Research Article - Otolaryngology Online Journal (2019) Volume 9, Issue 1
Patient Characteristics and Outcomes Following Conventional Small Fenestra Stapedectomy: A Retrospective Analysis
Verma N* and Dubey KKDepartment of ENT, Melaka Manipal Medical College (MAHE), Melaka, Malaysia
- *Corresponding Author:
- Nishikanta Verma
Department of ENT
Melaka Manipal Medical College (MAHE)
Melaka, Malaysia
Tel: 0060126507859
E-mail: drverman@gmail.com
Received date: November 23, 2018; Accepted date: January 04, 2019; Published date: January 11, 2019
Copyright: © 2019 Verma N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
The current study was undertaken to evaluate the results of stapedotomy over a three-year period at a tertiary hospital. We studied the case records, including demographic data and operative results, of patients with clinically suspected otosclerosis undergoing stapedotomy. Over a 3-year period, a total of 264 patients underwent small fenestra stapedectomy of which records were complete for 200 patients and were thus included for analysis. The procedure was done under local anaesthesia and used a 0.6 mm Teflon piston with sacrifice of the stapedius tendon. Air-Bone Gaps at speech frequencies of 500 Hz to 3 KhZ were averaged to calculate the Pure-Tone averages. This was done following the recommendations of the AAO-HNS and was done pre-operatively and post-operatively. 92/200 patients were male (46%) and 108/200 (54%) were female with an age range of 20-50 and a mean of 32 ± 7.78 years. The mean pre-operative Air-Bone gap was 46.1 ± 8.23. No patient had abnormal BC thresholds. After surgery, the mean air-bone gaps at 30 days, 90 days and 180 days were 28.84 ± 6.74, 18.32 ± 6.53 and 9.26 ± 4.49 dB. At six months’ follow-up, all patients had achieved Air-Bone Gap closure to within 25 dB while 104 patients (52%) had achieved closure to within 10 dB. While the study is retrospective in nature, our results reflect current thought that small fenestrastapedectomy remains an excellent surgical option in experienced hands for patients with otosclerosis.
Keywords
Otosclerosis; Air bone gap; Stapedectomy
Introduction
Otosclerosis is an autosomal dominant primary metabolic bone disease resulting in the fixation of the footplate of the stapes. The inability of the footplate to vibrate optimally results in conductive hearing loss, which is the usual presenting symptom. The penetrance of the gene is incomplete and the triggering mechanisms for its expression remain incompletely understood. Hearing may be rehabilitated either by hearing aids or by surgery, which in experienced hands has shown good and immediate results [1,2].
The modern history of stapes surgery begins with John Shea Jr. After numerous attempts to mobilize the stapes or fenestrate the semicircular canals resulted in suboptimal results and complications, he decided to bypass the diseased stapes footplate by inserting an artificial piston. The original piston was made of Teflon. This was used with success for the first time in 1956. Soon thereafter, Shea promoted the total removal of the footplate of the stapes and used a vein graft as a seal. This operation was called “stapedectomy” [3].
In 1962, advances in technique resulted in the modification of the original procedure. It was found that precision fenestration of the footplate for piston insertion decreased the risk of perilymph leak. This started the era of “stapedotomy”. Since then, numerous modifications to the original technique have been studied and recently, lasers have been used to cut the stapedius tendon or to make the stapes footplate opening more precise [4,5].
The present study was undertaken to review the results of consecutive stapedotomies over a threeyear period.
Patients and Methods
Consecutive patients undergoing stapedotomies over a three-year period were included in the analysis. A total of 264 patients were operated in this period. However, complete case records were only available for 200 patients and hence only this number was taken for final analysis. We recorded the age, gender, mean pre-operative Air Bone Gaps and the mean post-operative Air Bone Gaps. The Air-Bone gaps were studied at the speech frequencies (500 kHz to 3 kHz) as recommended as the speech frequencies by the AAO-HNS. Air Bone Gaps were calculated by subtracting AC thresholds from pre-operative BC thresholds [6,7].
In all cases, patients were admitted overnight. A stapedotomy was performed under local anaesthesia. A 0.6 mm Teflon piston was used for all cases. Patients were followed up at one month, three months and six months.
