Case Report - Otolaryngology Online Journal (2018) Volume 8, Issue 1
Vocal Fold Granulomas: A Case Series
Dian Paramita Wulandari*, Rangga Putra Nugraha, Jessica Fedriani and Hermawan SuryaDepartment of Otolaryngology, Sardjito General Hospital, Gadjah Mada University, Indonesia
- *Corresponding Author:
- Dian Paramita Wulandari
Faculty of Medicine
Department of Otolaryngology
Sardjito General Hospital
Gadjah Mada University
Indonesia
Mobile: +62 274 581876
Email: dian.pewe@gmail.com
Received date: January 29, 2018; Accepted date: February 03, 2018; Published date: February 09, 2018
Abstract
Background: Vocal fold granulomas are still largely unidentified by otolaryngologist. This entity could be one of the most prevalent causes of extubation failure, aside from subglottic stenosis. Postintubation granuloma is one of post-endotracheal intubation complications. Prolonged intubation or history of multiple intubation increases the risk of granuloma formation. Thus we need to be aware of the existence possibility of this pathologic condition
Introduction: During January 2014 to January 2017 at Sardjito General Hospital, it has been reported four cases of post-intubation vocal fold granuloma. Three cases with prolonged intubation, one case with long hours operation. All patients were female.
Case Report: The first case was a 28 years old woman with bilateral vocal fold granuloma, had history of multiple operations with general anesthesia using endotracheal tube intubation, and also history of prolonged intubation in the ICU. Endoscopic examination revealed bilateral large vocal fold masses. After removal of granulomas, we administered intraoral steroid and PPI therapy and the patient was relief completely with no tightness or hoarseness post-operative. The second case, a 59 years old woman with unilateral laryngeal granuloma with history of craniectomy. Endoscopic examination showed large size unilateral granuloma which moved along with inspiration and expiration. The patient was then managed by microlarynx surgery and showed no recurrence at evaluation. The third case was a 25 years old woman with unilateral granuloma which has been managed with anti-inflammatory drugs for 2 weeks without any changes in the size of mass. This patient also had history of prolonged intubation in the ICU due to pneumonia. The granuloma was removed with microlarynx surgery. The fourth case, a 24 years old female with history of prolonged intubation and tracheal stenosis post repair, endoscopic examination showed a unilateral mass in the left posterior commissure; patient was managed conservatively, and has not yet come for follow up.
Conclusion: Four cases of bilateral and unilateral post-intubation laryngeal granulomas associated with history of intubation were reported.
Keywords
Vocal fold granuloma; Prolonged intubation
Background
Vocal cord granuloma is a structure caused by inflammation process arise from perichondrium area around aritenoids cartilage. It is estimated that this granuloma was caused by perichondritis of the aritenoids cartilage, which was resulted from trauma of mucosal or perichondrium areas of the aritenoids cartilage.
Laryngeal granuloma may occurs as unilateral or bilateral masses with a variety of colours, from white, reddish, even purplish, and majority has pedicles that attached to posterior glottis areas, mainly at the apophysis vocalis [1].
Even though maximal prevention measures have been performed, this granuloma may occurs as a complication of endotracheal intubation procedure.Endotracheal intubation can causes trauma of the mucosal of aritenoids cartilage, while trauma of the aritenoids cartilage perichondrium can be caused by suppression at prolonged endotracheal intubation or by laryngopharyngeal reflux (LPR) [2].
The development of granuloma is varied and individualized. Some patients can tolerate the use of endotracheal tube for couple days without experience laryngeal injury, and other patients develop granuloma only after short period of intubation. In the literature, the occurrence of post intubation laryngeal granuloma was reported to be rare, some report 1 case every 800-1000 intubation, there is even a literature that reports one case every 10000 intubation [3].
The pathophysiology of granuloma development is an inflammatory reaction of the tissues that causes over proliferation of those tissues, and eventually the granuloma develops.
