Research Article - Current Trends in Cardiology (2018) Volume 2, Issue 1
Comparison of the two dimensional versus three dimensional transthoracic echocardiography in assessment of mitral regurgitation.
- *Corresponding Author:
- Kavita Tyagi
Interventional Cardiology Ospedale, Max Superspeciality Hospital, Saket, Delhi
E-mail: drkavitatyagi@gmail.com
Accepted June 21, 2017
Citation: Kavita Tyagi. Comparison of the two dimensional versus three dimensional transthoracic echocardiography in assessment of mitral regurgitation. AACC 2018;2(1):10-15.
Abstract
The mitral valve is a complex structure1 .Mitral regurgitation is often referred to as organic, if there is an intrinsic valve disease, or functional, if the valve is structurally normal but leaks as a result of an extravalvular abnormality, such as an alteration in left ventricle chamber geometry and/or dilatation of the mitral annulus that adversely affects normal coaptation of the mitral valve leaflets during systole .Ischemic MR may be organic (ruptured or ischemic papillary muscle) and/or functional because of LV chamber dilatation. Nonischemic MR may be organic e.g., rheumatic or functional e.g., dilated cardiomyopathy. In contrast to conventional 2 dimensional echocardiography, which only displays the mitral valve leaflets en face from the left ventricle perspective, 3D echocardiography enables en face visualization from both left ventricle and left atrial perspectives. The latter view is also known as the ‘‘surgical view,’’ because it resembles the intraoperative image of the mitral valve after the surgeon, standing on the patient’s right side, opens the left atrium2. Two-dimensional echocardiography is not able to provide data about mitral annular shape, because mental reconstruction from separate 2D views cannot provide the same information as the volume-rendered 3D reconstruction. Instead, the oval shape of the mitral annulus is best appreciated from the 3DE surgical view of the mitral valve with the entire annular circumference captured in one data set. Moreover, the saddle shape of the mitral valve is best assessed by offline reconstructions, which depict the saddle shaped contour in three dimensions with high points that are anterior and posterior and low points that are lateral and medial . In addition, dynamic 3 dimensional rendering of the mitral valve can discriminate between normal leaflet mobility and tethered leaflets due to regional wall motion abnormalities or global left ventricular enlargement with increased sphericity (resulting in ischemic or functional mitral regurgitation). Despite proven superiority of three dimensional echocardiography over two-dimensional echocardiography no Indian studies are available comparing the two modalities. Considering above factors we decided to take up this study at our center to compare the assessment of mitral regurgitation by two dimensional versus three dimensional transthoracic echocardiography .
Keywords
Transthoracic echocardiography, rheumatic, diabetes, heart disease, atrial fibrillation
Introduction
The mitral valve is a complex structure [1]. Mitral regurgitation is often referred to as organic, if there is an intrinsic valve disease, or functional, if the valve is structurally normal but leaks as a result of an extra valvular abnormality, such as an alteration in left ventricle chamber geometry and/or dilatation of the mitral annulus that adversely affects normal coaptation of the mitral valve leaflets during systole. Ischemic MR may be organic (ruptured or ischemic papillary muscle) and/or functional because of LV chamber dilatation. Nonischemic MR may be organic e.g, rheumatic or functional e.g, dilated cardiomyopathy. In contrast to conventional 2-dimensional echocardiography, which only displays the mitral valve leaflets en face from the left ventricle perspective, 3-D echocardiography enables en face visualization from both left ventricle and left atrial perspectives. The latter view is also known as the ‘‘surgical view’’ because it resembles the intraoperative image of the mitral valve after the surgeon, standing on the patient’s right side, opens the left atrium [2]. Two-dimensional echocardiography is not able to provide data about mitral annular shape, because mental reconstruction from separate 2-D views cannot provide the same information as the volume-rendered 3-D reconstruction. Instead, the oval shape of the mitral annulus is best appreciated from the 3-D surgical view of the mitral valve with the entire annular circumference captured in one data set. Moreover, the saddle shape of the mitral valve is best assessed by offline reconstructions, which depict the saddle shaped contour in three dimensions with high points that are anterior and posterior and low points that are lateral and medial. In addition, dynamic 3 dimensional rendering of the mitral valve can discriminate between normal leaflet mobility and tethered leaflets due to regional wall motion abnormalities or global left ventricular enlargement with increased sphericity (resulting in ischemic or functional mitral regurgitation). Despite proven superiority of three dimensional echocardiography over two-dimensional echocardiography no Indian studies are available comparing the two modalities. Considering above factors we decided to take up this study at our centre to compare the assessment of mitral regurgitation by two dimensional versus three dimensional transthoracic echocardiography.
