Research Article - Journal of Physical Therapy and Sports Medicine (2023) Volume 7, Issue 1
Arthroscopic anterior shoulder stabilisation: Get them moving early.
Sriskandarasa Senthilkumaran*Department of Trauma and Orthopaedic Surgery, Woodend General Hospital, Aberdeen, Scotland, United Kingdom
- *Corresponding Author:
- Sriskandarasa Senthilkumaran
Department of Trauma and Orthopaedic Surgery
Woodend General Hospital, Aberdeen
Scotland, United Kingdom
E-mail: kumaran26@hotmail.co.uk
Received: 06-Jan-2023, Manuscript No. AAJPTSM-23-86894; Editor assigned: 08-Jan-2023, PreQC No. AAJPTSM -23-86894;(PQ); Reviewed: 22-Jan-2023, QC No AAJPTSM -23-86894; Revised: 24-Jan-2023, QC No AAJPTSM -23-86894; Published: 30-Jan-2023, DOI:10.35841/aajptsm-7.1.134
Citation: Senthilkumaran S. Arthroscopic anterior shoulder stabilisation: Get them moving early. J Phys Ther Sports Med. 2023;7(1):134
Abstract
Introduction: There is clinical equipoise regarding postoperative rehabilitation following arthroscopic shoulder stabilisation. The aim of this study was to compare early mobilisation regime with standard protected regime.
Method: Twenty-eight patients who were undergoing arthroscopic anterior shoulder stabilisation for recurrent dislocation were recruited into this prospective randomised clinical trial. They were randomised to either Early Mobilisation (EM) or Sling Immobilisation (SI) group. The EM group was allowed to move the shoulder immediately within a limited range. The SI group was kept in a sling for 6 weeks. Primary outcome measure was failure rate at 2 years. Secondary measures were Oxford Shoulder Instability Score (OSIS) at 3 weeks, 6 weeks, 3 months, 6 months, 1 year and 2 years.
Results: There were no failures in the EM group; however SI group had 2 failures. There were no differences in the Oxford scores at any time points. The study was terminated prematurely as early results showed no significant difference between the two groups in terms of failure rate and functional scores throughout the follow up period.
Conclusion: Sling immobilisation does not appear to offer any advantage and may, in fact, be detrimental. Our results provide scientific evidence for early mobilisation following arthroscopic stabilisation surgery.
Keywords
Rehabilitation, Mobilisation, Sling immobilisation, Stabilisation.
Introduction
The shoulder joint is the most commonly dislocated joint with an incidence of 1.7%. Anterior dislocation is the most common (95%) direction for shoulder dislocation. Recurrent instability is common after a primary traumatic dislocation; with a rate of up to 95% in patients under the age of 20.1 most patients with recurrent instability after a traumatic shoulder dislocation need surgery. Arthroscopic reattachment of the capsulolabral complex using anchors is the treatment of choice for post traumatic recurrent instability in the absence of any significant bone defects [1]. Modern arthroscopic technique with suture anchors, are as effective as open techniques.
Open repair has been associated with failure rate of 0%-11% whilst arthroscopic techniques have reported failure rate about 8%-11%. Historically, higher failure rates of (33%) have been associated with arthroscopic procedures. Therefore, surgeons have historically been hesitant in allowing early mobilisation. There is clinical equipoise regarding postoperative rehabilitation following arthroscopic shoulder stabilisation surgery with most surgeons advocating immobilisation for a period of three weeks to six weeks to allow the ligaments to heal and prevent recurrence. However, one of the risks of prolonged immobilisation is residual shoulder stiffness [2].
Advocates of early mobilisation argue that there is no apparent increased risk of recurrence and excess stiffness is avoided. It also permits early strengthening and proprioception exercises.
Rehabilitation protocols from centres around the world vary greatly with most advocating sling immobilisation for period 3 weeks-6 weeks. Some centres strictly keep the arm in the sling at all times while others allow limited exercises within the first 3 weeks. Postoperative guidelines from the North Sydney orthopaedic and sports medicine centre focus on early range movement exercises with passive external rotation limited to 10 degrees and forward elevation to 90 degrees. The Vanderbilt Orthopaedic Institute changed their physiotherapy guidelines based on results of one study showed that early mobilisation improved functional outcomes [3]. They start their physiotherapy regimen on the third post-operative day with external rotation limited for 2 weeks.
From the currently available literature, there is very little evidence to support various rehabilitation protocols following anterior shoulder stabilisation surgery and there is no homogeneity in the recommendations between different specialist centres. They appeared to be based on surgeons’ preferences. We designed a randomised clinical trial with the aim to devise an evidence-based rehabilitation protocol following anterior shoulder stabilisation surgery. Our hypothesis was that early mobilisation does not have an adverse effect on recurrence rate and, in fact, should be beneficial in terms of improving shoulder function [4]. Therefore, there will be no difference in the failure rate between 2 groups but significantly better functional scores. Null hypothesis (H0) stated that sling immobilisation will protect against failure of the repair. Hence, there will be significantly fewer recurrences in this group of patients but with identical functional scores. We prematurely terminated our recruitment after three years as the results from both arms of the trial were showing no difference and it was felt unethical to continue with the study.
Materials and Methods
Patient selection
All patients undergoing arthroscopic anterior shoulder stabilisation surgery during 2010 to 2013 were approached and informed consents obtained.
Inclusion criteria
Patients with recurrent instability who had a Bankart lesion and were deemed suitable clinically and radiologically for an arthroscopic anterior shoulder stabilisation were included.
Exclusion criteria
Patients with previous failed stabilisation surgery, multidirectional instability or posterior instability were excluded. Patients who were unwilling to participate were also excluded.
Study design
This study was a prospective randomised clinical trial. It was initially powered for 60 patients with 30 in each group. On the day of surgery, participants were randomised to either Early Mobilisation (EM) or Sling Immobilisation (SI) groups using sealed envelopes. This information was recorded on the operation note and verbally communicated to the ward Physiotherapist. Blinding was not possible. The operations were performed by one of three consultant orthopaedic upper limb surgeons in a single centre. The procedure performed in all cases was an arthroscopic capsulolabral repair using a minimum of 3 suture anchors inserted into the glenoid. The patients were reviewed by a physiotherapist post-operatively who provided verbal and written instructions regarding the postoperative mobilisation, according to the randomisation, following surgery.
The EM Group was allowed to move the shoulder immediately post-operatively. They were given a sling for comfort for the first 2 days-3 days and advised to wear the sling at night. The only movement restrictions were abduction to 45 degrees and external rotation to 0 degrees.
The SI Group was predominantly kept in a sling for 6 weeks. For the first 3 weeks, they were completely immobilised at all times with a polysling and body belt. After 3 weeks, they were allowed to mobilise out of the sling for short periods to perform active exercises. The same restrictions i.e. abduction less than 45 degrees and limiting external rotation to zero degrees were applied, as with the EM group. The sling without the body belt was worn at all other times during weeks 4-6. Both groups began full Range of Motion (ROM), cuff strengthening and proprioception exercises at the 6-week mark. All patients were given posture advice and elbow, wrist and hand exercises from day 1 postoperatively (Table 1).
| EM group | SI group | |
|---|---|---|
| Phase I 0-3 weeks | Active ROM but limit external rotation to neutral (0°) and abduction to 45° sling at night only | Immobilised in sling with body belt |
| Phase II 3-6 weeks | Active ROM but limit external rotation to neutral and abduction to 45° sling at night only | Active ROM but limit external rotation to neutral and abduction to 45° sling at all other times except when exercising |
| Phase III After 6 weeks | Progress ROM, rotator cuff strengthening proprioception | Progress ROM, rotator cuff strengthening proprioception |
Table 1. Rehabilitation protocol.
Outcome measures
The primary outcome measure was failure of surgery which was defined as further anterior subluxation or re-dislocation. Secondary outcome measure was Oxford Shoulder Instability Score (OSIS) at 3 weeks, 6 weeks, 12 weeks, 26 weeks, 52 weeks and 104 weeks. OSIS is an uncomplicated self-reported assessment tool that is based on 12 relevant questions. It is specifically designed to measure the activity of daily living and pain levels in people with recurrent instability. It has been validated extensively in this group of patients and shown to have excellent reliability and reproducibility. The independent samples t-test was used to compare the outcome scores of the two patient groups at the predetermined time points. The Chi- squared test was used to analyse categorical data. Ethical approval was obtained from NRES Committee- North of Scotland in June 2010. The study was registered in ISRCTN registry (trial no. ISRCTN13628010).
Results
Patient selection
Thirty-three patients were screened, and five patients were excluded. Two of the patients declined to take part in the study and 3 others did not meet the inclusion criteria as they had multidirectional instability. Twenty-eight patients were recruited in to the study. Although the study was initially powered for 60 patients, recruitment ceased after 28 patients. This was due to a variety of factors which will be discussed later. No patients were excluded after recruitment.