The possible mechanisms that cause laryngeal granuloma are:
1. Vocal misuse or vocal abuse [1,4]
2. Habitual coughing,
3. Gastroesophageal or laryngopharyngeal reflux [4]
4. Trauma
5. Endotracheal intubation [4,5]
6. Idiopathic [1]
Laryngeal granuloma can mimics malignancy of the larynx, therefore anatomical pathology examination is still needed to confirm this diagnosis.
The optimal management of laryngeal granuloma is still being topic of debate until now. Generally, its therapeutic strategies include corticosteroid, vocal hygiene and/or surgery accompanied by risk factors elimination. Patients will have a high recurrence risk if their risk factors were not well controlled [5]. The most important prevention strategies for the development or recurrence of laryngeal granuloma are by controlling risk factors or avoiding the underlying causes.
Intubation could be a risk factor for the development of laryngeal granuloma. The endotracheal tube that placed inside larynx even only for short duration can cause mucosal superficial damage. In prolonged intubation, pressure necrosis can emerges which eventually will spread into the submucosal, perichondrium, and the cartilage areas. Even short term intubation can cause serious damage to the glottis and transglottis areas [6]. For adult, the damage frequently occurs inside the posterior glottic area, and it is in subglottic area for pediatric patients.
Factors that influence the development of granuloma are as follows:
Extrinsic factors:
1. Diameter, shape, and the contour of endotracheal tube
2. Duration of the intubation time
3. Traumatic/multiple intubation [6]
Therefor to prevent the development of microtrauma, we can cultivate to use the minimum tube size possible, shorten the intubation duration, and avoid multiple intubation [7].
The management of laryngeal granuloma are as follows:
1. Conservative treatment is prioritized by using antiinflammation regimen or corticosteroid, systemic or topical [4,8,9]
2. Controlling risk factors; such as laryngopharyngeal reflux (LPR) with proton pump inhibitor (PPI), allergy with antiallergic medications, and antibiotic for infection [9]
4. If the granuloma is persistent and unresponsive to the therapy or if there is an airway obstruction risk, operative granuloma extirpation needs to be performed.
Introduction
During January 2014 to January 2017 at Sardjito General Hospital, it has been reported four cases of post-intubation vocal fold granuloma. Three cases with prolonged intubation, one case with long hours operation. All patients were female. One patient had bilateral vocal cord granulomas, while three others are unilateral. Three cases of vocal cord granulomas were removed by microlaringoscopic surgery, two cases were operated due to risk of upper airway obstruction, one for biopsy, and the fourth was managed conservatively.
Case Report
The first case was a 28 years-old woman patient who came with main symptom of hoarseness and sometimes it was accompanied with the loss of voice and dyspnea. The hoarseness was noticed since she had surgery procedure about 3 months before went to the ENT clinic and it was progressive since the last 3 weeks. The hoarseness was noticed since she was took off from her ventilator 3 months before went to the ENT clinic. This patient was treated in the ICU with endotracheal tube and ventilator for 7 days. In the ICU two surgery procedures were performed, and 1 week after discharged from ICU this patient underwent maxillary reconstruction surgery with general anesthesia using endotracheal intubation. One month after, she underwent plate removal surgery in jaw, and plate placement surgery in hand one and a half month later. Overall this patient had undergone 6 surgeries since the accident that happened 4 months before.