Methods
This study was conducted in the Department of Cardiology of ‘Sir Ganga Ram Hospital’, New Delhi from June, 2013 to April, 2015. Sample size of 80 was calculated using the formula (Z² × p × q)/d²), p=70%, precision error of estimation d=0.10 and alpha=0.05.
Inclusion criteria were patients diagnosed to have mitral regurgitation by clinical and two Dimensional Transthoracic Echocardiography who have given informed consent. Exclusion criteria were non co-operation by the patient, mitral stenosis and congestive heart failure. Patient information was documented in a proforma including presenting complaints, present, past, personal and family history, with details of duration of disease. The diagnosis was on the basis of clinical and two Dimensional Transthoracic Echocardiographic findings. Real-time three dimensional echocardiography was performed and recorded in parallel with a routine, comprehensive two-dimensional (2-D) study, by two separate echo-cardiographers. Both echo-cardiographers were blind to each other’s observations in order to avoid biases. The mitral valve leaflets, annulus, quantification of mitral regurgitation, were studied by both modalities. The three dimensional volumes were sliced offline in the three dimensions to selectively display specific cardiac structures along with real time three dimensional acquisition. Statistical testing was conducted with the statistical package for the social science system version SPSS 17.0.
Results
Out of 80 subjects, 27 (33.8%) were males and 53 (66.3%) were females and the mean age was 54.68 ± 14.02 years. Annulus transverse diameter was found to be 37.29 ± 6.68 mm by 2-d echo and 42.75 ± 6.10 mm by 3-d echo p<0.001. Vena contracta width was 5.80 ± 1.59 mm by 2-d echo and by 3-d echo it was 7.66 ± 4.77 mm, p value being 0.001 (Table 1).
| 2D Group | 3D Group | P Value | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Annulus (mm) | 37.29 ± 6.68 | 42.75 ± 6.10 | <0.001 |
| Vena contracta (mm) | 5.80 ± 1.59 | 7.66 ± 4.77 | 0.001 |
| ERO | 33.17 ± 19 | 47.97 ± 21.94 | <0.001 |
Table 1: Table showing differences in 2-d and 3-d measurements of transverse diameter of annulus, vena contracta and effective regurgitant orifice.
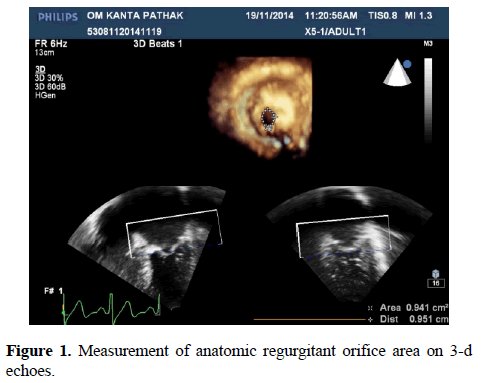
The Effective Regurgitant Orifice Area was calculated by PISA method with 2-d echo which was found to be 33.17 ± 19 mm. It was compared with Anatomic Regurgitant Orifice Area measurements by 3-d echo which was 47.97 ± 21.94 mm, p<0.001 (Figure 1).
