Research Article - Journal of Clinical Pathology and Laboratory Medicine (2022) Volume 4, Issue 4
Are physicians suspicious enough? Assessing knowledge level in diagnosing multiple myeloma in Nigeria.
Olanrewaju Osho P1, Osho E2, Maltida O1, Okunnuga N3, Alabi B1, Oni O1*
1Department of Hematology and Virology, University of medical sciences, Ondo state, Nigeria.
2Department of Radiology, University of medical sciences, Ondo state, Nigeria
3Department of Oncology, University of medical sciences, Ondo state, Nigeria
- Corresponding Author:
- Olanrewaju Osho
Department of Hematology and Virology
University of Medical Sciences
Ondo State, Nigeria
Tel No: +2348034970314
Email : droshopo@ unimed.edu.ng
Received: 28-May-2022, Manuscript No. AACCR -22-65213; Editor assigned: 31-May-2022, PreQC No. AACCR -22-65213(PQ); Reviewed: 14-Jun-2022, QC No. AACCR -22- 65213; Revised: 17-Jul-2022, Manuscript No. AACCR-22-65213(R); Published: 24-Jul-2022, DOI:10.35841/aacplm-4.4.116
Citation: Osho P, Osho E, Maltida O, et al. Are physicians suspicious enough? Assessing knowledge level in diagnosing multiple myeloma in Nigeria. J Clin Path Lab Med. 2022;4(4):116
Abstract
Multiple myeloma (Kahler’s disease) is a hematological disorder resulting from proliferation of plasma cells in the bone marrow characterized by hypercalcaemia, bone lesion, renal impairment, and anaemia which causes a monoclonal protein-secreting disorder called paraproteinemias. Globally, it is commoner in blacks than in Caucasians and Asians although Africans show a lower incidence rate. It is a disease of the elderly with a median age incidence of 65 years in Western countries and 58 years in Nigeria. The male to female ratio is 2-3:1. Objectives: This study was carried out to assess the extent of knowledge of physicians with regards to multiple myeloma. Our research also explored the state of multiple myeloma diagnosis across health care facilities in Ondo State, outlining the challenges resulting from lack of knowledge and proposing possible solutions. Methodology: The research was conducted among physicians working across Ondo State. This was a specific and direct study of physicians and specialists working at the health facilities using a semi- structured questionnaire. SPSS version 23 was used for statistical analysis and chi square was used to check the significant association in the study with p-value <0.05 being significant. Results: A total of 205 doctors were involved. There was a general poor knowledge of the disorder although the specialists had a better understanding. Bone pain and anemia are the major clinical features seen in their patients with multiple myeloma. Significant association exists between area of specialty, years of experience and knowledge of physicians in the studied population. Conclusion: There’s poor knowledge which was influenced by years of experience, area of specialty and lack of retraining programmers among other factors. To aid early referral, we recommend that physicians have a high index of suspicion. In patients with multiple myeloma, newer treatment options should be considered.
Keywords
Myeloma, Suspicion, Physicians, Knowledge Assessment.
Introduction
Multiple Myeloma (MM) is a chronic haematological disorder of varying severity which affects terminal differentiated B lymphocytes characterized by proliferation and accumulation of clonal immunoglobulin producing neoplastic plasma cells in the bone marrow leading to hyperkalemia, bone lesion, renal impairment and anaemia; a condition known as paraproteinemia [1]. MM is a spectrum of diseases which evolves from Monoclonal Gammopathy of Unknown Significance (MGUS) to smouldering multiple myeloma and advances to symptomatic stage of MM [2].
Globally, MM constitutes about 2% of all cancers and also accounts for 13.4% of all lymphohematopoietic cancers, 19% mortality cases related to hematological malignancies, and 2% of all cancer-related mortality. Studies in Nigeria show that MM accounts for 8.2% all of hematological malignancies with a median age of 58 years as compared to 65 years in the Western world [3,4]. Higher incidence is seen in black Americans as compared to their counterparts in Africa. A high prevalence rate is also seen in African population with an incidence rate of 12.7% (21 million people) of total population of Nigeria while the male to female ratio in Nigeria is 2-3:1[5].