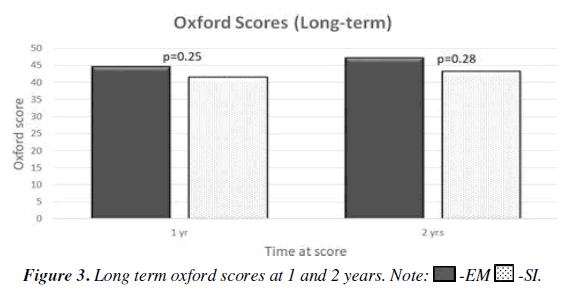
Three patients from each arm of the study failed to attend the first review clinic. They defaulted two further review appointments and were not included in the analysis. 22 patients were included in the analysis at 6 weeks, 3 months and 6 months. Two further patients from the SI group did not attend 1-year follow-up. Another two patients from each group failed to attend their 2-year follow-up. In total, 16 patients were included at the final 2-year analysis (Figure 1).
Demographics
There were more males (n=20) and females (n=2) among the participants. The mean age at the time of surgery was 32.1 years (range 18-54). There was no statistical difference in the basic demographics in term of age and gender distribution of both groups (Table 2).
| Sling immobilization | Early mobilization | |
|---|---|---|
| Mean age (yrs) | 32.3 | 31.9 |
| Range | 22-40 | 22-54 |
| Gender (M:F) | 0.458333 | 0.376389 |
Table 2. Distribution of patients in both groups.
Failure rate
No episodes of anterior subluxation or re-dislocation occurred in the EM group. In the SI group, one patient had re-dislocated at one year. Another patient in the SI group had recurrent subluxation. Therefore, the overall failure rate in the SI group was 18.1%. However, there was no statistically significant difference in the failure rate between the two groups (p=0.12). The overall failure rate was 9% for all patients.
One patient in the SI group had marked shoulder stiffness and subsequently needed an arthroscopic capsular release. No patients in the EM group experienced any complications. Overall, there were significantly more complications in the SI group (p=0.04).
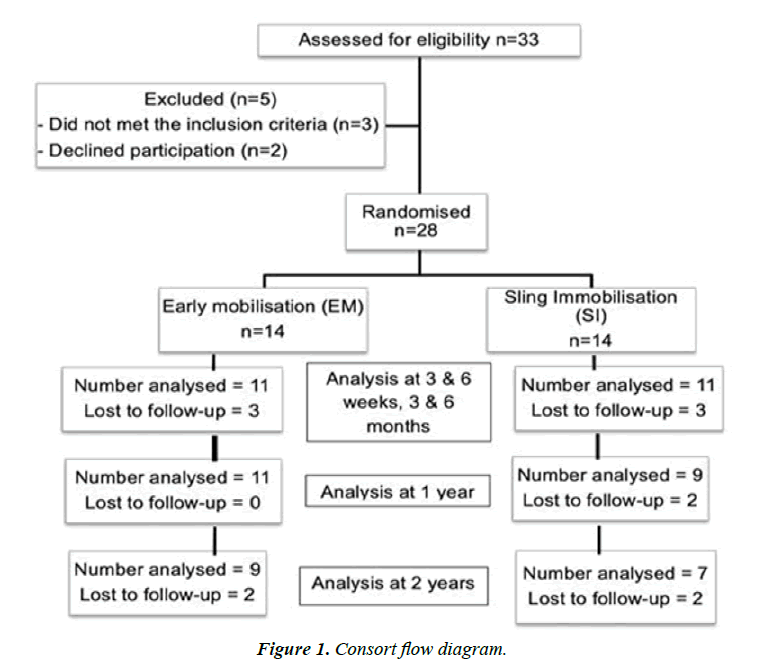
Functional scores
Pre-operative OSIS were 27.5 and 25.3 in the EM and SI groups respectively. In both groups, the first post-operative scores at 3 weeks were lower than the pre-op scores being 19.0 and 17.2 in the EM and SI groups respectively. As the pain decreased, the scores improved at 6 weeks to 25.6 and 25.9. At 6-months, the Oxford scores were 38.9 and 36.7 in the EM and SI groups respectively. The average short-term Oxford scores at 3 weeks, 6 weeks, 12 weeks and 6 months. There was no statistical difference between the two groups at any time. At 6 weeks, the functional scores were considered to be fair (score 20-29) in both groups. Only eight patients had good scores (30-38) at this time point. The number of patients reporting good scores increased to fifteen and nineteen patients at 3 months and 6 months respectively. Excellent functional scores (40-48) were observed in 17 patients at 1 year (Figure 2).
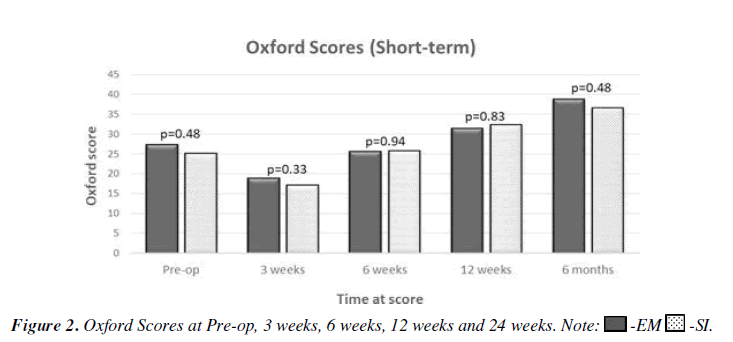
At 1 year, the mean OSIS scores were 44.7 and 41.2 in the EM and SI groups respectively. There was no significant difference between the two groups (p=0.25). Similar scores were observed at 2 years. The mean scores were 47.3 and 43.3 in EM and SI group respectively. Again, there was no significant difference between the two groups (p=0.28).
Inter group analysis showed that average OSIS scores were marginally better in the EM group than SI group. However, there were no significant differences in the scores. Intragroup analysis showed that there was a statistically significant improvement in functional scores from pre-op to 2-year follow up in both SI (p=0.0002) and EM (p=0.000) groups (Figure 3).
Discussion
Historically, open anterior shoulder stabilisation surgical techniques were associated with high recurrence rates post stabilisation, prompting surgeons to immobilise the shoulder joint for a period of time to allow for the soft tissues to heal adequately before commencing rehabilitation. With modern arthroscopic techniques, there is minimal insult to the soft tissues. Through the evolution of tissue anchors, suture materials and suturing techniques, the incidence of anterior subluxation and re-dislocation have decreased [5-8]. Despite these developments, many surgeons remain cautious and are slow to permit their patients to mobilise their shoulders actively.
Most of the published literature and guidelines on rehabilitation following arthroscopic stabilisation surgery is based on expert opinions and descriptive evidence, with limited level I or II evidence available. Our study is only the second randomised trial of its kind, looking at different rehabilitation regimes for arthroscopic shoulder stabilisation surgery.
The overall failure rate was 9% for all patients. This is comparable to the failure rates reported in the literature. Both failures happened at approximately one year following surgery and both were in the immobilised group. This finding is not statistically significant and may be explained by the small sample size. However, there were significantly more complications in the SI group when other complications such as shoulder stiffness were taken into account.
The initial post-operative Oxford scores were low in both groups due to pain, limitation of activities and lack of confidence in using the shoulder. The mean functional improved steadily with time in both groups 6 weeks after surgery [9]. By 1 year, seventeen patients rated their function as excellent. Nineteen patients gained the benefit of surgery (good-excellent scores) between 6 months and 1 year. Scores at 2 years are significantly better than the pre-operative scores when analysed within each group.
Recruitment was terminated prematurely after three years. This was primarily because our early results suggested that sling immobilisation was potentially detrimental and with growing support in the available literature for early mobilisation, we felt that further recruitment into the trial could not be justified. Therefore, the post-hoc analysis showed that the study was underpowered at 31%. Although undesirable, it is not unprecedented for a trial to be stopped prematurely when clinical equipoise has been lost.
Six patients (21.4%) failed to attend their first post-operative clinic appointment and were lost to long term follow-up. The highest rate of loss to follow up occurred in young male patients, in whom a significant proportion in our geographical area works in the energy sector [10-13]. This population is globally mobile and finds it difficult for economic reasons to find time to attend follow up clinics. Two patients failed to attend their 1 year follow up and another four failed to attend the 2 year follow up. Attempts to contact by telephone were not successful.
A randomised control trial looking at 62 patients with Bankart lesion who underwent arthroscopic repair and they were followed up for a mean 31 months. Patients were either immobilised for 3 weeks or started on an accelerated rehabilitation program starting their exercises on day 1 postoperatively. Pain was reported to be significantly better at six weeks in the early mobilisation group. There was no significant difference in the recurrence rates or shoulder function scores in both groups. The authors found that early mobilisation with some initial limitation of range of movements enhanced healing and allowed early return to activities. Our study is the only other randomised trial of this kind, looking at accelerated rehabilitation.