A1 segment of anterior mitral leaflet was normal in 51 (63.8%) patients with 2-d echo while it was normal in 29 (36.3%) of patients with 3-d echo, p<0.001 (Tables 2-4).
| A1 | 2D Group | 3D Group | P Value | ||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| EM | 10 | 12.60% | 8 | 10% | <0.001 |
| N | 51 | 63.80% | 29 | 36.30% | |
| P | 4 | 5.00% | 35 | 43.80% | |
| RM | 15 | 18.80% | 8 | 10% | |
| Total | 10 | 12.60% | 80 | 100% | |
Table 2: Showing percentage of excess mobility, normal mobility, and prolapsing, restricted mobility of A1 segment of anterior mitral leaflet.
| A2 | 2D Group | 3D Group | P Value | ||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| EM | 8 | 10% | 6 | 7.50% | <0.001 |
| N | 51 | 63.80% | 24 | 30% | |
| P | 7 | 8.80% | 40 | 50% | |
| RM | 14 | 17.50% | 10 | 13% | |
| Total | 80 | 100% | 80 | 100% | |
Table 3: Showing percentage of excess mobility, normal mobility, and prolapsing, restricted mobility of A2 segment of anterior mitral leaflet.
| A3 | 2D Group | 3D Group | P Value | ||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| EM | 8 | 10% | 6 | 7.50% | <0.001 |
| N | 52 | 62.00% | 33 | 41.30% | |
| P | 7 | 8.80% | 33 | 41.30% | |
| RM | 13 | 16.30% | 8 | 10% | |
| Total | 80 | 100% | 80 | 100% | |
Table 4: Showing percentage of excess mobility, normal mobility, and prolapsing, restricted mobility of A3 segment of anterior mitral leaflet.
The prolapse of this segment was seen in 4 (5.0%) of patients with 2-d echo but with 3-d echo it was seen in 35 (43.8%) of patients. Excess mobility was noted in 10 (12.6%) of patients by 2-d echo while by 3-d echo only in 8 (10%), it was noted. Restricted mobility was noted in 15 (18.8%) of subjects by 2-d echo and 8 (10%) by 3-d echo. A2 segment was found to be normal in 24 (30%) by 3-d echo while it appeared normal in 51 (63.8%) by 2-d echo, p<0.001. Prolapse of this segment was seen in 40 (50 %) of patients with 3-d echo which was seen in 7 (8.8%) of the patients with 2-d echo. Excess mobility and restricted mobility were found in less number of patients with 3-d echo: 6 (7.5%) and 10 (13%) respectively in contrast to the findings of excess mobility and restricted mobility with 2-d echo 8 (10%) and 14 (17.5%) respectively. Similarly A3 segment was found normal in 33 (41.3%) of the patients by 3-d which was found normal in 52 (62.0%) of patients by 2-d echo. Prolapsing segment was seen in 33 (41.3%) of patients by 3-d echo and only 7 (8.8%) of patients by 2-d echo. Excess mobility and restrictive mobility was seen in 6 (7.5%) and 8 (10%) by 3-d echo which was lesser than with 2-d echo 8 (10%) and 13 (16.3%) respectively (Tables 5-7).
| P1 | 2D Group | 3D Group | P Value | ||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| EM | 4 | 5% | 0 | 0.00% | <0.001 |
| N | 63 | 78.80% | 38 | 47.50% | |
| P | 1 | 1.30% | 30 | 37.50% | |
| RM | 12 | 15.00% | 12 | 15% | |
| Total | 80 | 100% | 80 | 100% | |
Table 5: Showing percentage of excess mobility, normal mobility, prolapsing, restricted mobility of P1 segment of posterior mitral leaflet.
| P2 | 2D Group | 3D Group | P Value | ||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| EM | 3 | 3.80% | 0 | 0.00% | <0.001 |
| N | 69 | 86.30% | 44 | 55.00% | |
| P | 0 | 0.00% | 29 | 36.30% | |
| RM | 8 | 10.00% | 7 | 8.80% | |
| Total | 80 | 100% | 80 | 100% | |
Table 6: Showing percentage of excess mobility, normal mobility, prolapsing, restricted mobility of P2 segment of posterior mitral leaflet.
| P3 | 2D Group | 3D Group | P Value | ||
|---|---|---|---|---|---|
| Frequency | % | Frequency | % | ||
| EM | 3 | 3.80% | 0 | 0.00% | <0.001 |
| N | 70 | 87.50% | 51 | 63.80% | |
| P | 0 | 0.00% | 23 | 28.80% | |
| RM | 7 | 8.80% | 6 | 7.50% | |
| Total | 80 | 100% | 80 | 100% | |
Table 7: Showing percentage of excess mobility, normal mobility, prolapsing, restricted mobility of P2 segment of posterior mitral leaflet.
P1 segment was seen to prolapse only in 1 (1.3%) of patients with 2-d echo and 30 (37.5%) patients with 3-d echo. It was found to be normal with 2-d echo in 63 (78.8%) while with 3-d echo it was normal in 38 (47.5%) of patients, p<0.001. Excess mobility was not seen even in single patient with 3-d echo while with 2-d echo it was seen in 4 (5%) of the patients. Restricted mobility was seen in equal number with both modalities of investigation 12 (15%).
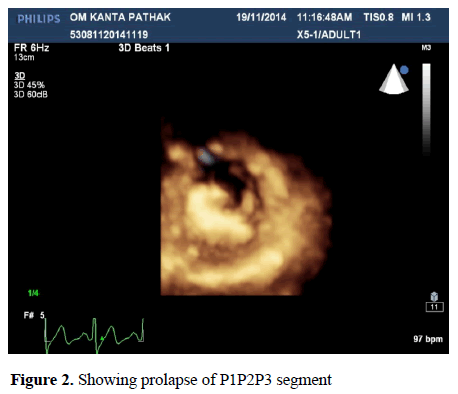
The P2 segment was found to be normal in 69 (86.7%) of the patients with 2-d echo while it was normal in 44 (55.0%) of the patients with 3-d echo, p<0.001. The prolapse segment was not seen in any of the patients with 2-d echo while it was seen in 29 (36.3%) of the patients with 3-d echo. Excess mobility was not seen in any patient with 3-d echo while it was seen in 3 (3.8%) of the patients with 2-d echo. Restricted mobility was seen in 7 (8.8%) of patients with 3-d echo while it was seen in 8 (10.0%) of the patients with 2-d echo. The P3 segment was found normal in 70 (87.5%) with 2-d echo, while it was normal in 51 (63.8%) of the patients with 3-d echo p<0.001. Prolapse segment was not seen in any of the patients with 2-d echo while it was seen in 23 (28.8%) of the patients with 3-d echo (Figure 2).
Excess mobility was seen in 3 (3.8%) of patients with the 2-d echo while it was not seen in any of the patient with 3-d echo. Restricted mobility was seen in 7 (8.8%) of the patients with 2- d echo and in 6 (7.5%) of the patients with 3-d echo.
Discussion
In the present study Mitral Valve was reconstructed en face from the left atrium (LA). AROA was measured by planimetry from 3-D pictures and compared to the EROA by proximal Isovelocity surface area and proximal MR jet width from 2-D echo. EROA with 2-d echocardiography was 33.17 ± 19 mm and with 3 echo it was 47.97 ± 21.94 mm. This difference was statistically significant p<0.001. Lange et al. studied 38 unselected patients [3]. Transesophageal echo (TOE) 3-D images were acquired; AROA was measured by planimetry from 3D pictures and compared to the effective regurgitant orifice area (EROA) by PISA and proximal MR jet width from 2-D echo. Good correlation was found between EROA and AROA measured from LA (r=0.97, P<0.0001). They came to conclusion that AROA enables quantification of MR with excellent agreement with the accepted clinical method of proximal flow convergence.
