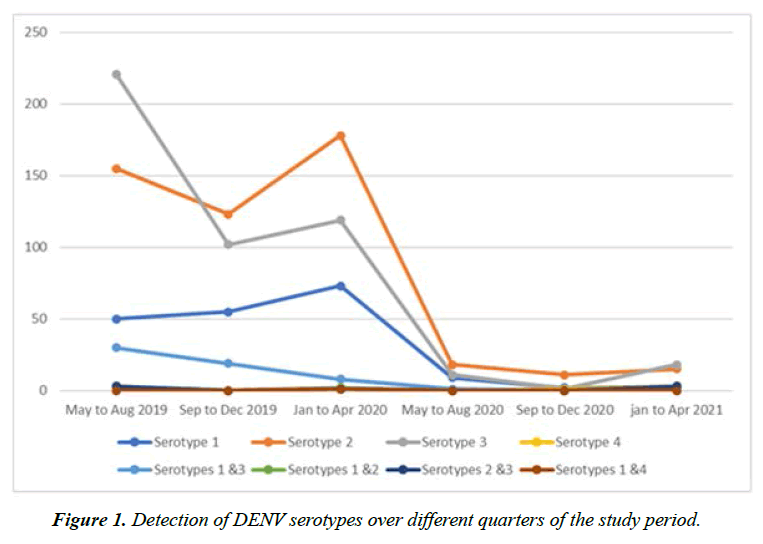
DENV-3 was the predominant serotype detected (47.62%, n=221) in the samples tested from May to August 2019, followed by DENV-2 (33.4%, n=155), DENV-1 (10.7%, n=50) and co-infection with DENV- 1 and DENV-3 (6.4%, n=30). From September 2019 to August 2020 DENV-2 was detected as most prevalent (44.2%, n=319) with detection of DENV-3 in 32.1% (n=232) and DENV-1 in 19% (n=137) of the samples. DENV-2 predominated the samples (23.4%, n=11) tested from September to December 2020 followed by DENV-1 and DENV-3, while DENV-3 was detected in predominance in the samples tested from January to April 2021. Figure 1 elaborates the detection of DENV serotypes over different quarters of the study period.
Correlation of clinical features with the DENV serotype distribution
Of the clinical presentations DENV-3 infection exhibited the highest detection (47.5%, n=124) in patients with severe DENV infection followed by DENV-2(39.46%, n=103). Further all three patients with features of encephalitis were suffering from DENV-3 infection. Of the patients infected with two different DENV serotypes 14.7% showed features of severe DENV infection (Table 4). The clinical features of DENV infection were significantly associated with the DENV serotype distribution (p<0.001) in this study.
| Clinical presentation | Frequency, n(%) | |||||
|---|---|---|---|---|---|---|
| DENV-1 | DENV-2 | DENV-3 | DENV-4 | Co-infection * | ||
| Non severe DENV infection | 158 (17.3%) |
372 (40.8%) |
322 (35.4%) |
5 (0.54%) |
54 (5.92%) |
|
| Severe DENV infection without encephalitis Severe DENV infection with encephalitis |
19 (7.2%) |
103 (39.4%) |
124 (47.5%) 3 (100%) |
1 (0.38%) |
10 (3.8%) |
|
| No data | 15 (20.8%) |
25 (34.7%) |
23 (31.9%) |
1 (1.38%) |
8 (11.1%) |
|
*Co-infection with DENV- 1 & 3, 1 & 2, 2 & 3 and 1 & 4
Table 4. Correlation of clinical features with the DENV serotype distribution.
Discussion
This study was conducted with the aim of detecting the incidence of DENV infection and the distribution of the DENV serotypes during the COVID-19 pandemic in Sri Lanka.
The study sample included predominantly children less than 16 years of age whereas the clinical presentations varied from non-severe to severe DENV infection. Majority of the samples were received from the Western province.
The overall incidence of DENV infection from May 2019 to April 2021 was detected as 69.2% in this study. The incidence has shown a marked decrease from between 70.73 to 80.12% to between 31.9 to 38.7% from May 2019 to April 2021. Similar findings have been observed in a study carried out in China which has demonstrated a decrease in the incidence of DENV infection during the COVID-19 pandemic [17]. However, both a reduction as well as an increase in incidence overtime has been reported in a study carried out in Malaysia [18]. At the same time the World Health Organization is anticipating an increase in the incidence of DENV infection with the current COVID-19 pandemic, especially to affect geographies with higher population density [1]. Therefore, continuous follow up studies will be required to monitor the progression of the incidence of DENV infection with time in Sri Lanka.