The exact cause of MM is unknown. However, like all cancers, the disorder develops when genetic mutations cause particular cells to grow uncontrollably [6]. Specific proteins such as KRAS, BRAF, NRAS and TP53 have been implicated in many cases of MM. Other implicated factors include: exposure to ionizing radiations, exposure to chemicals of benzene derivatives, genetic predispositions (associated with with HLA-Cw5 or HLA-Cw2), chromosomal translocations involving the immunoglobulin’s heavy chain locus on chromosome 14 in 20-40%; and monosomy [7].
At the cellular level, there’s secretion of osteoclast-activating factors such as interleukin IL-6, (IL)-1B and TNF-B that are responsible for the myeloma related end organ damage and tissue impairment. These are induced by adhesion of myeloma cells to bone marrow. Also, the microenvironment created by the cytokines is known to enhance angiogenesis, which allow malignant plasma cells to thrive [8].
Common features in MM are: Bone Pain, Anemia, Fatigue, Fracture, Vertebrae Collapse, Spinal cord compression, recurrent infections and Renal and Neurological complications. The disease can progress to end organ damage. These are all characteristics of CRAB showing hyperkalemia, renal impairment, anemia, bone lesion, bone pain, bleeding.
Diagnosis of MM is often done using full blood count, Erythrocyte Sedimentation Rate, peripheral blood film, bone marrow aspirate, electrolyte, serum chemistry, urea and creatinine. Total protein albumin and globulin, serum protein electrophoresia and complication, Bence Jone Protein and free light chains electrophoretic test. B2 micro globulins level and skeletal x ray of the bones and MRI [9].
MM outcomes have improved drastically over the last decades as a result of novel therapies, several of which are now commonly continued to disease relapse. Autologous stem cell transplantation has been included in management of MM as it gives a form of Pseudocure and often, the myeloma relapses after a few years. However, in SubSaharan regions including Nigeria, funding has been a huge hindrance to purchase these therapies which resulted in the heavy reliance on the old therapies. In this mini review, we explored the state of MM diagnosis across our state and near, outlining the challenges to diagnosis and proposing possible solutions.
Materials & Methods
Study design
The study employed a quantitative research method in order to access the knowledge of MM among physicians across Ondo State in the study location. Besides, we employed a quantitative research method in order to be able to have a broader view of the knowledge of MM and make inference from the study location.
Study area
The study was conducted at health care facilities across Ondo State, SouthWestern Nigeria which included: General Hospital, Comprehensive Hospital, Health Centre, Private Hospitals and Teaching Hospital all across Ondo State Table 1.
| Variable | Frequency | Percentage (%) |
|---|---|---|
| Designation | ||
| Medical Officer cadre | 106 | 51.7 |
| Senior Registrar | 42 | 20.5 |
| Junior Registrar | 16 | 7.8 |
| House Officers | 8 | 3.7 |
| Consultants | 33 | 16.3 |
| Total | 205 | 100 |
| Officer Cadre | ||
| Chief Medical Officer | 1 | 0.9 |
| Principal Medical Officer | 2 | 1.9 |
| Senior medical officers | 38 | 35.8 |
| Medical officer | 65 | 61.3 |
| Total | 106 | 100 |
| Years of Experience | ||
| <2 years | 61 | 29.8 |
| 2 – 5 years | 65 | 31.7 |
| 6 – 10 years | 58 | 28.3 |
| >10 years | 21 | 10.2 |
| Total | 205 | 100 |
| Institution where you Practice | ||
| Teaching Hospital | 85 | 41.5 |
| Specialist Hospital | 45 | 22 |
| Federal Medical center | 20 | 9.8 |
| General Hospital | 12 | 5.9 |
| Comprehensive Health Centre | 8 | 3.9 |
| Health Centre | 4 | 2 |
| Private Hospital | 31 | 15.1 |
| Total | 205 | 100 |
Table 1. Socio-Demographic Characteristics.
The structured questionnaire was developed which was divided into the following parts:
1. Socio demographic information of the respondents.
2. General knowledge of Clinical features of Multiple myeloma.
Study population
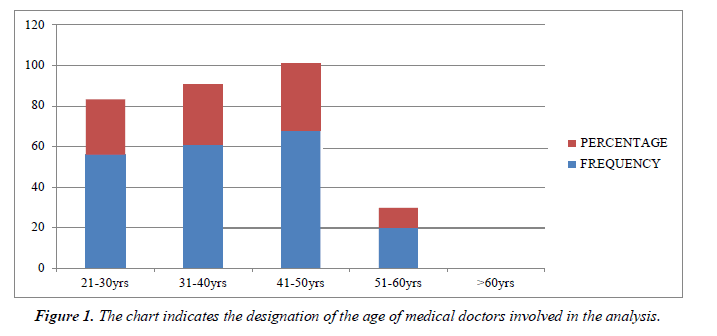
The study consists of all physicians of all cadres who participated in the survey voluntarily. A total of 205 physicians were involved in the research. Majority of the physicians in our study are within the age range of 21-60 years Figure 1.
Sampling method
The sample size for this study was derived from the Krejcie and Morgan. The sample sizes are at 0.95 percent level of confidence. A total sample of 205 was arrived at using the Table 2.
| Features | Frequency | Percentage |
|---|---|---|
| Backache | ||
| Yes | 199 | 97.1 |
| No | 5 | 2.4 |
| Don’t know | 1 | 0.5 |
| Total | 205 | 100 |
| Renal Failure | ||
| Yes | 189 | 92.2 |
| No | 6 | 2.9 |
| Don’t Know | 10 | 4.9 |
| Total | 205 | 100 |
| Anaemia | ||
| Yes | 173 | 84.4 |
| No | 5 | 2.4 |
| Don’t Know | 27 | 13.2 |
| Total | 205 | 100 |
| Hypercalcemia | ||
| Yes | 143 | 69.8 |
| No | 13 | 6.3 |
| Don’t know | 49 | 23.9 |
| Total | 205 | 100 |
| Pathologic Fracture | ||
| Yes | 142 | 69.3 |
| No | 5 | 2.4 |
| Don’t Know | 58 | 28.3 |
| Total | 205 | 100 |
| Inability to walk | ||
| Yes | 132 | 64.4 |
| No | 5 | 2.4 |
| Don’t Know | 68 | 33.2 |
| Total | 205 | 100 |
Table 2. Assessment of knowledge of clinical features of MM Clinical Features.
Data analysis
SPSS version 23 was used for statistical analysis and chi square was used to check the significant association in the study with p value <0.05 being significant
Ethical consideration
Ethical consideration is gotten from the Ministry of Health, Ondo State.
Discussion
This research also draws out the hierarchy importance of the physicians in relation to their knowledge extent.
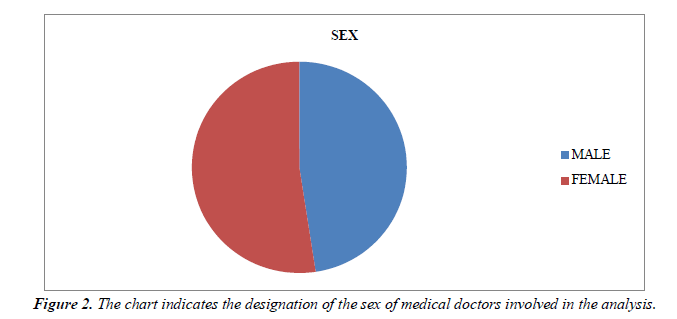
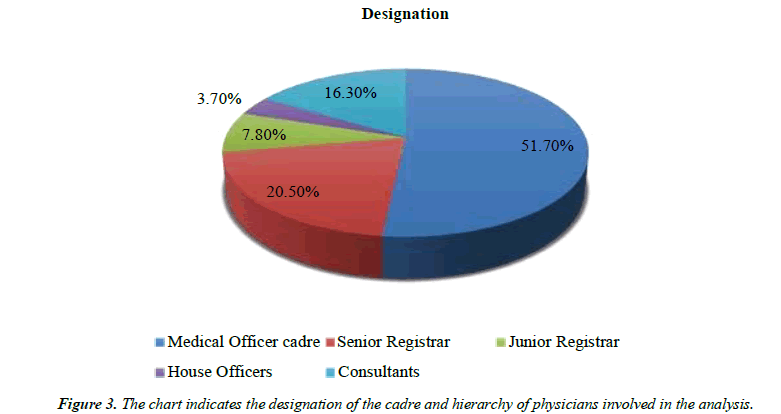
Majority of the physicians in our study are within the age range of 21-60 years. This slightly differs in correlation with study done [10,11] with the median age of 50 years. 52% of the physicians in our study are females; however this is not in accordance with study in Nigeria with majority of physicians in the study being male. Medical Officers had the highest number of physicians used in this study with most of them practicing in health facilities across the state with 2-5 years of working experience; this is also similar to a study [12]. It was also noticed that majority out of the 164 medical officers had a poor knowledge (57.32%) while 42.68% represented the percentage of them that had good knowledge of MM [13]. Among the Specialists which involved the consultants and residents, it was noticed there was a shift of knowledge as well. The consultants had a good knowledge of MM which varies with the departments they fell into Table 3. The residents also showed an appreciable knowledge of the disease. Backache has been seen to be one of the major features of MM seen among the physicians in our study. This is in correlation with study done by [14]. Patients with MM are also diagnosed with renal failure as seen in study done by. Common presenting signs seen among MM patients are anemia and bone pain. This presentation is important in resource-constrained contexts when clinical judgments are relied upon rather than diagnostic equipment Figure 2.
| Methods | Frequency | Percentage |
|---|---|---|
| Bone Marrow Biopsy/ Aspiration | ||
| Yes | 128 | 62.4 |
| No | 2 | 1.0 |
| Don’t Know | 75 | 36.6 |
| Total | 205 | 100 |
| Protein Electrophoresis | ||
| Yes | 140 | 68.3 |
| No | 3 | 1.5 |
| Don’t Know | 62 | 30.2 |
| Total | 205 | 100 |
| Elevated ESR | ||
| Yes | 147 | 71.7 |
| No | 7 | 3.4 |
| Don’t Know | 51 | 24.9 |
| Total | 205 | 100 |
| Roleaux Formation | ||
| Yes | 118 | 57.6 |
| No | 20 | 9.8 |
| Don’t Know | 67 | 32.7 |
| Total | 205 | 100 |
| Doppler Ultrasound | ||
| Yes | 150 | 73.2 |
| No | 7 | 3.4 |
| Don’t know | 48 | 23.4 |
| Total | 205 | 100 |
| Total Protein & Albumin | ||
| Yes | 142 | 69.3 |
| No | 3 | 1.5 |
| Don’t Know | 60 | 29.3 |
Table 3. Knowledge of method of Assessment of MM.
The most common diagnostic methods seen in our study include Bone marrow aspiration, Protein electrophoresis, Doppler Ultrasound, Elevated ESR, Total protein and albumin. This is in correlation with study done. It can be seen in our study that majority of the physicians had a poor knowledge on MM where it was noticed that the 65% of medical officer’s cadre were the most affected with little knowledge of the disease. This is in accordance with study. The poor knowledge of MM among physicians in our study had led misdiagnosis of patients with MM hence could pose a serious threat to the health condition of the people Table 4. Factors responsible for the poor knowledge of physicians on MM are few years of experience and lack of medical equipment due to poor resource state of the country [15].
| Knowledge | Frequency | Percentage |
|---|---|---|
| MM is an infectious disease | ||
| Yes | 129 | 62.9 |
| No | 11 | 5.4 |
| Don’t Know | 65 | 31.7 |
| Total | 205 | 100 |
| MM is a B Malignant disorder | ||
| Yes | 139 | 67.8 |
| No | 8 | 3.9 |
| Don’t know | 58 | 28.3 |
| Total | 205 | 100 |
| MM can be triggered by HIV | ||
| Yes | 89 | 43.4 |
| No | 59 | 28.8 |
| Don’t Know | 57 | 27.8 |
| Total | 205 | 100 |
| MM can appear as loss of Tumor | ||
| Yes | 119 | 58.0 |
| No | 12 | 5.9 |
| Don’t Know | 74 | 36.1 |
| Total | 205 | 100 |
| CRAB is not a supportive diagnostic | ||
| Yes | 127 | 62.0 |
| No | 20 | 9.8 |
| Don’t Know | 58 | 28.3 |
| Total | 205 | 100 |
| Bence Jones Proteinemia & Paraproteinema | ||
| Yes | 132 | 64.4 |
| No | 9 | 4.4 |
| Don’t Know | 64 | 31.2 |
| Total | 205 | 100 |
| 60% or more plasma can suggest MM | ||
| Yes | 136 | 66.3 |
| No | 4 | 2.0 |
| Don’t Know | 65 | 31.7 |
| Total | 205 | 100 |
| MM is a T – cell Malignant disorder | ||
| Yes | 87 | 42.4 |
| No | 35 | 17.1 |
| Don’t know | 83 | 40.5 |
| Total | 205 | 100 |
| Paget Disease and Osteitis Fibrosis Cystica | ||
| Yes | 115 | 56.1 |
| No | 6 | 2.9 |
| Don’t Know | 84 | 41.0 |
| Total | 205 | 100 |
| MM involves multidisciplinary Management | ||
| Yes | 129 | 62.9 |
| No | 1 | 0.5 |
| Don’t Know | 75 | 36.6 |
| Total | 205 | 100 |
| Referral Pattern of Patients with Multiple Myeloma in your centre | ||
| Interdepartmental | ||
| Yes | 80 | 39.0 |
| No | 12 | 5.9 |
| Don’t Know | 113 | 55.1 |
| Total | 205 | 100 |
| Other teaching hospital | ||
| Yes | 45 | 22.0 |
| No | 7 | 3.4 |
| Don’t Know | 153 | 74.6 |
| Total | 205 | 100 |
| Federal Medical Centre | ||
| Yes | 38 | 18.5 |
| No | 13 | 6.3 |
| Don’t Know | 154 | 75.1 |
| Total | 205 | 100 |
| State Specialist | ||
| Yes | 61 | 29.8 |
| No | 9 | 4.4 |
| Don’t Know | 135 | 65.9 |
| Total | 205 | 100 |
| Steroid based Chemotherapy used for treatment | ||
| Yes | 140 | 68.3 |
| No | 2 | 1.0 |
| Don’t know | 63 | 30.7 |
| Total | 205 | 100 |
| Patients with MM benefit from anticoagulant | ||
| Yes | 159 | 77.6 |
| No | 0 | 0 |
| Don’t know | 46 | 22.4 |
| Total | 205 | 100 |
| Analgesics are part of treatment regimen | ||
| Yes | 162 | 79.0 |
| No | 0 | 0 |
| Don’t Know | 43 | 21.0 |
| Total | 205 | 100 |
| Biophosphate drugs are invaluable in Management | ||
| Yes | 161 | 78.5 |
| No | 2 | 1.0 |
| Don’t Know | 42 | 20.5 |
| Total | 205 | 100 |
| Bortezomib is an important Chemotherapy Regimen | ||
| Yes | 172 | 83.9 |
| No | 0 | 0 |
| Don’t Know | 33 | 16.1 |
| Total | 205 | 100 |
| Phalidomide, Lenalidomide Cyclophomide used in treatment | ||
| Yes | 178 | 86.8 |
| No | 0 | 0 |
| Don’t Know | 27 | 13.2 |
| Total | 205 | 100 |
| Bone Marrow Transplantation can lead to cure | ||
| Yes | 173 | 84.4 |
| No | 0 | 0 |
| Don’t Know | 32 | 15.6 |
| Total | 205 | 100 |
Table 4. Knowledge based Assessment of different diseases.