Outcomes of 34 professional foot ballers who were rehabilitated using an accelerated programme following arthroscopic stabilisation surgery. The players returned to sport at about 11 weeks and there was a 9% recurrence rate. In a case series, the patients were mobilised on day 1. Their recurrence rate was 5.8% and good functional scores were reported [14]. The main focus of this study was of early surgery. In this study, the footballers received more supervised physiotherapy sessions. In the National Health Service, physiotherapy sessions are more limited.
Our study and published cohort and case studies have shown that prolonged immobilisation does not reduce the risk of recurrent instability when compared with early mobilisation. Immobilisation can also result in stiffness and muscle wasting that could result in loss of the secondary stabilising role of the rotator cuff muscles, causing increased morbidity. It also delays initiation of proprioception exercises. In our study, one patient required an arthroscopic capsular release at six months for severe post-operative capsulitis.
Limitations
The strength of our study include that it was a prospective randomised clinical trial with strict inclusion and exclusion criteria. The weakness is the small number of participants and subsequently reduced statistical power. We did not feel that further recruitment was justified as previously discussed. There were also a large number of patients who were lost to follow- up. However, these patients have not re-presented to our unit to date, with ongoing shoulder instability, although clearly some may have presented to other clinical units with recurrent instability.
Patients in the SI group were advised to keep their shoulder in a sling for the first 3 weeks. It is prudent to assume that not all of the patients had complied strictly with these instructions and it was not possible to control for this. Early mobilisation will tend to improve compliance as most these patients are keen to get back to their usual activities as soon as possible.
Conclusion
Evidence from our randomised clinical trial has shown that there is no advantage in prolonged sling immobilisation after arthroscopic shoulder stabilisation surgery. Early mobilisation within an initial limited range of movement does not have any detrimental effect upon failure rates.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
There are no conflicts of interest.
References
- Hobby J, Griffin D, Dunbar M, et al. Is arthroscopic surgery for stabilisation of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. J Bone Joint Surg Br. 2007;89(9):1188-96.
- Godin J, Sekiya JK. Systematic review of arthroscopic versus open repair for recurrent anterior shoulder dislocations. Sports Health. 2011;3(4):396-404.
- Kim SH, Ha KI, Jung MW, et al. Accelerated rehabilitation after arthroscopic Bankart repair for selected cases: a prospective randomized clinical study. Arthroscopy. 2003;19(7):722-31.
- Gibson J, Kerss J, Morgan C, et al. Accelerated rehabilitation after arthroscopic Bankart repair in professional footballers. Shoulder & Elbow. 2016;8(4):279-86.
- Law BK, Yung PS, Ho EP, et al. The surgical outcome of immediate arthroscopic Bankart repair for first time anterior shoulder dislocation in young active patients. Knee Surg Sports Traumatol Arthrosc. 2008;16:188-93.
- Gaunt BW, Shaffer MA, Sauers EL, et al. The American Society of Shoulder and Elbow Therapists' consensus rehabilitation guideline for arthroscopic anterior capsulolabral repair of the shoulder. J Orthop Sports Phys Ther. 2010;40(3):155-68.
- Dawson J, Fitzpatrick R, Carr A. The assessment of shoulder instability: the development and validation of a questionnaire. J Bone Joint Surg Br. 1999;81(3):420-6.
- Ma R, Brimmo OA, Li X, et al. Current concepts in rehabilitation for traumatic anterior shoulder instability. Curr Rev Musculoskelet Med. 2017;10:499-506.
- DeFroda SF, Mehta N, Owens BD. Physical therapy protocols for arthroscopic Bankart repair. Sports Health. 2018;10(3):250-8.
- Duckworth AD, Clement ND, McEachan JE, et al. Prospective randomised trial of non-operative versus operative management of olecranon fractures in the elderly. Bone Joint J. 2017;99(7):964-72.
- Kirkley A, Griffin S, Richards C, et al. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder. Arthroscopy1999;15(5):507-14.
- Mazzocca AD, Brown FM, Carreira DS, et al. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am J Sports Med. 2005;33(1):52-60.
- Kirkley A, Griffin S, Richards C, et al. Prospective randomized clinical trial comparing the effectiveness of immediate arthroscopic stabilization versus immobilization and rehabilitation in first traumatic anterior dislocations of the shoulder. Arthroscopic. 1999;15(5):507-14.
- Robinson CM, Jenkins PJ, White TO, et al. Primary arthroscopic stabilization for a first-time anterior dislocation of the shoulder: a randomized, double-blind trial. JBJS. 2008;90(4):708-21.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
 -EM
-EM  -SI.
-SI.