Majority of the DENV viraemic samples belonged to children less than 16 years of age. This study finding showed similarity to findings observed during a major DENV outbreak in Sri Lanka in 2017 [19]. Further, similar findings have also been observed globally owing to increased engagement in outdoor activities seen in this age group [20-23]. Features of non-severe DENV infection predominated the clinical presentation among the vireamic samples, in agreement with previous study findings in Sri Lanka as well as globally [21,24]. Majority of the viraemic samples were received from the Western province followed by the Southern province, probably indicating the impact of higher population density leading to increased incidence of infection.
DENV-2 was detected predominantly during this study period. Further, DENV-3 also demonstrated a similarly high incidence. Several studies have demonstrated DENV-2 infection to be associated with more severe clinical disease [12,22]. Similarly, in this study a high percentage of patients with severe dengue infection were infected with DENV- 2, while the percentage of severe clinical disease among patients with DENV-2 infection was higher compared to infection with DENV-1. At the same time according to some studies primary infection with DENV-3 is also documented to result in severe clinical disease [2]. Similarly, the highest percentage of patients with severe DENV infection were infected with DENV-3 in this study while among all the serotypes, DENV- 3 infection exhibited the highest percentage of patients with severe disease within a serotype. However, differentiation of primary and secondary dengue infection was not performed in this study.
DENV-2 and DENV-3 exhibited dominance throughout the study period, with either type showing predominance at a given period during the study duration. Similarly, dominance of DENV-2 and DENV-3 has been observed in Sri Lanka in outbreaks between 2003 to 2006 as well as during the major outbreak in year 2017 [19,21].
Interestingly re- emergence of DENV-1 was detected in this study. DENV-1 was lastly identified as the predominating serotype in Sri Lanka in year 2013 with no documented outbreaks thereafter. Evidence indicates low level of population immunity to a given serotype in a geographical location to predispose to an epidemic in future [11,12]. Thus, the increase prevalence of DENV-1 infection detected in this study may indicate re-emergence of DENV-1 following a low population immunity owing to predominant circulation of other serotypes in the recent past in Sri Lanka. Further this finding may indicate the probability of an impending outbreak of infection with DENV-1 in near future.
The present study indicated co-circulation of DENV- 1,2 and 3 in Sri Lanka, whereas detection of DENV-4 was markedly low. In contrary studies carried out during the major outbreak in 2017 have demonstrated co-circulation of DENV- 2, 3 and 4 [19]. However, it was noted in early 2019 that DENV-2 and DENV-3 continued to be predominant, while a rise in the prevalence of DENV-1 infection was demonstrated, indicating a gradual shift in the serotype distribution.
Co-infection with two different DENV serotypes was detected among study samples in this study. Similar study findings have been detected globally in several other studies carried out in the past [25]. Though DENV-2 and DENV-3 were the predominant circulating serotypes, co-infections were detected mainly with DENV-1 and DENV-3 in this study. This was in contrary to past study findings which have detected co-infections to be commonly present with the predominantly circulating serotypes [25]. Some study findings have indicated co-infection to be associated with severe disease [9] while other studies have not detected a difference in the clinical outcome [26]. The percentage of severe disease detected in patients with co-infection was lower than with infection with a single serotype in this study.
Conclusion
In conclusion, the incidence of Dengue virus infection has shown a noticeable decrease during the study period in Sri Lanka. Infection with DENV-2 and DENV-3 exhibited dominance with re-emergence of DENV-1 infection as well as co-infection with multiple serotypes. Infections with DENV-2 and DENV-3 were detected with severe infection predominantly.
Acknowledgment
Authors would like to acknowledge all the staff members at the Department of Virology at Medical Research Institute for their immense support. This research did not receive any specific grant from funding agencies in the public, commercial, or notfor- profit sectors.
Disclosure Statement
Authors would like to declare that there are no potential conflicts of interests.
References
- World Health Organization, Dengue and Severe Dengue. https://www.who.int/news-room/fact-sheets/detail/dengue-and-severe-dengue.
- Soo K, Khalid B, Ching S, Chee H. Meta-Analysis of Dengue Severity during Infection by Different Dengue Virus Serotypes in Primary and Secondary Infections. PLoS ONE. 2016;11(5):e0154760.
- Waggoner JJ, Balmaseda A, Gresh L, et al. Homotypic Dengue Virus Reinfections in Nicaraguan Children. J Infect Dis. 2016;214(7):986-93.
- Halstead SB. Neutralization and antibody-dependent enhancement of dengue viruses. Adv Virus Res. 2003;60:421-67.
- Rothman L. Dengue: defining protective versus pathologic immunity. J Clin Invest. 2004;113(7):946-51
- Leitmeyer KC, Vaughn DW, Watts DM, et al. Dengue virus structural differences that correlate with pathogenesis. J Virol. 1999;73(6):4738-47.