Altiok E evaluated direct measurement of anatomic regurgitant orifice area (AROA) by 3-dimensional transesophageal echocardiography [4]. In 72 patients (age 70.6 ± 13.3 years, 37 men) with mild to severe MR, 3-dimensional transesophageal echocardiography and transthoracic colour Doppler echocardiography were performed to determine AROA by direct planimetry, EROA by proximal convergence method, and vena contracta area (VCA) by 2-dimensional colour Doppler echocardiography. AROA determined by direct planimetry was 0.30 ± 0.20 cm², EROA determined by proximal convergence method was 0.30 ± 0.20 cm². Ashraf M Anwar evaluated the feasibility and possible additional value of transthoracic real-time three dimensional echocardiography (RT3D-TTE) for the assessment of cardiac structures as compared to 2D-TTE [5]. Their patients mean age was 45 ± 8.4 years, 75% males. Assessment of native (112 patients) and prosthetic (30 patients) valves morphology and functions was performed. Different shapes of vena contracta were found e.g. oval, circular, and irregular. The RT3D-TTE findings in 3 patient underwent MV surgery were similar to that obtained by intraoperative 2-D TEE and guided towards the proper surgical techniques of repair. de Agustın et al. did a Validation Study of Direct Measurement of PISA by Single-Beat Three- Dimensional Colour Doppler Echocardiography in Mitral Regurgitation [6]. According to authors this was the first study demonstrating that mitral EROA and Rvol can be reliably measured with transthoracic, single-beat, real-time 3-D colour Doppler echocardiography in the clinical setting. A limitation of this study of MR is the lack of a gold standard against which to compare the results of different methods. They concluded that the 3D PISA method may become the standard approach for determining EROA. Paaladinesh Thavendiranathan did a study to test the accuracy of an automated 3-dimensional (3D) proximal isovelocity surface area (PISA) (in vitro and patients) and stroke volume technique (patients) to assess MR severity using real-time volume colour flow Doppler transthoracic echocardiography [7]. The mean anatomic regurgitant orifice area (0.35 ± 0.10 cm2) was underestimated to a greater degree by the 2-D (0.12 ± 0.05 cm2) than the 3D method (0.25 ± 0.10 cm2; P<0.001 for both). It led to conclusion that Automated real-time 3-D volume colour flow Doppler based 3D PISA is more accurate than the 2D PISA method to quantify MR. However in our study we have not quantified MR by PISA on 3-d echo. Zaghlol et al. subjected fifty patients to both 2D and 3D transthoracic colour Doppler flow mapping techniques to assess mitral regurgitation by VC [8-10]. Their studied group of patients consisted of 50 patients, 28 males and 22 females. Their age ranged from 45 to 65 years with a mean of 55.1 ± 7.4 years. Thirty patients with ischemic or dilated cardiomyopathy, 11 patients with rheumatic heart diseases, and 9 patients with mitral valve prolapse. In patients with central jet mitral regurgitation, the VC width obtained by 2-D and 3-D were nearly equal (0.68 ± 0.22 cm vs. 0.65 ± 0.17 cm, p=0.063) and significantly correlated with effective regurgitant orifice area EROA (r=0.548, p=0.005 and r=0.747, p=0.001, respectively). In patients with eccentric jet of mitral regurgitation, the VC width measured by 2D overestimated the VC area measured by 3D echocardiography (0.67 ± 0.168 cm vs. 0.53 ± 0.174 cm, p=0.040) and this 2D VC width was poorly correlated with EROA (r=0.125, P=0.088). In contrast, the VC area measured by 3D echocardiography in patients with eccentric jet of mitral regurgitation correlated well with EROA (r=0.812, p=0.002). Conclusions drawn are that Real-time three dimensional echocardiography provides more accurate and highly reproducible assessment of VC cross-sectional area in patients with both central and eccentric mitral regurgitation than two-dimensional echocardiography. However in the present study jets were not classified in central and eccentric types. In the present study A1, A2, A3 of AML and P1, P2, P3 of PML were studied by both 2-d and 3-d echo. A1 segment of Anterior mitral leaflet was found to be normal in 51 (63.8%) patients with 2-d echo while it was found to be normal only in 29 (36.3%) of patients with 3-d echo, this difference is statistically significant p<0.001. The prolapse of this segment was seen only in 4 (5.0%) of patients with 2-d echo but with 3-d echocardiography it was seen in 35 (43.8%) of patients. Excess mobility was noted in 10 (12.6%) of patients by 2-d echo while by 3-d echo it was seen in 8 (10%). Restricted mobility was also noted in 15 (18.8%) of subjects by 2-d echocardiography and 8 (10%) by 3-d echo. In the present study A2 segment was found to be normal in 24 (30%) of the studied patients with 3-d echo while it was normal in 51 (63.8%) of patients with 2-d echo, making the difference statistically significant p<0.001. Prolapse was seen in 40 (50%) of patients with 3-d echo which was however seen only 7 (8.8%) of the patients by 2-d echo. Excess mobility and restricted mobility were found in less number of patients with 3-d echo 6 (7.5%) and 10 (13%) respectively in contrast to the findings of