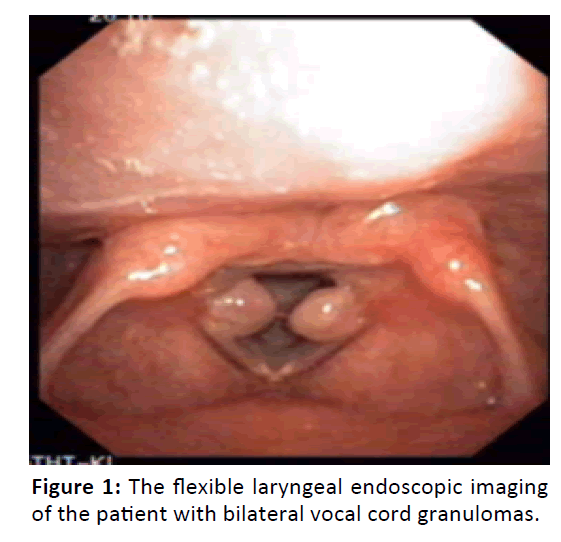
Flexible laryngeal endoscopic examination was performed for this patient in the ENT clinic and it revealed a large size of bilateral granulomas on posterior commissure of the vocal cords. Looking at her history with multiple surgeries and multiple endotracheal intubations, we concluded that this case was a postintubation granuloma. This patient started to complain progressive dyspnea, and considered the size of the granuloma that quite massive and bilateral hence it had risk to cause upper airway obstruction, we decided to perform granuloma extirpation procedure with microlaryngeal surgery (Figure 1).
Removal granuloma surgery with general anesthesia was performed for this patient. The anesthetic was performed with intubation using small size endotracheal tube. After the patient was intubated, direct laryngoscopy and operative field visualization were performed using endoscopy technique. Large size granulomas on both posterior commissure of the vocal cord were seen. Granulomas then were grasped using curved microlaryngeal forceps and they were pulled to the medial side, granuloma excision then was performed with dissection and the slice of granuloma stalk was performed using curved microlaryngeal scissors. Both granulomas could be completely removed with only minimal bleeding and it was controlled using adrenaline.
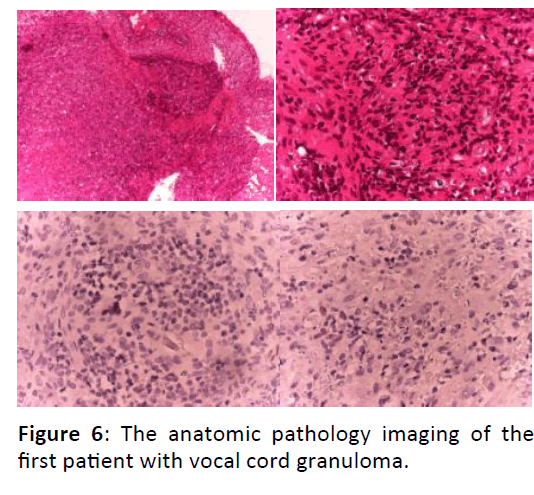
The excised tissues subsequently were sent to the anatomical pathology department to be evaluated. Postoperatively, this patient was given antibiotic cefadroxil 500 mg twice time a day for 7 days, methilprednisolone 16-8-0 mg with tapered off doses, diclofenac potassium 50 mg twice time a day and lansoprazole 30 mg twice time a day. This patient went to ENT clinic one week after surgery and brought her AP result with her. The results of her AP JRS 16-709 evaluation is: right and left vocal cords: pyogenic granuloma with suspicious areas of “spindle cell carcinoma”. Suggestions: evaluation of IHC cytokeratin and Ki67. After the evaluation of IHC cytokeratin and Ki67 were performed, the results of her AP HIS 16-143 is: evaluation of IHC cytokeratin and Ki67 Larynx: in accordance with inflammation process with granulation tissues.
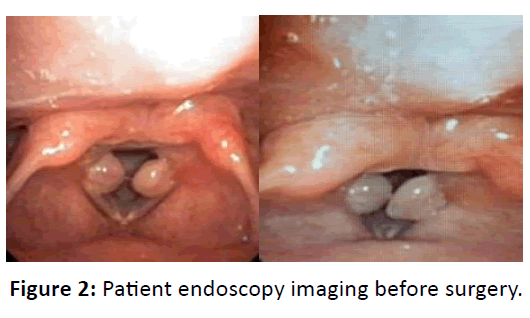
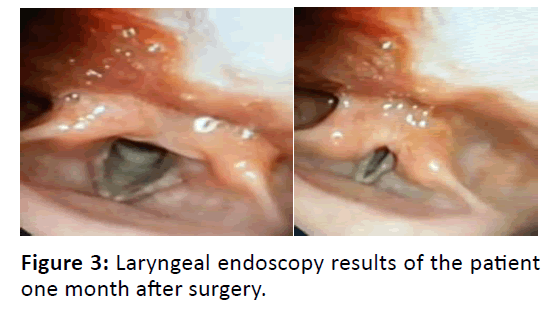
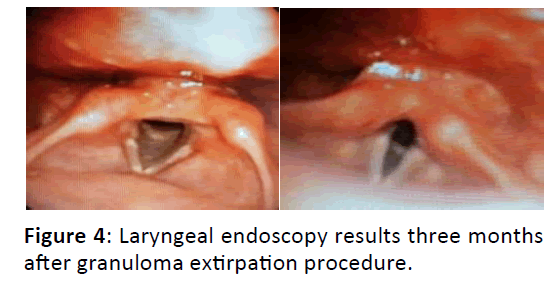
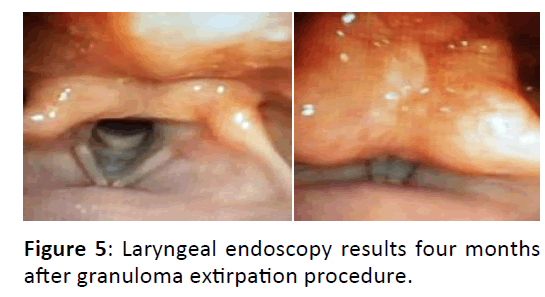
From the evaluation results of postoperative laryngeal endoscopy, granuloma tissue was no longer found and the mobilization of the vocal cords were found to be normal. Patient could produce normal voice and hoarseness or dyspnea was no longer found. The methylprednisolone treatment was tapered off, and the PPI treatment was continued. One month after, this patient went to ENT clinic and endoscopic evaluation was performed which still showed good results, there were no granulation tissues found (Figures 2-6).
This patient went to ENT clinic at one week, one month, three months, and four months after surgery, all showed good results and no granuloma recurrence was found.
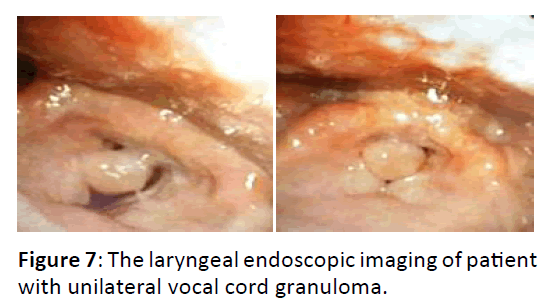
The second case, a 59 years-old woman, came to ENT-HN clinic with hoarseness that was noticed since two weeks after craniectomy surgery six months before she went to ENT clinic at Sardjito hospital. She noticed that her hoarseness was progressive and sometimes she lost her voice. Before came to Sardjito hospital, this patient went to a hospital in Bandung and a surgery procedure was planned but it was cancelled because of the long queue. Flexible laryngeal endoscopic examination was performed with the results showed a large size granuloma at right vocal cord with pedicle at posterior commissure that reached right supraglottic area and this granuloma moved inside and outside from rima glottis in accordance with inspiration and expiration movement of the patient.
As with the first case, the granuloma in the second case also had a large size, had risk to cause airway obstruction, and need to biopsied because this granuloma mimicked laryngeal papilloma, therefore extirpation with microlaryngeal surgery were performed. Neuroleptic technique was performed to anaesthetize patient without endotracheal intubation, the mass then was grasp with curved microlaryngeal forceps, it was pulled to the medial side, and granuloma base dissection was performed with curved microlaryngeal scissors. The tissue and mucosal residues were completely removed during laryngeal forceps and scissors. The bleeding was minimal and was controlled with applicator and cotton with adrenaline. The tissues could be removed completely, and were sent to the anatomical pathology department for evaluation. This patient was discharged home with antibiotic therapy of cefadroxil 500 mg twice time a day, metilprednisolone 16-8-0 mg with tapered off doses, lansoprazole 30 mg twice time a day, and diclofenac potassium 25 mg twice time a day and she was advised to take total bed rest.
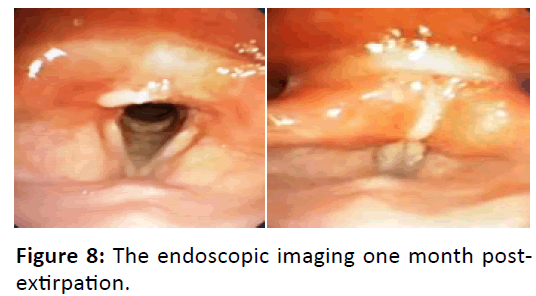
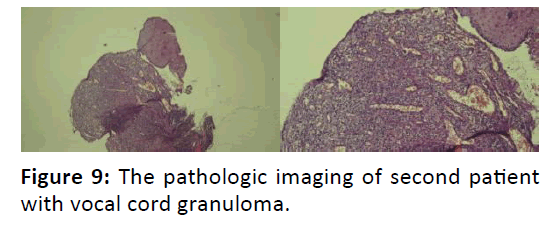
This patient went to the ENT clinic one week later and brought her AP result. The result AP JRS – 16-708 showed: right vocal cord mass: chronic inflammation with granulation. The endoscopic evaluation showed no granuloma, and the larynx was in good condition without oedema or hiperemic. This patient went to the ENT clinic at one month and two months after surgery and the endoscopic results were good, without recurrence of the granuloma (Figures 7-9).
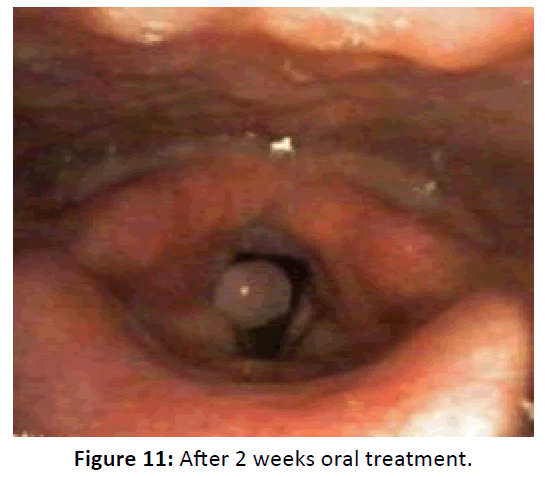
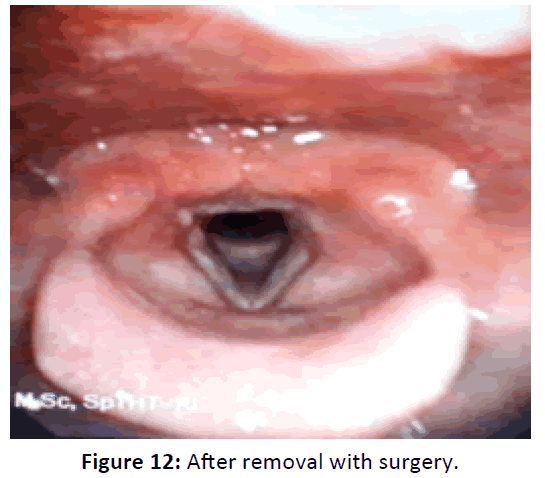
The third case was a 25 years old woman complains of 3 months hoarseness and intermittent aphonia. There is no dyspnea, feeding problem, sore throat, dysphagia or cough. These complaints were present after endotracheal extubation about 3 months ago. The patient has been intubated for 3 days in the ICU before because of pneumonia. There is no history of smoking, voice abuse or gastritis in this patient. Endoscopic examination was done and shows unilateral granuloma. The patient was then given oral anti-inflammatory drugs for 2 weeks without any changes in the size of mass. The granuloma was then removed with micro larynx surgery. Evaluation shows no recurrence of granuloma (Figures 10-12).
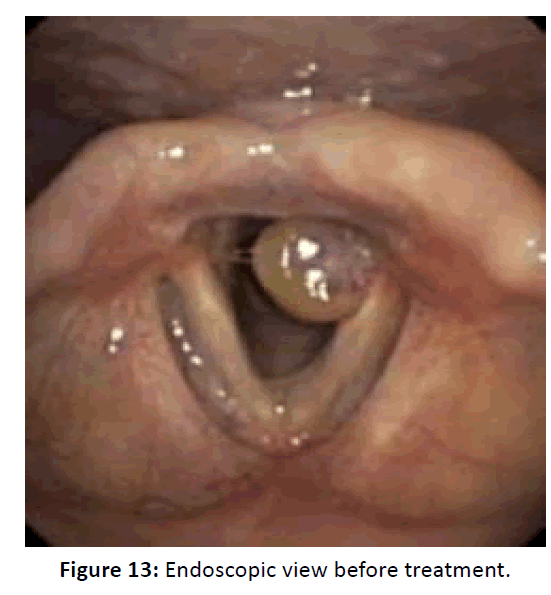
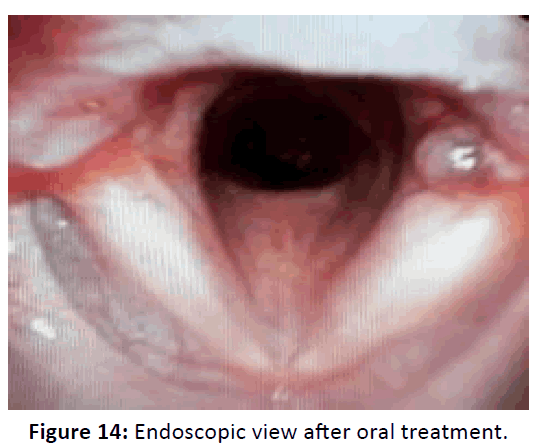
The fourth case, a 24 years old female comes to the outpatient unit with hoarseness since 3 months ago, after the patient was admitted to a hospital because of traffic accidents. Dyspnea was present and persistent since the time of accidents. There are no sore throat, dysphagia, or choking. There was no feeding problem. This patient has a history of prolonged intubation for 2 weeks in the ICU and a Percutaneous Dilatation Tracheostomy was done by the anesthesist. After follow up, it turns out that there was a stenosis in the trachea, and a tracheal stenosis repair by end to end surgery was done by the thoracic surgeon. Endoscopic examination evaluation showed a unilateral mass in the left posterior commissure, patient was managed conservatively, and in 2 weeks follow up the granuloma size has significantly decreased (Figures 13 and 14).
Discussion
The term granuloma in laryngeal granuloma pathologically is not a true granuloma, it is more a reactive reaction against reparation processes, where intact or ulcerative squamous epithelium were covered with fibrotic or granulation tissue. The management of vocal cord granuloma consists of combination between conservative and invasive methods. Conservatively, granuloma can be treated with speech therapy and treatment of the underlying diseases. If the cause that triggers granuloma still exist, the possibility of recurrence is high. Laryngeal granuloma has no malignancy potential5.
The development of laryngeal granuloma can be caused by several factors, ulcerative and contact granulomas have the same pathologic process but with different stages. In some literature, it is called with aritenoid granuloma, vocal cord granuloma, peptic granuloma, pyogenic granuloma, inflammatory polyp, and granulomatous disease of the larynx. It was first reported by Jackson in 1928 as ulcerative contact. Postintubation laryngeal granuloma case was first reported by Clausen in 1932. Contact granuloma more often occurred in male, and postintubation granuloma more often occurred in female. Pediatric patients never acquire contact granuloma, but the case of postintubation granuloma was reported.
The etiology of laryngeal granuloma is still unclear. The point is granuloma develops as an inflammatory reaction in perichondrium area of arytenoids cartilage as a response to mechanical or functional –and sometimes idiopathic— injuries. Mechanical injury can be caused by iatrogenic factors such as: prolonged intubation, incorrect size of endotracheal tube, microlaryngeal surgery, laryngeal laser surgery, and bronchoscopy. Abuse, overuse, and misuse of voice, forced phonation especially inpatient with profession and psychologic characteristics that need excessive use of voice. Risk factors that influence the development of granuloma are heavy cough, vomiting, GERD, habitual throat clearing, alcohol and tobacco use, emotional stress.
The pathogenetic causes include inflammatory response, secondary intention healing process, reparation process of perichondritis, ephitelial hyperplasia, and a possibility of secondary infection. The pathologic processes are the loss of mucoperichondrium in vocal processes of arytenoids. Subepithelial hemorrhage can cause the development of persistent laryngeal granuloma.
The signs and symptoms of granuloma include hoarseness, the sensation of strange body inside the throat, something stuck in the throat, and urge sensation to clearing the throat, pain or blockade inside the throat, difficulty of breathing, and it also could be asymptomatic. The diagnosis is based on history, physical examination, endovideolaryngostroboscopy, voice psychoacoustic analysis, multidimensional computer voice analysis, voice handicap index, reflux symptom index and reflux finding score. Biopsy is needed to define malignancy. The differential diagnoses include specific and non-specific inflammation processes, recurrent laryngeal papilloma, and malignancy.
The main treatments are conservative therapy and intensive voice rehabilitation (vocal and speech therapy, voice rest), inhalation therapy (corticosteroid, panthenol solution, saline), H2 blocker or PPI. Surgical excision is better avoided if granuloma does not narrowing upper airway or it has small size because it tends to reccur. Laser or microlaryngeal surgery could help on cases where granuloma is already narrowing upper airway and threatening respiratory.
Granuloma could be completely removed with conservative therapy using proton-pump inhibitors, vocal and speech therapy, corticosteroid inhalation, or it could be self-limited. In one literature it was said that the adding of zinc in the laryngeal granuloma treatment has quite high successful rate [10].
According to Behm & Brasnu, laryngeal granuloma is the most frequent postintubation complication right after laryngeal oedema. Intubation and extubation procedures still pose risk to cause laryngeal injury. Although these procedures have been closely monitored with cuff pressure and with soft cuff tube, the risk of laryngeal injury is still exist [11]. Trauma of the larynx has been correlated with the duration of intubation and the size of tube used. The injury can manifests as oedema with variable severity, ulceration tissue, and the development of granuloma with potential to obstruct the upper airway.
Granuloma could develop because of multiple intubation or prolonged intubation. In our case, granuloma developed because patient needed to underwent multiple surgeries (overall 9 times surgeries), automatically this patient must underwent multiple intubation, therefore this was in accordance with the data from literature, with possibility that the laryngeal granuloma developed after intubation. This was in accordance with literature because the granuloma had significant size and bilateral position hence it posed an airway obstruction risk and clinically this patient started to complain difficulty of breathing, therefore granuloma extirpation with microlaryngeal surgery was performed. Anesthetic in surgery could be performed with intubation technique using small tube and cuff high volume low pressure [7] or with jet ventilation [12,13]. Some anesthesiologist prefer to use neuroleptic in cases of surgery in laryngeal area to broaden the field visualization and simplified the maneuvers for the surgeon. The postexcisional evaluation of our cases showed clean larynx with no recurrence of granuloma until 4 months postoperatively.
Conservative treatments that can be used for granuloma are as follows:
1. Speech therapy/vocal training
2. Proton Pump Inhibitor (PPI)
3. Anti-inflammatory treatment with NSAID or corticosteroid, topical or sistemic [8]
4. Zinc supplementation (200 mg 3 times a day for adults, and 50 mg for children) [10]
In this patient, we gave antibiotic for infection prophylaxis, corticosteroid for antiinflammation and analgetic. We also gave PPI to prevent the risk of acid reflux from gaster to the laryngeal area.
Conclusions
Vocal cord granuloma is one of possible post intubation complication and it can develop in the case of prolonged intubation, multiple intubation, or short term intubation. This granuloma is developed because of injury of the mucosal or perichondrium area of arytenoids cartilage.
Patients usually came with hoarseness, loss of voice, stuck feeling inside the throat, or difficulty of breathing. The diagnosis was confirmed with direct laryngoscopy or laryngeal endoscopy examinations.
The management vocal fold granuloma includes anti-inflammatory treatment, with NSAID or corticosteroid–local or systemic, PPI, speech therapy and strictly control of risk factors. In the case of unresponsive granuloma with conservative treatment, or a large size granuloma, the presence of difficulty at swallowing or breathing warrant the need to perform the granuloma extirpation surgery with microlaryngeal surgery.
References
- Martins RH, Dias NH, Santos DC, Fabro AT, Braz JR (2009)Clinical, histological and electron microscopic aspects of vocal fold granulomas. Braz J Otorhinolaryngol 75: 116-122.
- Rosen CA, Simpson CB (2008) Operative techniques in laryngology. Springer Science & Business Media.
- Russell C, Matta B (2004) Tracheostomy a multiprofessional handbook. Cambridge university press.
- Lemos EM, Sennes LU, Imamura R, Tsuji DH (2005) Vocal process granuloma: Clinical characterization, treatment and evolution. Rev Bras Otorrinolaringol 71: 494-498.
- Wang H, Chen M, Chao P (2014) Bilateral large postintubation vocal granulomas. J Exp Clin Med 6: 29-30.
- Benjamin B, Lauren D (2008) Laryngeal complications of endotracheal intubation. Annals of Otology, Rhinology & Laryngology 117: 2-20.
- Patil PG, Jain R, Chaudhuri SM, Thakkar JM, Patel BM (2012) Case report tracheal granuloma as an incidental finding during endotracheal intubation. Gujarat Med J 67: 123-125.
- Yokoi A, Nakao M, Bitoh Y, Arai H, Oshima Y, et al. (2014) Treatment of postoperative tracheal granulation tissue with inhaled budesonide in congenital tracheal stenosis. J Pediatr Surg 49: 293-295.
- Santosh D, Lailyang T, Gautamjit RK, Kanato A, Savanna M (2015) Post-intubation vocal fold granuloma in a case of twin pregnancy with disseminated intravascular coagulopathy :A case report. J Dent Med Sci 14: 3-5.
- Djukić V, Krejović-Trivić S, Vukašinović M, Trivić A, Pavlović B, et al. (2015) Laryngeal granuloma-Benefit in treatment with zinc supplementation? J Med Biochem 34: 228-232.
- Tadié JM, Behm E, Lecuyer L, Benhmamed R, Hans S (2010) Post-intubation laryngeal injuries and extubation failure: A fiberoptic endoscopic study. Intensive Care Med 36: 991-998
- Altun D, Yılmaz E, Başaran B, Çamcı E (2014) Surgical excision of postintubation granuloma under jet ventilation. Turk J Anaesthesiol Reanim 42: 220-222.
- Nakahira J, Sawai T, Matsunami S, Minami T (2014) Worst-case scenario intubation of laryngeal granuloma: A case report. BMC Res Notes 7: 74.