Results and Discussion
In our study, 92 patients were male (46%) and 108 women (54%). These figures do not convey a gender predilection for otosclerosis as has been suggested by Glasscock and Shambaugh. The cohort of Grolman et al. also had more female patients. However, in recent studies, no gender difference was reported [8-10].
The mean age at presentation was 32 ± 7.78 years with a range from 20-50 years. No patient had abnormal bone conduction thresholds at presentation. Niedermeyer et al. Studied 1351 patients who had undergone stapes surgery and concluded that the average age at presentation had increased over the years. In their cohort, the mean age at presentation in 1978 was 39.60 ± 10.83 years while by 1999 it had increased to 43.57 ± 12.5 years. The authors of this study hypothesized that younger patients may have been less attentive to hearing issues, thus presenting later, or that younger patients may have already undergone surgery as a result of increased health awareness. The introduction of the anti-measles MeV vaccine in Germany, where this study was conducted, may have also played a role as the measles virus is implicated in expression of the otosclerotic gene [11,12]. The mean age in our study is slightly lower than in the Niedermeyer study, perhaps reflecting that our cohort, which was mainly derived from a lower-socioeconomic stratum, may not have been vaccinated against measles in childhood or found that hearing loss was a significant disabling factor in daily activities necessitating a hospital consultation.
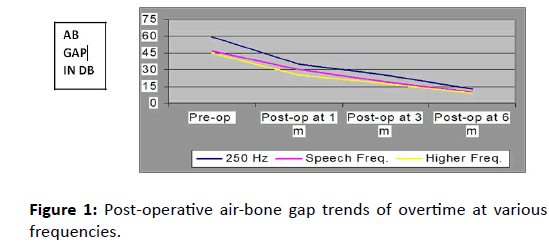
The mean pre-operative Air-Bone Gap in the speech frequencies averaged 46.1 ± 8.23 dB. No patient had abnormal BC thresholds. After surgery, the mean Air-Bone Gaps at 1 month, 3 months and 6 months were 28.84 ± 6.74, 18.32 ± 6.53 and 9.26 ± 4.49 dB reflecting improving hearing. At six months’ followup, all patients had achieved Air-Bone Gap closure to within 25 dB while 104 patients (52%) achieved closure to within 10 dB.
No patient had sensori-neural hearing loss though six patients reported temporary facial nerve paresis which had recovered by the time they were discharged. This was possibly an effect of the local anaesthetic used for surgery on a dehiscent facial canal though the latter finding was not recorded in the operative notes. The average operating time was 22 minutes. These results are summarized in the following Tables 1, 2 and Figure 1.
| Age | Male | Female | Total |
|---|---|---|---|
| 20-24 | 12 | 24 | 36 |
| 25-29 | 8 | 16 | 24 |
| 30-34 | 36 | 48 | 84 |
| 35-39 | 12 | 0 | 12 |
| 40-44 | 4 | 16 | 20 |
| 45-50 | 20 | 4 | 24 |
Table 1: Age and gender distribution.
| Age | Mean A-B Gap |
|---|---|
| 20-24 y | 47.48 ± 4.83 |
| 25-29 y | 49.17 ± 4.45 |
| 30-34 y | 42.74 ± 9.06 |
| 35-39 y | 49.58 ± 5.20 |
| 40-44 y | 52.50 ± 8.29 |
| >45 y | 49.79 ± 9.27 |
Table 2: Pre-operative air-bone gaps at speech frequencies.
Stapedotomy, or small fenestra stapes surgery is a valuable tool for improving hearing and our results reflect that it should be preferred over stapedectomy where possible. This is borne out by numerous previous studies such as Portmann and Aramann-Tucoo [13]. In their study, 622 patients who underwent either stapedectomy or stapedotomy were evaluated at least five years after surgery. The authors observed that while Air-Bone Gap closure was better with stapedectomy at one month, the incidence of overclosure was comparable between the two procedures. Significantly, the authors noted that as time passed, the Air-Bone Gap increased after stapedectomy while it decreased after stapedotomy. This is in line with our results which also show a narrowing of the A-B Gap over time, though in our case, the follow-up is only six months. We did not have any incidence of overclosure in our study.
Spandow et al. has evaluated 60 consecutive patients who underwent stapes surgery. They found that while stapedectomy and stapedotomy had comparable results in the lower frequency ranges, stapedotomy fared considerably better in the 4-6 KhZ range [14].