Excess mobility and restricted mobility by 2-d echo 8 (10%) and 14 (17.5%) respectively. In the present study A3 segment was found to be normal in 33 (41.3%) of the patients by 3-d and it was found normal in 52 (62.0%) of patients by 2-d echo. Prolapsing segment was seen in 33 (41.3%) of patients by 3 d echo and 7 (8.8%) of patients by 2-d echo. Excess mobility and restrictive mobility was seen in 6 (7.5%) and 8 (10%) by 3-d echo which was lesser than with 2-d echo 8 (10%) and 13 (16.3%) respectively. In conclusion, 3-d echo appears to be better at picking up the prolapse segment than 2-d echo and overall prevalence of prolapsed valve could be higher. In the present study P1 segment was seen to prolapse in 1 (1.3%) of patients with 2-d echocardiography and 30 (37.5%) patients with 3d echo. It was found to be normal with 2-d echo in 63 (78.8%) patients while with 3-d echo it was normal in 38 (47.5%) of patients, which was statistically significant p<0.001. Excess mobility was not seen even in single patient with 3-d echo while with 2-d echo it was seen in 4 (5%) of the patients. Restricted mobility was seen in equal number with both modalities of investigation 12 (15%) each. The P2 segment, in the present study was found to be normal in 69 (86.7%) of the patients with 2-d echo while it was normal in 44 (55.0%) of the patients with 3-d echo, which is statistically significant. The prolapse segment was not seen in any of the patient with 2-d echo while it was seen in 29 (36.3%) of the patients with 3-d echo. Excess mobility was not seen in any patient with 3-d echo while it was seen in 3 (3.8%) of the patients with 2-d echo. Restricted mobility was seen in 7 (8.8%) of patients with 3 d echo while it was seen in 8 (10.0%) of the patients with 2-d echo. The P3 segment was found normal in 70 (87.5%) with 2- d echo, while it was normal in 51 (63.8%) of the patients with 3-d echo which was statistically significant. Prolapse segment was not seen in any of the patients with 2-d echo while it was seen in 23 (28.8%) of the patients with 3-d echo. Excess mobility was seen in 3 (3.8%) of patients with the 2-d echo while it was not seen in any of the patient with 3-d echo. Restricted mobility was seen in 7 (8.8%) of the patients with 2-d echo and with 3-d echo, in 6 (7.5%) of the patients. The limitation of present studies was that, we did not differentiate among different shapes of vena contracta. We did not compare PISA results of 2-D with PISA results 3-D. Despite meticulous searching the literature we did not get any comparative study for assessing difference in capability of 2-d and 3-d for assessing the prolapse, excessive mobility and restrictive mobility. Our study has clearly shown 3-d echo superior to 2-d echo for measurements of vena contracta, anatomic regurgitant orifice area and it seems that 3-d echo is superior to 2-d echo in visualizing the prolapsed segment. 3-d echo doesn’t seem to differentiate restrictive mobility and excess mobility better than 2-d echo. Till now the accepted classification of mitral regurgitation solely depends on the measurements and other criterion on 2-d echocardiography and surgical decisions also largely depend on this. However if its proven in further studies, that mild or moderate mitral regurgitation might turn out to be severe, more number of patients might benefit from surgical intervention. To confirm our detailed individual segmental study findings, large studies are required including confirmation of results during surgery. By seeing the results of our study, it seems that prolapse of segments could be responsible for large number of mitral regurgitations in our population also. Annulus transverse diameter was also clearly found more on 3-d echo than 2-d echo. These measurements can have some surgical implications in future in terms of bigger sizes of prosthetic valves and their rings. The shape of mitral valve annulus, and its dynamics are being studied by various workers in great detail, however in our study details of annulus shape and dynamics were not studied. Vena contracta has also been found to be different shapes, when studied in different planes by 3-d echo. We also noted different shapes of vena contracta. In future, such studies can be undertaken in which we try to differentiate the dimensions of different shapes of vena contracta and their implications on the assessment of severity and treatment outcomes. Our values are the result of different types of pathological valves, due to time constraints, and small cohort of patients. In future we recommend conducting study for individual valve pathologies of different etiology and comparing them statistically in their own cohort. We also recommend PISA comparison of both the modalities and their cross comparison with anatomic regurgitant orifice area with 3-d echo. This study remains inconclusive about the role of excess mobility and restricted mobility in quantifying the severity of MR and which modality is better to assess them needs further studies. We conclude that mitral valve is more complex than what it has been perceived so far and extensive efforts are required in understanding not only dynamics of annulus but that of leaflets also.