A positive correlation occurs between the type of institution of practice and the level of knowledge in our study Figure 3. In most specialist and tertiary hospital, availability of good medical facilities with skilled personnel contributes to the good knowledge of the physicians on MM whereas in remote general hospital, comprehensive health center and primary health care have lack of skilled man power and physicians with less knowledge of multiple myeloma which is responsible for misdiagnosis of patients with MM. Our study also shows statistical association between socio-demographic variables of physicians and their knowledge on MM. It can be inferred from our study that significant association was seen between the level of knowledge of physicians and educational qualification with a p value <0.001. Rank of the physicians was also seen to have a significant association with sociodemographic variables. Years of experience plays a significant role in the treatment and diagnosis of patients with MM as seen in our study showing a significant association with the demographic variables Table 5. This is in correlation with study [16].
| Variable | Knowledge | Df | Chi – Square | P – value | |
|---|---|---|---|---|---|
| Good | Poor | ||||
| Age | 6 | 5.047a | 0.538 | ||
| 21 – 30 | 24 | 32 | |||
| 31 – 40 | 21 | 40 | |||
| 41 – 50 | 25 | 43 | |||
| 51 – 60 | 7 | 13 | |||
| Total | 77 | 128 | |||
| Sex | 2 | 2.625a | 0.269 | ||
| Male | 42 | 55 | |||
| Female | 35 | 73 | |||
| Total | 77 | 128 | |||
| Designation | |||||
| Consultants | 26 | 7 | 10 | 34.309a | 0.000 |
| Medical Officer cadre | 31 | 75 | |||
| Senior Registrar | 9 | 33 | |||
| Junior Registrar | 4 | 4 | |||
| House Officers | 7 | 9 | |||
| Total | 77 | 128 | |||
| Medical Officer Cadre | 6 | 14.198a | 0.027 | ||
| Chief Medical Officer | 1 | 0 | |||
| Principal Medical Officers | 1 | 1 | |||
| Senior Medical officers | 5 | 33 | |||
| Medical Officers | 70 | 94 | |||
| Total | 77 | 128 | |||
| Years of Experience | 6 | 8.130a | 0.229 | ||
| < 2 years | 25 | 36 | |||
| 2 – 5 years | 21 | 44 | |||
| 6 – 10 years | 20 | 38 | |||
| >10 years | 11 | 10 | |||
| Total | 77 | 128 | |||
| Health Facilities General Hospital |
3 | 9 | |||
| Comprehensive Hospital | 3 | 5 | |||
| Health Centre | 2 | 2 | |||
| Private Hospital | 10 | 21 | |||
| Total | 77 | 128 | |||
Table 5. Knowledge based Assessment of Variables.
Moreover, there are few medical officer cadre in particular CMO, PMO with more than 10 years of experience in our study tend to have good knowledge on MM. Also, years of experience also plays a major role in the knowledge of physicians on MM as seen in our study that majority of the physicians had less than 2 years of experience in particular HO and JMO which contributes to the poor knowledge of the physicians due to their training and exposure to MM compared to those with more than 10 years’ experiences have seen a lot of cases of MM patients.
