Research Article - Current Trends in Cardiology (2021) Volume 5, Issue 4
Acute coronary syndrome in non-diabetic young: Risk factors and coronary artery disease pattern
Abdulaziz Aboshahba1*, Raphael C Solomon2, Kamal S Mansour3, Mohammed M Aldiamony3, Marwa M Gad3, Khaled Eid3
1Department of Cardiology, AL-Azhar University, Cairo, Egypt
2Department of Cardiology, Prince Abdullah Bin Musaed Cardiac Centre (PAMCC), Arar, Saudi Arabia
3Department of Cardiology, Zagazig University, Zagazig, Egypt
- Corresponding Author:
- Abdulaziz aboshahba
Department of Cardiology
Al-Azhar University
Cairo
Egypt
E-mail: abdelazeez_aboshahba@yahoo.com
Accepted date: 11 June, 2021
Citation: Aboshahba A, Solomon RC, Mansour KS, et al. Acute coronary syndrome in non-diabetic young: Risk factors and coronary artery disease pattern. Curr Trend Cardiol. 2021;5(4):49-54.
Abstract
It is of great significance to identify young individuals who are at risk for CAD; as such patients may need more aggressive secondary prevention. However, predicting risks in young ACS patients is challenging, and how to identify young ACS patients as high risk for recurrent CAD is still unclear.
Keywords
Computer-Aided Design (CAD), Direct Message (DM), Young, ST-elevation Myocardial Infarction (STEMI).
Introduction
The burden of CAD is increasing, and is gradually becoming a major public health problem. With changes in lifestyle, dietary habits, and social stress, the onset age of CAD has decreased. Although compared with elderly patients, the prognosis for young patients with CAD may be relatively good. Risk factors and prognosis for premature ACS are still debilitating. According to the VIRGO study, almost 98% of young patients (18-55 years) with acute myocardial infarction have one or more risk factors for CAD and 64% have three or more risk factors; only about half (53%) of patients knew that they had CAD risks, and even fewer were informed about the risk factors for CAD before the onset of the disease. Besides, some studies have shown that young patients with ACS had a higher plaque burden than older patients. Since the pathophysiology of atherosclerosis in young ACS patients is different from older patients by the presence of genetic abnormalities, lipids metabolism, and coronary artery anomalies, the risk factors profile in young ACS patients need to be addressed [1-6].
Aim of the study
The aim of this studyis the correlation between the risk factors and clinical picture and coronary angiographic pattern in non-diabetic patients younger than forty years.
Patients and Methods
Study population
The present study is a prospective, cross sectional study carried out between October 2016 to April 2020 included one hundred patients with coronary artery disease aged<40 years old and two hundred patients with CAD ≥ 40 years old who underwent coronary angiography at the National Heart Institute (NHI) and cardiology department of Zagazig hospital university. The protocol approved by ethical committee.
Patient selection
This study was conducted to evaluate clinical condition, risk factors and angiographic characteristics among patients with premature CAD and compared them with older patients.
All patients with age more than 18 years and had their first angiogram done with a positive findings of coronary artery disease were included in this study.
All had significant coronary artery disease defined as ≥ 50% lumen diameter reduction of at least one major epicardial artery, coronary angiography was the first ever performed for each patient [1].
All patients with concomitant valvular heart disease, dilated cardiomyopathy, hypertrophic cardiomyopathy, previous coronary intervention, coronary artery bypass graft and chronic renal or liver disease were excluded from this study.
The patients were classified into two groups: Group 1 comprised 98 patients with non-diabetic CAD aged<40 years Old, while group 2 comprised 102 patients with non-diabetic CAD aged ≥ 40 years old.
Methods
All patients were subjected to the following:
I. Full history taking including age, gender, risk factors as diabetes mellitus, hypertension, smoking, dyslipidemia and family history of premature coronary artery disease.
II. Thorough physical and clinical examination.
III. 12 Lead ECG.
IV. Echo ― EF ―
V. Coronary angiography.
This study included 198 patients who underwent angiogram at cardiology department of National Heart Institute and cardiology department at Zagazig University Hospital [7-9]. Coronary angiography considered abnormal when there is diameter stenosis (occlusion) that occurs to one or more of the three major coronary arteries during the angiogram procedure [10]. Significant occlusion defined as equal or more than 50% narrowing in left main branch and equal or more than 70% of other epicardia [11].
Angiograms were visually assessed by two independent observers blinded to the identity and clinical characteristics of the patients. Theangiographic view at end-diastole, in which the lesion appeared most severe, was selected. The severity of stenosis was defined as the maximum percentage narrowing calculated from the minimum diameter (absolute measurement in millimeters) of the involved segment andthediameter ofan adjacentnormal coronary segment.
Angiographic features will be evaluated regarding:
I. Artery affected: left main, left anterior descending artery, left circumflex artery and right coronary artery.
II. Site of the lesion: Bifurcation lesion or involve the main trunk only.
III. Lesion location: Smooth "type A" (discrete<10 mm length, concentric, less than totally occlusive and smooth contour and absence of thrombus).complex “type B and C"(tubular or diffuse>10 mm length, eccentric, angulated, moderate to heavy calcification).
IV. Collateral circulation: grade 0: no visible collaterals, grade 1: the filling of the side branch via collateral vessels without a visible epicardial coronary artery, grade 2: the incomplete filling of the epicardial coronary artery, and grade 3: the complete filling of the epicardial coronary artery.
V. TIMI flow: grade 3: complete reperfusion, grade 2: partial reperfusion, grade 1: penetration with minimal perfusion and grade 0: no perfusion.
VI. Myocardial blush is a strongangiographic predictor of mortality in patients with TI
MI 3 flow after primary angioplasty and graded into grade 0: no myocardial blush, grade 1: minimal myocardial blush, grade 2: moderate myocardial blush and grade 3: normal myocardial blush [9].
VII. Multivessel disease included two vessel diseases vs. single vessel disease. The Syntax score algorithm was calculated according to the Dominance of the artery, number of lesions, segments involved per lesion, lesion characteristics, bifurcation or trifurcating lesions, and presence of total occlusion:
Data management
Data were collected, verified, revised then edited on personal computer. Categorical variables were expressed as their absolute and relative frequencies (percentage) while continuous variables werepresented as mean values± standard deviation.
Comparison was made between the 2 groups using the t-test for continuous variables and the Chi-square and Pearson correlation coefficient for categorical variables.
Statistical analysis
Data were analyzed using Statistical Program for Social Science (SPSS) version 25.0 for windows (SPSS Inc., Chicago, IL, USA) and NCSS 12.0 for windows(NCSS LCC., Kaysville, UT, USA).
Quantitative data of normal distribution were expressed as mean ± standard deviation (SD). Qualitative data were expressed as frequency and percentage.
The following tests were done:
• Independent-samples t-test of significance was used when comparing between two means of normally distributed data.
• Chi-square (χ2) test also called Pearson's chi-square test or the chi-square test of association is used to discover if there is a relationship between two categorical variables.
• Fisher Exact test is a test of significance that isused in the place of chi squaretest in 2 by 2 tables, especially in cases of small samples.
• The "Linear-by-Linear" test is for ordinal (ordered) categories and assumes equal and ordered intervals. The Linear-by-Linear Association test is a test for trends in a larger than 2 × 2 table.
• Multivariate regression analysis is used when we want to predict the value of a variable based on the value of two or more other variables. The variable we want to predict is called the dependent variable (or sometimes, the outcome, target or criterion variable). The variables we are using to predict the value of the dependent variable are called the independent variables (or sometimes, the predictor, explanatory or regress or variables).
Results
This prospective cross sectional study was conducted between October 2014 to October 2020. The study population was divided into two groups included 98(49%) patients with CAD aged ≤ 40 years old and 102 (51%) patients with CAD>40 years old.
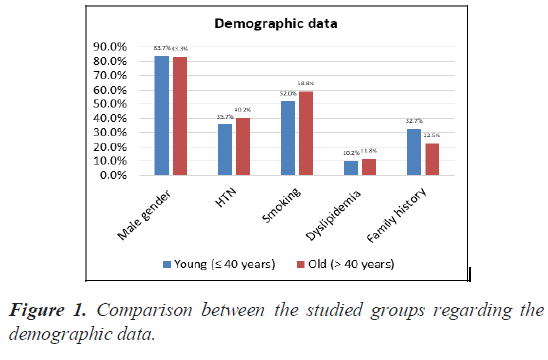
As regard demographic data, statistical analysis showed significant difference between the two groups, male predominance in the studied groups with high prevalence in age ≤ 40 (P value<0.05). Regarding coronary vascular risk factors in different age groups, smoking and positive family history were significantly higher in group I with age ( ≤ 40) than group II with age (>40) (Pvalue<0.05) (Table 1) (Figure 1).
| Demographic data | Young (≤ 40 years) | Old (>40 years) | P-value(Sig.) |
|---|---|---|---|
| Count | 98 | 102 | |
| Risk factors | |||
| Male gender | 82 (83.7%) | 85 (83.3%) | 0.948 (NS) |
| HTN | 35 (35.7%) | 41 (40.2%) | 0.514 (NS) |
| Smoking | 51 (52%) | 60 (58.8%) | 0.335 (NS) |
| Dyslipidemia | 10 (10.2%) | 12 (11.8%) | 0.724 (NS) |
| Family history | 32 (32.7%) | 23 (22.5%) | 0.110 (NS) |
Table 1. Descriptive statistics.
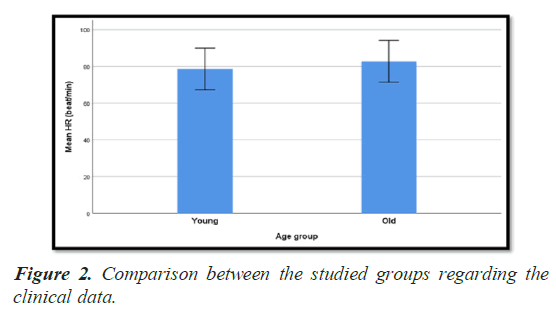
Comparison between the studied groups regarding the clinical data (Table 2) (Figure 2) showed that STEMI diagnosis was more common in group 1, while NSTEMI was more in group II. However this has no statistical significant.
| Clinical data | Young (≤ 40 years) | Old (>40 years) | P-value(Sig.) |
|---|---|---|---|
| Count | 98 | 102 | |
| Diagnosis | |||
| STEMI | 70 (71.4%) | 66 (64.7%) | 0.308 (NS) |
| Non-ST ACS | 28 (28.6%) | 36 (35.3%) | |
| ECG | |||
| Anterior STEMI | 44 (44.9%) | 42 (41.2%) | 0.775 (NS) |
| Non-anterior STEMI | 26 (26.5%) | 24 (23.5%) | |
| ST-T changes | 21 (21.4%) | 26 (25.5%) | |
| No specific changes | 7 (7.1%) | 10 (9.8%) | |
| SBP (mmHg) | |||
| Mean ± SD | 129.6 ± 18.3 | 129.8 ± 22.0 | 0.955 (NS) |
| DBP (mmHg) | |||
| Mean ± SD | 81.9 ± 10.2 | 81.5 ± 9.4 | 0.791 (NS) |
| HR (beat/min) | |||
| Mean ± SD | 78.6 ± 11.3 | 82.8 ± 11.4 | 0.010 (S) |
| Pain to door (hour) | |||
| Mean ± SD | 5.07 ± 1.52 | 5.10 ± 1.27 | 0.853 (NS) |
| Door to balloon (min) | |||
| Mean ± SD | 58.1 ± 22.1 | 55.4 ± 14.0 | 0.315 (NS) |
Table 2. Comparison between the studied groups regarding the clinical data.
None of SBP or DBP or HR was statistically significant between patients of group I and patients of group II. Heart rate was less in group I (78.6 ± 11.3 beatsminutes) as compared with group II (82.8 ± 11.4 beats minutes), and this has statistical significance.
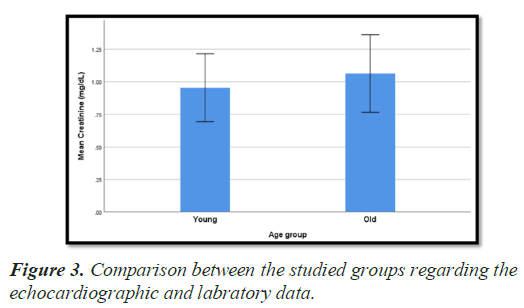
As regard EF%, there was statistically high significant difference in between both age groups regarding EF (P value 0.001) with higher in group II with age>40 years.
Creatinine level was lower in group I than group II. This difference was statistically significant (P value 0.006). On the other hand, there was no statistically significant difference in CK-MB level between both groups (Table 3) (Figures 3 and 4).
| Echocardiographic and laboratory data | Young (≤ 40 years) | Old (>40 years) | P-value(Sig.) |
|---|---|---|---|
| Count | 98 | 102 | |
| EF (%) | |||
| Mean ± SD | 45.9 ± 7.4 | 50.8 ± 8.1 | <0.001 (HS) |
| Creatinine (mg/dL) | |||
| Mean ± SD | 0.96 ± 0.26 | 1.07 ± 0.30 | 0.006 (S) |
| CK-MB (IU/L) | |||
| Mean ± SD | 84.9 ± 24.8 | 93.8 ± 53.1 | 0.131 (NS) |
Table 3. Comparison between the studied groups regarding the echocardiographic and laboratory data.
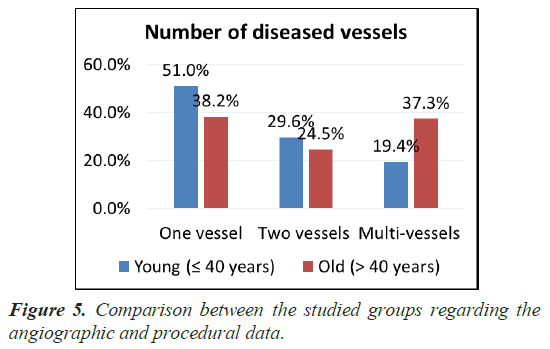
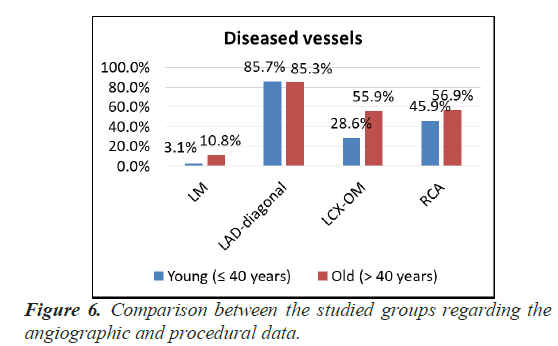
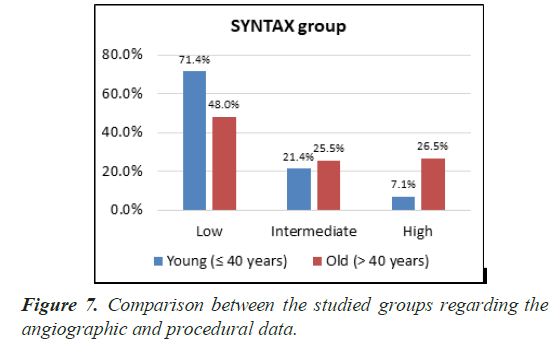
Statistical analysis showed that: One vessel and two vessel disease were the most prominent in group I with age ≤ 40 years versus group II with age>40 years while MVD was most prominent in Group II versus group I with significant P value 0.010. LM and LCX were the most common types of lesion in group II than group I, with significant P value (0.032) and (0.001) respectively, but LAD-diagonal and RCA had no significant difference between two groups (Table 4) (Figures 5-8).
| Coronary angiographic and procedural data | Young (≤ 40 years) | Old (>40 years) | P-value(Sig.) |
|---|---|---|---|
| Count | 98 | 102 | |
| Access | |||
| Femoral | 90 (91.8%) | 92 (90.2%) | 0.685 (NS) |
| Radial | 8 (8.2%) | 10 (9.8%) | |
| Number of diseased vessels | |||
| One vessel | 50 (51%) | 39 (38.2%) | 0.010 (S) |
| Two vessels | 29 (29.6%) | 25 (24.5%) | |
| Multi-vessels | 19 (19.4%) | 38 (37.3%) | |
| Diseased vessels | |||
| LM | 3 (3.1%) | 11 (10.8%) | 0.032 (S) |
| LAD-diagonal | 84 (85.7%) | 87 (85.3%) | 0.933(NS) |
| LCX-OM | 28 (28.6%) | 57 (55.9%) | <0.001 (HS) |
| RCA | 45 (45.9%) | 58 (56.9%) | 0.122 (NS) |
| SYNTAX group | |||
| Low (<22) | 70 (71.4%) | 49 (48%) | <0.001 (HS) |
| Intermediate (22.5-32) | 21 (21.4%) | 26 (25.5%) | |
| High (>32) | 7 (7.1%) | 27 (26.5%) | |
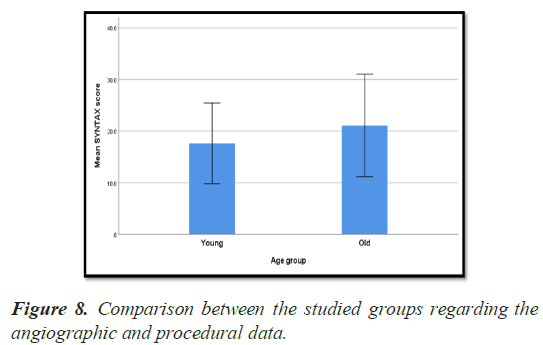
| SYNTAX score | |||
| Mean ± SD | 17.6 ± 7.8 | 21.1 ± 9.9 | 0.007 (S) |
| Pre-dilatation | |||
| 12 (12.2%) | 7 (6.9%) | 0.194 (NS) | |
| Number of stents | |||
| One stent | 75 (76.5%) | 89 (87.3%) | 0.048 (S) |
| Two stents | 23 (23.5%) | 13 (12.7%) | |
| Stent diameter (mm) | |||
| Mean ± SD | 3.09 ± 0.36 | 3.07 ± 0.31 | 0.702 (NS) |
| Stent length (mm) | |||
| Mean ± SD | 29.2 ± 7.1 | 27.5 ± 7.3 | 0.100 (NS) |
| Contrast volume (mL) | |||
| Mean ± SD | 163.3 ± 64.0 | 157.4 ± 53.8 | 0.480 (NS) |
Table 4. Comparison between the studied groups regarding the angiographic and procedural data.
There was significant difference in syntax score and number of stents Pvalue (0.007) and (0.048) respectively.
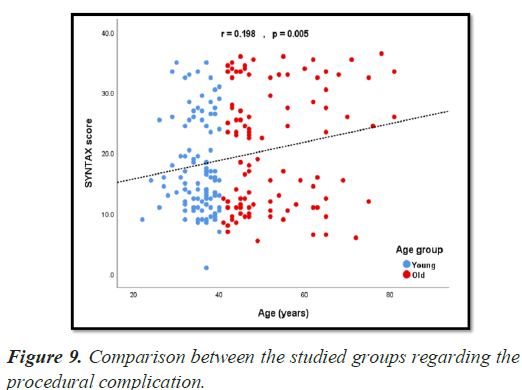
Statistical analysis showed a significant different regarding the procedural complications in both studied age groups with P value (0.011) (P value<0.05) with higher incidence in group II patients with age>40 years (Table 5) (Figure 9).
| Procedural complications | Young (≤ 40 years) | Old (>40 years) | P-value(Sig.) |
|---|---|---|---|
| Count | 98 | 102 | |
| Over-all complication | 23 (23.5%) | 41 (40.2%) | 0.011 (S) |
| Hematoma | 2 (2.0%) | 5 (4.9%) | 0.445 (NS) |
| Spasm | 4 (4.1%) | 10 (9.8%) | 0.113 (NS) |
| Dissection | 3 (3.1%) | 7 (6.9%) | 0.332 (NS) |
| Failed PCI | 3 (3.1%) | 7 (6.9%) | 0.332 (NS) |
| No reflow | 11 (11.2%) | 12 (11.8%) | 0.905 (NS) |
| Death | 3 (3.1%) | 8 (7.8%) | 0.138 (NS) |
Table 5. Comparison between the studied groups regarding the procedural complication.
Statistical analysis showed a significant different regarding the sever CAD (high syntax group) in both old age (0.001), Non-ST ACS (<0.001) and CK-MB (IU/L) (0.028) groups (P value<0.05) (Table 6).
| Variable | Unadjusted OR | 95% Confidence Interval for OR | P-value(Sig.) | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Old age (> 40 years) | 4.68 | 1.93 | 11.348 | 0.001 |
| Male gender | 0.906 | 0.342 | 2.399 | 0.843 |
| HTN | 1.57 | 0.746 | 3.305 | 0.235 |
| Smoking | 1.019 | 0.485 | 2.142 | 0.961 |
| Dyslipidemia | 0.749 | 0.209 | 2.687 | 0.657 |
| Family history | 1.12 | 0.497 | 2.527 | 0.784 |
| Non-ST ACS | 7.56 | 3.333 | 17.148 | <0.001 |
| EF (%) | 1.011 | 0.967 | 1.058 | 0.622 |
| Creatinine (mg/dL) | 1.972 | 0.563 | 6.91 | 0.289 |
| CK-MB (IU/L) | 1.009 | 1.001 | 1.017 | 0.028 |
Table 6. Univariate regression analysis for sever CAD (high SYNTAX group).
Statistical analysis showed a significant different regarding the severe CAD (high syntax group) in both old age (0.001) and Non- ST ACS (<0.001) groups (P value<0.05) (Table 7).
| Variable | Adjusted OR | 95% Confidence Interval for OR | P-value(Sig.) | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Old age (>40 years) | 4.745 | 1.836 | 12.265 | 0.001 |
| Non-ST ACS | 7.489 | 3.159 | 17.756 | <0.001 |
| CK-MB (IU/L) | 1.004 | 0.995 | 1.012 | 0.389 |
Table 7. Multivariate regression analysis for sever CAD (high SYNTAX group.
Statistical analysis showed a significant different regarding the multivessel disease occurrence in both old age (0.006) and Non-ST ACS(0.001) groups (P value<0.05) (Table 8).
| Variable | Unadjusted OR | 95% Confidence Interval for OR | P-value(Sig.) | |
|---|---|---|---|---|
| Lower Bound | Upper Bound | |||
| Old age (> 40 years) | 2.469 | 1.299 | 4.69 | 0.006 |
| Male gender | 1.076 | 0.466 | 2.482 | 0.864 |
| HTN | 1.273 | 0.68 | 2.381 | 0.451 |
| Smoking | 1.267 | 0.68 | 2.362 | 0.456 |
| Dyslipidemia | 0.524 | 0.169 | 1.623 | 0.262 |
| Family history | 0.81 | 0.401 | 1.637 | 0.557 |
| Non-ST ACS | 4.968 | 2.569 | 9.605 | <0.001 |
| EF (%) | 1 | 0.963 | 1.039 | 0.99 |
| Creatinine (mg/dL) | 1.592 | 0.549 | 4.616 | 0.392 |
| CK-MB (IU/L) | 1.006 | 0.999 | 1.013 | 0.121 |
Table 8. Univariate regression analysis for multi-vessel disease.
This table shows statistically significant regarding the multivessel disease in both old age (0.010) and Non-ST ACS(<0.001) groups (Pvalue<0.05) (Table 9).
| Variable | Adjusted OR | 95% Confidence Interval for OR | P-value(Sig.) | ||
|---|---|---|---|---|---|
| Lower Bound | Upper Bound | ||||
| Old age (> 40 years) | 2.456 | 1.24 | 4.865 | 0.01 | |
| Non-STACS | 4.953 | 2.524 | 9.719 | <0.001 | |
Table 9. Multivariate regression analysis of multivessel disease.
Discussion
The clinical presentation and angiographic findings of CAD varies from diabetic and nondiabetic patients and varies with the age of presentation. Coronary artery disease in patients below age of 45 is a special subset [9]. It is generally accepted that early detection of ACD in non-diabetic young aged patients is important clinical problem and increases the probability of cure and decease of the mortality rate, so the aim of this study is the correlation between the risk factors and clinical pictures and coronary angiographic patterns in non-diabetic patients younger than forty five.
This study included two hundred patients to assess the coronary angiographic findings regarding number, type of lesions and severity of CAD in relation to the conventional risk factors and the clinical presentation in younger than forty five years non diabetic patients.
In our current study, the youngest patient presented with acute coronary syndrome was 32 years old, suggesting an early onset of disease and requiring an alarming attention. In a study it showed theyoungest patient presented with ACS was 22 years old [10].
Analysis of risk factors in the current study revealed that male gender, hypertension, smoking, dyslipidemia and family history (83.5%, 38%, 55.5%, 11% and 27.5% respectively) were common among younger patients.
Smoking is known to cause increased fibrinogen concentration and platelets agreeability, along with impaired fibrinolytic activity, decreased coronaryflow reserve and vasospasm [4,8]. Smoking has been traditionally recognized as the most common risk factors for CHD, particular among young patients [12]. This is in agreement with other studies of similar nature [13-15].
It should be emphasized that smoking are reversible so smoking cessation may thus prove to be one of the most cost effective approach in both primary and secondary prevention.
Dyslipidemia was less in our patients which represent 22 cases in line in one of the study [11].
Hypertension was highly significant as two times more common in older patients as younger patients, similar finding was concluded in one of the study, this fading was matching with our study which detect 76(38%) of cases had hypertension.
As regard the family history many previous studies showed that familyhistory is a strong independent predictor of significant CAD in younger patients. It has been documented, that children born of parents with premature CAD tend to have more lipid abnormalities, insulin resistance and obesity strengthening the belief of a common genetic linkage and genetic polymorphism, indicating that family history of CAD is an important risk factor in young adults with ACS, this consistent with our study that detect 55 cases had family history of ACS [10].
In most of the studies single vessel disease (SVD) is the most common angiographic finding in young CAD in non-diabetic, while the diabetics showed the more diffuse pattern of double vessel disease (DVD) [9].
The LAD vessel is most affected vessel in our study, which detected in 171(85%) patients followed by RCA and LCX winch detected n 103(51.5%) and 85(42.5) patients respectively these findings were in agreement with study was done [10].
Finally by measuring the severity of the coronary artery disease lesion using the syntax score, we found that most cases has low syntax score, and regard the severity of coronary lesion current study showed preponderance of single vessel disease, these finding were Consistent with other work was done [12].
Conclusion
Young patients with ACS had different risk profile and less extensive coronary artery disease as compared to older patients with ACS. As in our study, it was observed that smoking, substance abuse, dyslipidemia and single vessel and less extensive disease were significantly higher in younger age group below 40 years old with ACS. On the other hand, DM, hypertension, multivessel, extensive diseases and the mean of syntax score were significantly higher in older age group more than 40 years old with ACS.
Many early studies evaluating these patients labeled them as having premature CAD, but it isnow better understood as a rapidly progressive form of the disease.
Limitations• We evaluated the standard coronary risk factors, while the other newer risk factors such as lipoprotein abnormalities, hypercoagulable states, and elevated homocysteine levels were not studied.
• The lack of long term follows up after hospital discharge.
• Study of emerging risk factors and their relation to ACS in young needs to be addressed in larger randomized controlled trials
Recommendations
• The study of ACS is important in the current era of primary and secondarypreventive cardiology, hence, we highlight and emphasis on diagnosis and management of major modifiable risk factors especially for younger patients is very crucial in the primary and secondary prevention of cardiovascular disease.
• Applying strict primary and secondary prevention parameters would definitely be reflected on decreasing the economic burden resulting from treatment of younger patients presenting with ACS in Egypt.
• Future prospective studies are needed to develop particular guidelines directing the diagnosis of risk factors and angiographic features ofACS in younger patients and it is management.
References
- Conroy RM, Pyorala K, Fitzgerald AE, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. European Heart Journal. 2003;24(11):987-1003.
- Barbero U, Scacciatella P, Iannaccone M, et al. Culprit plaque characteristics in younger versus older patients with acute coronary syndromes: An optical coherence tomography study from the formidable registry. Catheterization and Cardiovascular Interventions. 2017;92(1):1-8.
- Akcay M, Yuksel S. Smoking and cardiovascular diseases. J Exp Clin Med. 2017;34(1):21-5.
- Ambrose JA, Singh M. Pathophysiology of Coronary Artery Disease Leading to Acute Coronary Syndromes. F1000prime Reports. 2015;7:8.
- Abdallah MS, Wang K, Magnuson EA, et al. Quality of life after PCI vs. CABG among patients with diabetes and multivessel coronary artery disease: A randomized clinical trial. Jama J. Am. Med. Assoc. 2013;310(15):1581-90.
- Ahmed E, El-Menyar A, Singh R, et al. Effect of age on clinical presentation and outcome of patients hospitalized with acute coronary syndrome: A 20-year registry in a Middle Eastern Country. Open Cardiovasc Med J. 2012;6(1):60-7.
- Avezum A, Makdisse M, Spencer F, et al. Impact of age on management and outcome of acute coronary syndrome: Observations from the Global Registry of Acute Coronary Events (GRACE). Am Heart J. 2005;149(1):67-73.
- Morital L, Brown JP, Clark AM, et al. Patient education in the management of coronary heart disease. Cochrane Database Syst Rev. 2017;6(6):CD008895.
- Narayanan L, hanifah M, Ballard BD, et al. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL). Cardiovasc Dis.2020
- Bauersachs R, Zeymer U, Brière JB, et al. Burden of coronary artery disease and peripheral artery disease: a literature review. Cardiovasc Therap. 2019;2019:1-9.
- Juonala M, Magnussen CG, Berenson GS, et al. Childhood adiposity, adult adiposity, and cardiovascular risk factors. N Engl J Med. 2011;365:1876-85.
- Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007;356(15):1503-16.
- Barua RS, Sy F, Srikanth S, et al. Effects of cigarette smoke exposure on clot dynamics and fibrin structure: An ex vivo investigation. Arterioscler Thromb Vasc Biol. 2010;30(1):75-9.
- Brown JC, Gerhardt TE, Kwon E. Risk factors for coronary artery disease. StatPearls [Internet]. 2020.
- Yadav P, Joseph D, Joshi P, et al. Clinical profile and risk factors in acute coronary syndrome. National J Comm Med. 2010;1(2):150-1.