Persson et al. has analyzed the long-term results of stapes surgery in a sample of 437 operated ears. Patients underwent either partial stapedectomy (16%) or total stapedectomy (47%) or stapedotomy (37%). The authors found that while stapedectomy (total and partial) offered better hearing gains in the first three years, there was a decline in hearing with these procedures which was faster than with stapedotomy. This suggested a sensor neural cause for post-operative hearing loss which was not the case with stapedotomy. Thus stapedotomy seemed to be a more reliable choice of procedure. Dornhoffer et al. has stated that stapedotomy causes less post-operative vertigo and also results in better hearing, especially at slightly higher frequencies. This has been borne out by multiple studies which endorse the efficacy and safety of stapedotomy [15-19].
Conclusion
Conventional stapedotomy remains a safe and effective procedure for otosclerosis. This is especially valuable to know in centers where lasers are unavailable. The absence of advanced equipment should not be a deterrent to surgery.
Funding
This research did not benefit from any funding grants by any agencies.
Conflicts of interest
None
References
- Velegrakis GA. Otosclerosis: State of the art. Otorhinolaryngologia Head Neck Surg. 2011;43:6-16.
- Khan H, Shah JI, Saeedullah, et al. Small fenestra stapedotomy. JPMI. 18:176-81
- Shea JJ Jr. A personal history of stapedectomy. Am J Otol. 1998;19:S2-12.
- Lesinski SG. Lasers for otosclerosis-which one and why. Lasers Surg Med. 1990;10: 448-57
- Vernick DM. Comparison of the results of KTP and CO2 laser stapedotomy, Am J Otology. 1996;17: 221-24.
- Monsell EM, Balkany TA, Gates GA, et al. Committee on hearing and equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol Head Neck Surg. 1995;113:186-87.
- Laitakari K, Laitakari E. From posterior crus stapedectomy to 0.6 mm stapedotomy-towards reliability in otosclerosis surgery. Acta Otolarygologica. 1997;50-2.
- Glassock ME, Shambaugh GE Jr.,(Ed.) Surgery of the Ear, 5th edition. 1990 W.B. Saunders, Philadelphia.
- Grolman W, Tange RA, Debruijn AJ, et al. A retrospective study of the hearing results obtained after stapedotomy by the implantation of two Teflon pistons with a different diameter. Eur Arch Otorhinolaryngol. 1997;254:422-24.
- Niedermeyer HP, Häusler R, Schwub D, et al. Evidence of increased average age of patients with otosclerosis. Adv Otorhinolaryngol. 2007;65:17-24.
- Arnold W, Friedman I. Otosclerosis-an inflammatory disease of the otic capsule of viral aetiology. J Laryngol Otol. 1988;102:865-71.
- Lolov SR, Encheva VI, et al. Antimeasles immunoglobulin G in sera of patients with otosclerosis is lower than that in healthy people. Otol Neurotol. 2001;22:766-70.
- Portmann D, Aramann tuccoo JF. Stapedectomy and microstapedectomy in the treatment of otospongiosis. A comparative study. Rev Laryngol Otol Rhinol. 1989;110: 317-22.
- Spandow O, Soderberg O, Bohlin L. Long-term results in otosclerotic patients operated by stapedectomy or stapedotomy. Scand Audiol. 2000;29:186-90.
- Persson P, Harder H, Magnusson B. Hearing results in otosclerosis surgery after partial stapedectomy, total stapedectomy and stapedotomy. Acta Otolaryngol. 1997;117:94-99.
- Dornhoffer JL, Bailey HA, Graham PS. Long-term hearing results following stapedectomy. Am J Otol. 1994;15: 674-78.
- Adedeji TO, Indorewala S, Indorewala A, et al. Stapedotomy and its effect on hearing - our experience with 54 cases. Afr Health Sci. 2016;16:276-81.
- Murfee J, O'Connell B, Haynes D, et al. Outcomes of Stapedotomy with heat-crimped prostheses. Otol Neurotol. 2018;39:1235-1240.
- Cheng HCS, Agrawal SK, Parnes LS. Stapedectomy Versus Stapedotomy. Otolaryngol Clin North Am. 2018;51:375-92.