Conclusions
Statistical difference in vena contracta width, annulus and effective regurgitant orifice are measurements may enable us to quantify much more moderate regurgitation as severe ones leading to need of more number of early interventions. However more long term studies are required to establish the standard values on 3-D echo. To confirm our findings of different scallops, large studies are required specially confirmation of results during surgery. Further large studies are required for studying various shapes of annulus and its dynamics. Studies are required to differentiate the different dimensions of different shapes of vena contracta and their implications on the assessment of severity and treatment outcomes. Effective Regurgitant orifices are by PISA method should be done by both 2-d echo and 3-d echo for comparison. Despite extensive search we could not find detail morphological and mobility study references, which could have helped us for comparative evaluation.
References
- Fuster V, Rourke R.O, Wilson P.P, et al. Mitral Valve Regurgitation Including the Mitral Valve Prolapse Syndrome. Hurst's The Heart. 2008; 1721.
- Lang RM, Badano LP, Tsang W, et al. EAE/ASE Recommendations for Image Acquisition and Display Using Three-Dimensional Echocardiography. J Am Soc Echocardiography. 2012; 25:3-46.
- Lange A, Palka P, Donnelly J, et al. Quantification of mitral regurgitation orifice area by 3-dimensional echocardiography: comparison with effective regurgitant orifice area by PISA method and proximal regurgitant jet diameter. Int J Cardiol. 2002; 86:87-98.
- Altiok E, Hamada S, van Hall S, et al. Comparison of direct planimetry of mitral valve regurgitation orifice area by three-dimensional transesophageal echocardiography to effective regurgitant orifice area obtained by proximal flow convergence method and vena contracta area determined by color Doppler echocardiography. Am J Cardiol. 2011; 107:452-8.
- Anwar AM, Nosir YF, Zainal-Abidin SK, et al. Real-time three-dimensional transthoracic echocardiography in daily practice: initial experience. Cardiovascular Ultrasound 2012; 10:14.
- de Agustín JA1, Marcos-Alberca P, Fernandez-Golfin C, et al. Measurement of Proximal Isovelocity Surface Area by Single-Beat Three-Dimensional Color Doppler Echocardiography in Mitral Regurgitation: A Validation Study. J Am Soc Echocardiogr. 2012; 25:815-23.
- Thavendiranathan P1, Liu S, Datta S, et al. Quantification of Chronic Functional Mitral Regurgitation by Automated 3-Dimensional Peak and Integrated Proximal Isovelocity Surface Area and Stroke Volume Techniques Using Real-Time 3-Dimensional Volume Color Doppler Echocardiography In Vitro and Clinical Validation. Circ Cardiovasc Imaging. 2013; 6:125-33.
- Zaghlol A, Deraz I, Kasem H. Role of Real-Time 3-Dimensional Echocardiography in Mitral Regurgitation Heart Mirror Journal 2012; 6:1687-6652.
- Khanna D, Vengala S, Miller AP, et al. Quantification of mitral regurgitation by live three-dimensional transthoracic echocardiographic measurements of vena contracta area. Echocardiography 2004; 218:737-43.