No significant association had been seen with age and sex in correlation with knowledge of physicians on MM. This correlates the findings of [17].
Conclusion
The study confirms that there is a poor knowledge of MM among physicians. To aid early referral, we recommend that physicians have a high index of suspicion in patients with bone pain and anemia. Newer treatment techniques such as stem cell transplantation should be used. Bone pain and anemia especially in the elderly patients are critical clinical indicators that should prompt a physician in a resource-limited situation to investigate cases of MM. Seminars and presentations should be carried out frequently to re-educate and retrain the younger physicians on MM. Government should invest in the health insurance coverage for cancer patients. Creative approaches such as online training, research and capacity building should be explored for MM and other cancer related diseases.
References
- Alexander DD, Mink PJ, Adami HO, et al. Multiple myeloma: a review of the epidemiologic literature. Int J Cancer. 2007;120(S12):40-61.
- Fowler JA, Edwards CM, Croucher PI. Tumor–host cell interactions in the bone disease of myeloma. Bone. 2011;48(1):121-8.
- Mahindra A, Hideshima T, Anderson KC. Multiple myeloma: biology of the disease. Blood reviews. 2010;24:S5-11.
- Landgren O, Kyle RA, Pfeiffer RM, et al. Monoclonal gammopathy of undetermined significance (MGUS) consistently precedes multiple myeloma: a prospective study. Blood, Am J Hematol. 2009;113(22):5412-7.
- Durosinmi MA. A design Handbook of Haemato-oncology Chemotherapy for Medical Students and Doctors.
- Cohen HJ, Crawford J, Rao MK, et al. Racial differences in the prevalence of monoclonal gammopathy in a community-based sample of the elderly. Am J Med. 1998;104(5):439-44.
- Heider M, Nickel K, Hogner M, et al. Multiple myeloma: molecular pathogenesis and disease evolution. Oncol Res Treat. 2021;44(12):672-81.
- Talamo G, Farooq U, Zangari M, et al. Beyond the CRAB symptoms: a study of presenting clinical manifestations of multiple myeloma. Clin Lymphoma Myeloma Leuk. 2010;10(6):464-8.
- Devarakonda S, Efebera Y, Sharma N. Role of stem cell transplantation in multiple myeloma. Cancers. 13(4), 863.
- Madu AJ, Ocheni S, Nwagha TA, et al. Multiple myeloma in Nigeria: an insight to the clinical, laboratory features, and outcomes. Niger J Clin Pract. 2014;17(2):212-7.
- Fasola FA, Eteng KI, Shokunbi WA, et al. Renal status of multiple myeloma patients in Ibadan, Nigeria. Ann Ib Postgrad Med. 2012;10(2):28-33.
- Odunukwe NN, Madu JA, Nnodu OE, et al. Multiple myeloma in Nigeria: a multi-centre epidemiological and biomedical study. Pan Afr Med J. 2015;22(1).
- Ricciardi MR, Calabrese E, Milella M, et al. Preclinical Approach to Sensitize Multiple Myeloma Cells: Combination of the MEK Inhibitor PD0325901 with ABT-737 or Mevinolin. Blood. 2009;114(22):1842.
- Salawu L, Durosinmi MA. Myelomatosis: Clinical and laboratory features in Nigerians. West Afr J Med. 2005;24(1):54-7.
- Talamo G, Farooq U, Zangari M, et al. Beyond the CRAB symptoms: a study of presenting clinical manifestations of multiple myeloma. Clin Lymphoma Myeloma Leuk. 2010;10(6):464-8.
- Osborne TR, Ramsenthaler C, de Wolf-Linder S, et al. Understanding what matters most to people with multiple myeloma: a qualitative study of views on quality of life. Bmc Cancer. 2014;14(1):1-4.
- Krejcie RV, Morgan DW. Determining sample size for research activities. Educ Psychol Meas. 1970;30(3):607-10.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref