Research Article - Journal of Orthopedic Surgery and Rehabilitation (2023) Volume 7, Issue 5
A Seven-Year Retrospective Outcome Study of a Medial Extensile Surgical Tarsal 5 Tunnel Release in the Treatment of Tarsal Tunnel Syndrome
Brian G. Loder1*, Andrew Mastay1, Katherine Morrison1, Steven Goldstein1, Geoffrey K. Seidel21Department of Podiatric Surgery, Henry Ford Macomb Hospital, Clinton Township, United States
2Departments Physical Medicine and Rehabilitation, Wayne State University and Michigan State University, Detroit, United States
- *Corresponding Author:
- Brian G. Loder
Department of Podiatric Surgery
Henry Ford Macomb Hospital
Clinton Township, United States
E-mail: bloder@detroitfa.com
Received: 24-Aug-2023, Manuscript No. AAOSR-23-108109; Editor assigned: 28-Aug-2023, PreQC No. AAOSR-23-108109(PQ); Reviewed: 11-Sept-2023, QC No.AAOSR-23-108109; Revised: 16-Sept-2023, Manuscript No.AAOSR-23-108109(R); Published: 22-Sept-2023, DOI: 10.35841/ aaosr-7.5.161
Citation: Loder B, Mastay A, Morrison K, et al. A seven-year retrospective outcome study of a medial extensile surgical tarsal tunnel release in the treatment of tarsal tunnel syndrome. J Ortho Sur Reh.2023;7(5):161
Abstract
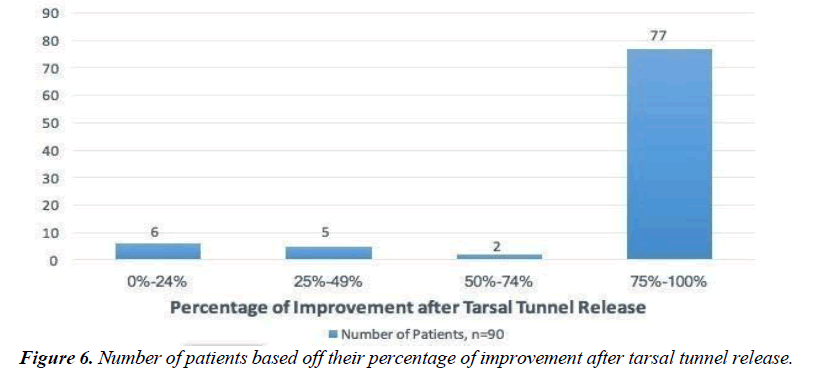
This study aims to analyze the clinical results of using a medial extensile surgical approach for decompression of the tibial nerve, including its distal medial and lateral branches, to treat tarsal tunnel syndrome. These structures are the complete flexor retinaculum and the deep fascia of the abductor halluces muscle, including individualized release of the medial and lateral plantar nerve tunnels. Method: This is a retrospective review of 90 surgical releases in 79 patients (19 men and 71 women) with an average age of 50 years compatible with idiopathic tarsal tunnel syndrome, which underwent an extensive medial decompression technique of the proximal and distal tarsal tunnel. Results: Of the 90 released 77 reported outcomes in the75thpercentile or better. There were 17 incidents of infection which resulted in 12 cases of wound dehiscence, which were all successfully managed. Conclusion: The extensile approach to tarsal tunnel release offers successful outcomes for the treatment of tarsal tunnel syndrome with low reoccurrence rates.
Keywords
Tarsal tunnel, Open approach, Electro diagnostic testing.
Introduction
Tarsal Tunnel syndrome is a relatively misunderstood pathology in the lower extremity. First described by Kopell and Thompson in 1960 and then by Keck and Lam in two separate studies in 1962, Tarsal tunnel syndrome is an entrapment syndrome of the entire tibial nerve behind the medial malleolus and under the flexor retinaculum or laciniate ligament [1-3].The clinical presentation is typically tenderness posteromedial over the nerve. In some patients there can be true neurogenic signs including both the sensation of numbness and actual hypoesthesia and clawing of the toes. Tinel sign as a diagnostic criterion has been met with some variability in the literature [4-6]. The underlying cause of Tarsal tunnel syndrome has been attributed to multiple pathologies including space occupying mass, anomalous muscle belly, tarsal coalition, trauma, venous malformation and limb lengthening procedures [7-19]. The literature reveals some of the best outcomes are associated with the removal of space-occupying lesions that are within the tarsal tunnel canal [20, 21]. In contrast, some of the poorest outcomes have been associated with re- operation of a failed tarsal tunnel [22-25]. Regardless of the cause a full work up to evaluate all intrinsic and extrinsic factors should be undertaken before any surgical intervention is performed. The diagnosis of tarsal tunnel is made with a thorough history and physical exam with the aid of ancillary studies. Patients usually present with medial ankle and plantar foot pain, worse with activity but also present at rest. Many times, the patient’s only complaint is heel or sub-metatarsal pain and the physician can be misled into treating the wrong diagnosis [26-28]. Ancillary studies that have proved to be helpful in the confirmation of the tarsal tunnel syndrome diagnosis include MRI, ultrasound and electro diagnostic studies [29-35]. In a small study of 9 patients by Samarawickrama, et al all of the patients with a positive EMG study had confirmation of a tarsal tunnel syndrome with ultrasound, revealing overlapping studies may help to confirm the diagnosis and reassure the patient and the surgeon of the appropriate treatment.The treatment of tarsal tunnel syndrome includes a myriad of non- surgical treatments including bracing, orthotics, physical therapy, immobilization and nerve blocks [36-38]. Surgical treatment of tarsal tunnel syndrome can be performed either as an endoscopic or open approach. The endoscopic tarsal tunnel release has received more attention lately but is more technical and requires a particular skill set by the surgeon [39-42]. The open procedure can be further divided into a minimal incision and extensile incision approach. The literature is replete with studies that reveal incomplete release is a major cause of tarsal tunnel release failure [43]. In this study the authors present 90 cases of extensile tarsal tunnel release over a period of seven years followed to stabilization of symptoms. All the releases were performed by the lead author. A detailed surgical technique is described as well as post-operative outcomes and surgical complications are reported the authors aim to prove that an extensive release provides the ability to release all compartments while minimizing post-surgical complications and inadequate release.
Surgical Technique
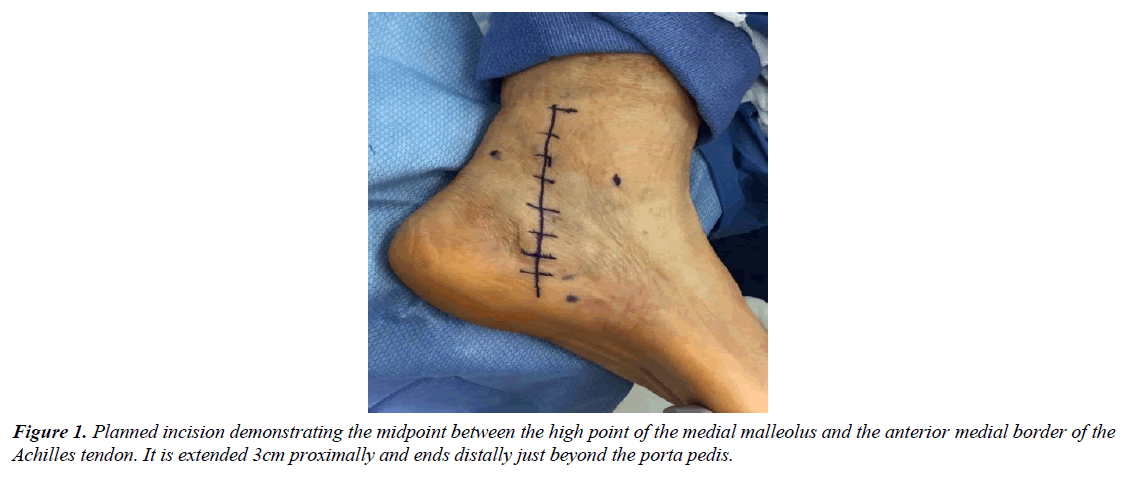
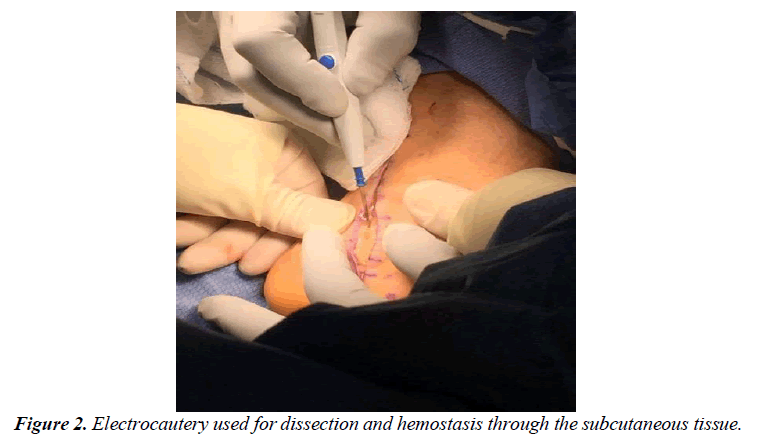
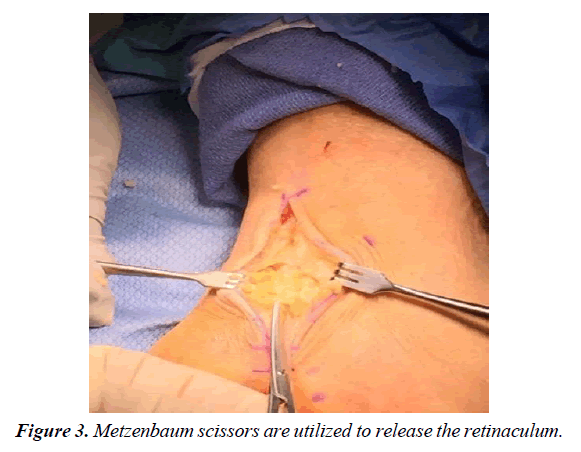
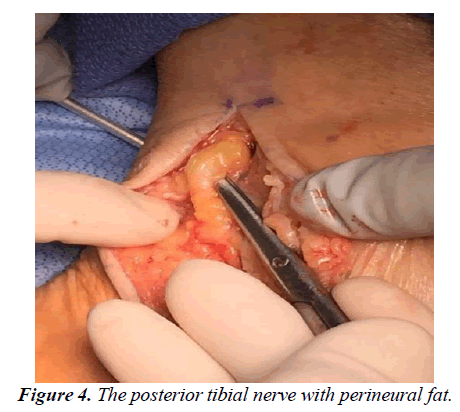
The patient is transferred to the OR suite and placed on the table in the supine position. A general anaesthetic was instituted, and a thigh tourniquet is used for hemostasis. After a standard prep and drape, the incision is marked in the posterior medial aspect of the ankle. The incision is centered halfway between the high point of the medial malleolus and the anterior medial border of the Achilles tendon and extended three centimeters proximal to this marked line as well as distally just beyond the porta pedis (Figure 1). A controlled depth skin incision is performed, and care is taken in the initial incision to cauterize all perforators and skin bleeders (Figure 2). The retinaculum is identified and all constrictors in the retinaculum are noted. A small rent is created in the retinaculum with a scalpel, taking care to avoid an iatrogenic injury to the neurovascular structure deep in the ligament. A blunt scissor is then used to release the retinaculum both distal and proximally completely, with special attention to the distal aspect deep to the abductor halluces muscle belly (Figure 3). Care must be taken to ensure the deep fascia of the posterior leg as well as the deep investing fascia of the abductor muscle belly is released in its entirety. The nerve is identified proximally and gently released utilizing a technique that worked from the edge of the neural tissue into the tarsal tunnel (Figure 4). No instrumentation directly contacted the nerve through the dissection this dissection was carried completely proximal to distally making sure to release all branches of the nerve distally. The focus of the dissection is to identify any soft tissue masses in the tarsal canal, release of any vascular slings if present, and gently free the posterior nerve and its branches from the retinaculum posteriorly. Once the nerve has been completely released, the perineural space is instilled with 8mg of dexamethasone with a 30-gauge needle. The proximal incision is instilled with a long-acting anaesthetic for post- operative pain control. Prior to any closure, the thigh tourniquet is released, and a bloodless field is maintained with cautery. Finally, the wound is closed in layers without approximation of the retinaculum and a well-padded posterior splint is applied (Figure 5). The post-operative protocol allows weight bearing in the splint for two weeks to protect the incision site. At the two-week follow-up, the splint and sutures are removed, and the patient is encouraged to start full weight bearing in the shoe of their choice.
Methods
A retrospective review of tarsal tunnel release procedures performed from January 2010 to December 2017 was carried out by gathering data from the hospital EMR and the lead surgeon’s clinical office. We obtained approval from our institution’s review board at Henry Ford Health System, after an expedited review. All surgical procedures were performed by the lead author. The query resulted in 104 cases of tarsal tunnel release. Fourteen cases were Excluded from the study due lack of follow up. In total, 90 tarsal tunnel releases were performed on 79 patients. Reviewed information consisted of age, sex, side of surgery, presence of diabetes, subjective symptoms of peripheral neuropathy, whether a diagnostic posterior tibial nerve block was performed, and whether an EMG was performed. A successful diagnostic block is defined as any block that produces lasting symptom relief greater than 8 hours. All diagnostic blocks were performed by the primary surgeon and were comprised of a combination of Kenalog 40mg, Marcaine 0.5% and lidocaine 2%. Post- operative information consisted of wound dehiscence, post-operative infection, and subjective percentage of improvement based upon patient’s subjective improvement rating.
Result
In total, 90 tarsal tunnel releases were performed on 79 patients. The average time of follow up was 529 days. The average age was 50 years. There were 49 procedures performed on the left foot and 41 on the right. There were 71 females compared to 19 males (Table 1). Subjective neurogenic symptoms were described in 83 (92%) of the cases. Of the 90 performed procedures, 77 (85.56%) exhibited ≥ 75% improvements at final follow up, which was determined by stabilization of symptoms. A diagnostic nerve block was performed on 57 (63.33%) limbs with 84.21% of those patients achieving a ≥ 75% improvement after surgical intervention (Figure 6). Preoperative electro diagnostic evaluated patients who had tarsal tunnel releases reported symptom improvement >74% in 89% (71/80). There were 17 incidences of post-operative infection and 12 surgical sites dehisced. All postoperative complications were successfully managed and despite these events 26/29(90%) patients who experienced complications reported >74% improvement postoperatively.
| Total Number of Tarsal Tunnel Releases | 90 |
| Number of Females | 71 |
| Number of Males | 19 |
| Average Age yrs. | 50 |
| Left Foot | 49 |
| Right Foot | 41 |
Table 1. Demographic information.
Discussion
In our study we have shown that the diagnosis of tarsal tunnel syndrome is dependent on a cumulative amount of data including patient history, clinical findings, ancillary studies. Of the 77 patients examined, ≥ 75% reported improvement in their clinical symptoms. We were also able to find a correlation between the success of tarsal tunnel syndrome and the success of a diagnostic block, with 84% of patients reporting ≥ 75% improvementDifferent surgical approaches have been described in literature and each has their merits. Our surgical approach was based on the anatomical location of the posterior tibial nerve. We have found that keeping the incision directly over the neurovascular bundle reduces the dissection needed to inspect and release the nerve. This directly reduces scarring around the nerve, which we believe lowers our failure rate. Another important part of our surgical approach is the length of the surgical incision. The direct relationship between incomplete release and patient satisfaction in the literature has led our lead author to define the appropriate incision length to avoid incomplete release of the nerve and its branches. Finally, avoiding manipulation of the posterior tibial nerve and its branches has allowed reduced scarring around the nerve. This is aided with the absolute rule to release the tourniquet prior to closure of the incision to ensure a bloodless field. The authors stress the importance of protecting the incision for two weeks in a posterior splint to reduce the possibility of wound dehiscence and thus the overall surgical success. We acknowledge deficiencies in our research. First, this was a retrospective study. Furthermore, our end point was defined by a stabilization of the patient’s symptoms and not a defined length of time. It is possible that higher overall patient satisfaction rates may have been reported if patients had been followed for a longer time. In conclusion, our data has shown that a medial extensile release of the tarsal tunnel using our specific technique yields consistently good outcomes and high patient satisfaction. The diagnosis of tarsal tunnel should be gained from a thorough work-up that includes a patient’s history, a thorough physical exam and ancillary studies to rule out any musculoskeletal causes of the symptoms. Further studies are needed to evaluate the tarsal tunnel release post-surgically with electro diagnostic evaluation to determine the true success of the procedure.
References
- Kopell HP, Thompson WA. Peripheral entrapment neuropathies of the lower extremity.N Engl J Med.1960;262(2):56-60.
- Keck C. The tarsal-tunnel syndrome. J Bone Joint Surg Br. 1962;44(1):180-2.
- Lam SJ. A tarsal-tunnel syndrome.Lancet.1962;280(7270):1354-5.
- Datema M, Hoitsma E, Roon KI, et al.The Tinel sign has no diagnostic value for nerve entrapment or neuropathy in the legs. Muscle Nerve.2016; 54(1):25-30.
- Dellon Al, Muse Vl, Scott Nd. A positive Tinel sign as predictor of pain relief or sensory recovery after decompression of chronic tibial nerve compression in patients with diabetic neuropathy. J Reconstr Microsurg.2012;28(04):235-40.
- Rinkel Wd, Cabezas Mc, van Neck Jw, et al.Validity of the Tinel sign and prevalence of tibial nerve entrapment at the tarsal tunnel in both diabetic and nondiabetic subjects: A cross-sectional study.Plast Reconst Surg.2018;142(5):1258-66.
- Ho Vw, Peterfy C, Helms Ca. Tarsal tunnel syndrome caused by strain of an anomalous muscle: An MRI-specific diagnosis.J Comput Assis Tomogr.1993;17(5):822-3.
- Sammarco Gj, Conti Sf.Tarsal tunnel syndrome caused by an anomalous muscle.J Bone Jt Surg.1994; 76(9):1308-14.
- Duran-Stanton Am, Bui-Mansfield Lt.Magnetic resonance diagnosis of tarsal tunnel syndrome due to flexor digitorum accessorius longus and peroneocalcaneus internus muscles. J Comput Assist Tomogr.2010;34(2):2702.
- Carrington SC, Stone P, Kruse D. Accessory soleus: a case report of exertional compartment and tarsal tunnel syndrome associated with an accessory soleus muscle. J Foot Ankle Surg.2016; 55(5):1076-8.
- Kwon JH, Yoon JR, Kim TS, et al.Peripheral nerve sheath tumor of the medial plantar nerve without tarsal tunnel syndrome: A case report. J Foot Ankle Surg.2009;48(4):477-82.
- Yoneda A, Sugimoto K, Tsukada N, et al.Glomus tumor in the tarsal tunnel: A case report.J Foot Ankle Surg.2017;56(4):865-7.
- Takakura Y, Kumai T, Takaoka T,et al.Tarsal tunnel syndrome caused by coalition associated with a ganglion.J Bone Joint Surg Br.1998;80(1):130-3.
- Bhat AK, Madi S, Mane PP, et al.Bilateral tarsal tunnel syndrome attributed to bilateral fibrous tarsal coalition and symmetrical hypertrophy of the sustentaculum tali.Case Rep.2017; 2017: bcr-2017.
- Webster Pl, Jagt D, Tiemessen Ct .Post-traumatic tarsal tunnel syndrome-the unrecognized entrapment neuropathy. J Bone Jt Surg Am.1999;81:309.
- Alpar EK, Howell N, Masood I. Traumatic tarsal tunnel syndrome: The outcome of surgical decompression.Foot Ankle Surg.2002;8(1):41-4.
- Mufty H, Matricali GA,Thomis S.Venous malformation as source of a tarsal tunnel syndrome: treat the source or the cause of the complaints? A case report.Acta Chir Belg.2018;118(3):188-91.
- Lamm BM, Paley D, Testani M, et al. Tarsal tunnel decompression in leg lengthening and deformity correction of the foot and ankle. J Foot Ankle Surg.2007;46(3):201-6.
- Primadi A, Kim Bs, Lee Kb. Tarsal tunnel syndrome after total ankle replacement-A report of 3 cases. Acta Orthop. 2016;87(2):205-6.
- Sung KS, Park SJ. Short-term operative outcome of tarsal tunnel syndrome due to benign space-occupying lesions.Foot Ankle Int.2009;30(8):741-5.
- Sammarco GJ,Chang L.Outcome of surgical treatment of tarsal tunnel syndrome.Foot Ankle Int.2003;24(2):125-31.295
- Sammarco GJ, Chang L.Outcome of surgical treatment of tarsal tunnel syndrome.Foot Ankle Int.2003;24(2):125-31.
- Barker AR, Rosson GD, Dellon AL.Outcome of neurolysis for failed tarsal tunnel surgery.J Reconstr Microsurg.2008;24(02):111-8.
- Gould Js.The failed tarsal tunnel release.Foot Ankle Clin.2011;16(2):287-93.
- Yalcinkaya M,Ozer UE,Yalcin MB,et al.Neurolysis for failed tarsal tunnel surgery.J Foot Ankle Surg.2014;53(6):794-8.
- Stroud CC. Heel pain, plantar fasciitis, and tarsal tunnel syndrome.Curr opin Orthop.2002;13(2):89-92.
- Arslan A, Koca TT, Utkan A, et al.Treatment of chronic plantar heel pain with radiofrequency neural ablation of the first branch of the lateral plantar nerve and medial calcaneal nerve branches.J Foot Ankle Surg.2016;55(4):767-71.
- Antoniadis G, Scheglmann K.Posterior tarsal tunnel syndrome: Diagnosis and treatment.Dtsch rztebl Int.2008;105(45):776.
- Zeiss J, Fenton P, Ebraheim N,et al.Magnetic resonance imaging for ineffectual tarsal tunnel surgical treatment.Clin.Orthop Relat Res.1991;264:264-6.
- Bayat E, Kelly JJ, Russo M, et al. Magnetic resonance imaging neurography in an unusual case of tarsal tunnel syndrome. Muscle Nerve. 2006;34(4):535-535.
- Coraci D, Ioppolo F, Di Sante L, et al.Ultrasound in tarsal tunnel syndrome: correct diagnosis for appropriate treatment. Muscle & nerve.2016;54(6):1148-9.
- Samarawickrama D,Therimadasamy Ak,Chan Yc, et al.Nerve ultrasound in electro physiologically verified tarsal tunnel syndrome. Muscle & Nerve.2016; 53(6):906-12.
- Kaplan Pe, Kernahan Jr Wt. Tarsal tunnel syndrome: An electro diagnostic and surgical correlation.J Bone Joint Surg Br.1981;63(1):96-9.
- Patel At, Gaines K, Malamut R,et al.Usefulness of electrodiagnostic techniques in the evaluation of suspected tarsal tunnel syndrome: An evidence‐based review. J Am Ass Electr dia Med.2005;32(2):236-40.
- Lindstrom H, Ashworth Nl.The usefulness of electrodiagnostic studies in the diagnosis and management of neuromuscular disorders.Muscle Nerve.2018;58(2):191-6.
- Sobey Jh,Franklin A.Ultrasound-guided tibial nerve block for definitive treatment of tarsal tunnel syndrome in a pediatric patient.Reg Anesth Pain Med.2016;41(3):415-6.
- Burke CJ, Adler Rs.Tibial Nerve Block Using an Ultrasound‐Guided Inframalleolar Medial Plantar Nerve Perineural Injection: A Technical Note.J Clin Ultrasound.2017; 45(3):134-7.
- Kushner S, Reid DC.Medial tarsal tunnel syndrome: A review.J Orthop Sports Phys Ther.1984;6(1):39-45.
- Day Fn, Naples Jj. Tarsal tunnel syndrome: An endoscopic approach with 4-to 28-month follow-up.J Foot Ankle Surg.1994;33(3):244-8.
- Krishnan KG, Pinzer T,Schackert G. A novel endoscopic technique in treating single nerve entrapment syndromes with special attention to ulnar nerve transposition and tarsal tunnel release: Clinical application.Oper Neurosurg.2006;59(1):ONS-89
- Krishnan KG. Endoscopic decompression of the tarsal tunnel.J Foot Ankle Surg.2010;9(2):52
- Yoshida A, Okutsu I, Hamanaka I.Endoscopic tarsal tunnel syndrome surgery using the Universal Subcutaneous Endoscope system. Asia-Pac.J Sports Med Arthrosc.2016;3:1-5.
- Gould JS. Recurrent tarsal tunnel syndrome.Foot Ankle Clin.2014;19(3):451-67.
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref
Indexed at, Google scholar, Cross ref