- Messer WB, Gubler DG, Harris E, et al. Emergence and global spread of a dengue serotype 3, subtype III virus. Emerg Infect Dis.2003;9:800–09.
- Vicente CR, Herbinger K, Fröschl G. Serotype influences on dengue severity: a cross-sectional study on 485 confirmed dengue cases in Vitória, Brazil. BMC Infectious Diseases. 2016;16:320.
- Dhanoa SS, Hassan CF, Ngim CF, et al. Impact of dengue virus (DENV) co-infection on clinical manifestations, disease severity and laboratory parameters. BMC Infect Dis. 2016; 16(1):406.
- Suwandono A, Kosasih H, Nurhayati R, et al. Four dengue virus serotypes found circulating during an outbreak of dengue fever and dengue haemorrhagic fever in Jakarta, Indonesia, during 2004. Trans R Soc Trop Med Hyg. 2006;100(9):855-62.
- Hapuarachchi HC, Koo C, Rajarethinam J, et al. Epidemic resurgence of dengue fever in Singapore in 2013–2014: A virological and entomological perspective. BMC Infect Dis. 2016;16:300
- Rodriguez-Roche R, Blanc H, Bordería AV, et al. Increasing clinical severity during a dengue virus type 3 Cuban epidemic: deep sequencing of evolving viral populations. J Virol. 2016;90(9):4320-33.
- Dayananda PD, de Silva H, Fernando L, et al. Genetic Variation in the Domain II, 3′ Untranslated Region of Human and Mosquito Derived Dengue Virus Strains in Sri Lanka. Viruses 2021;13(3):421.
- Bicudo N, Bicudo E, Costa JD, et al. Co-infection of SARS-CoV-2 and dengue virus: a clinical challeng. Braz J Infect Dis. 2020;24(5):452-54.
- Nath H, Mallick A, Roy S, et al. Archived dengue serum samples produced false-positive results in SARS-CoV-2 lateral flow-based rapid antibody tests. J Med Microbiol. 2021;70(6):001369
- Centers for Disease Control and Prevention, National Center for Emerging and Zoonotic Infectious Diseases (NCEZID), Division of Vector-Borne Diseases (DVBD) Page last reviewed:2021
- Jiang L, Liu Y, Su W, et al. Decreased dengue cases attributable to the effect of COVID-19 in Guangzhou in 2020. PLoS Negl Trop Dis. 2021;15(5):e0009441.
- Ong SQ, Ahmad H, Mohd Ngesom AM. Implications of the COVID-19 Lockdown on Dengue Transmission in Malaysia. Infect Dis Rep. 2021;13(1):148-160.
- Abeynayake JI, Welmillage SU, Gunasena S. Serotype-specific detection of dengue viruses in a multiplex real-time reverse transcriptase PCR. The Bulletin of Sri Lanka College of Microbiologist. 2017;15.
- Alia S, Khanb AW, Taylor-Robinson AW, et al. The unprecedented magnitude of the 2017 dengue outbreak in Sri Lanka provides lessons for future mosquito-borne infection control and prevention. Infection, Disease & Health. 2018;23(2):114-20.
- Jayarajah U, Faizer S, De Zoysa IM, et al. A Large Dengue Epidemic Affects Sri Lanka In 2017. International Journal of Progressive Sciences and Technologies. 2017; 6(1):84-86.
- Kularatne SA, Gawarammana IB, Kumarasiri PR, et al. Epidemiology, clinical features, laboratory investigations and early diagnosis of dengue fever in adults: a descriptive study in Sri Lanka. Southeast Asian J Trop Med Public Health. 2005;36(3):686-92.
- Messer WB, Kanakaratne N, Thevanesam V, et al. Clinical features of hospitalized dengue patients in Sri Lanka from 2004 to 2006. Sri Lanka Journal of Infectious Diseases.2012; 1(2):9-18.
- Udayanga L, Gunathilaka N, Iqbal MCM, et al. Comprehensive evaluation of demographic, socio-economic and other associated risk factors affecting the occurrence of dengue incidence among Colombo and Kandy Districts of Sri Lanka: a cross-sectional Study. Parasites Vectors. 2018;11(1):478.
- Vicente CR, Herbinger KH, Froschl, G et al. Serotype influences on dengue severity: a cross-sectional study on 485 confirmed dengue cases in Vitória, Brazil. BMC Infect Dis. 2016;16:320.
- Vaddadi K, gandikota C, Jain PK, et al. Co-circulation and co-infections of all dengue virus serotypes in Hyderabad, India 2014. Epidemiology & Infection. 2017;145(12):2563-74.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref