Research Article - Otolaryngology Online Journal (2016) Volume 6, Issue 2
Epidemiology of Otorhinolaryngology Diseases Seen in Health Camps in Rural Backward Areas of Himachal Pradesh
- *Corresponding Author:
- Manpreet Singh Nanda
Department of Otolaryngology, Maharishi Markandeshwar Medical College & Hospital, Kumarahatti, India
E-mail: u_tell_me_80@yahoo.co.inia
Received: March 06, 2016; Accepted: March 20, 2016; Published: March 23, 2016
Introduction
Himachal Pradesh is a hilly state in northern part of India. Sirmour and some parts of Solan district are amongst the most backward areas of the state. Health care facilities are not easily available in rural areas. In rural areas still untrained and unskilled practitioners attend the patients [1].
Otorhinolaryngology (ENT) diseases are common in rural community and early diagnosis and management will result in reduction of morbidity [2]. But in these areas doctors especially ENT specialists are not easily available and those available don’t have enough training and knowledge. Most of the ENT problems are managed by home remedies and most individuals manage their problems in the community without any help. Ignorance, poverty and traditional beliefs prevent the rural population from attending hospitals in cities [3].
There are just a few studies in literature describing the epidemiology in ENT care [4]. There is not much data available on the prevalence of ENT diseases in rural communities in India. A proper understanding of magnitude of ENT diseases and factors associated with their occurrence in the rural population is important to enable formulation of health care service aimed at early detection and treatment of morbidity. This study aims to determine the pattern of ENT diseases in the rural backward areas of this region and find ways to deal with them and help to develop programmes in rural areas relating to ENT diseases.
Materials and Methods
This is a prospective study among the patients attending the health camps in the rural backward areas of Solan and Sirmour districts in Himachal Pradesh conducted by our institute Maharishi Markandeshwar Medical College and Hospital over a period of two years between December 2012 and November 2014. All the patients presenting in the camps with ENT complaints were included in this study after taking written consent from them and were examined by the specialist. The patients were examined using head light, otoscope, nasal and aural speculums, tongue depressors, nasal and aural forceps and tuning forks for tuning fork tests. These equipments were made available at the camps. The approval of local ethics committee was taken. All the camps were free health camps. No money was charged for health check up, even medicines were distributed free of cost. The diseases were divided into three groups – Otology (Ear) diseases, Rhinology (Nose) diseases, Laryngology (Throat) diseases. A diagnosis was made by careful history taking and clinical examination. Details were recorded and data was analysed statistically.
The following data was extracted and analysed by simple descriptive methods
1) Total number of patients attending the camps and percentage of ENT cases among them.
2) Age and Sex distribution of patients with ENT complaints.
3) Pattern of distribution of diseases among Ear, Nose and Throat.
4) Incidence of various ENT diseases in paediatric and adult age groups.
5) The patients were enquired about any previous treatment taken.
6) Availability of ENT specialists or graduate doctors was enquired about in the villages where the camps were held.
Results
20 free health camps were held in rural areas of Solan and Sirmour district from December 2012 to November 2014. Out of the total 6404 patients in these health camps, 690 patients of ENT complaints were examined by the authors. This shows that ENT cases constitute nearly 11% of the total patients presenting in rural areas (Table 1).
| S.NO | Camp Location | Date of | Total | ENT Cases | Percentage of ENT Cases |
|---|---|---|---|---|---|
| camp | Patients | ||||
| 1 | Bhojnagar | 9-12-2012 | 305 | 36 | 11.8% |
| 2 | Subathu | 30-12-2012 | 371 | 41 | 11.1% |
| 3 | Nauni | 6-1-2013 | 250 | 30 | 12% |
| 4 | Dharampur | 20-1-2013 | 410 | 46 | 11.1% |
| 5 | Jabli | 17-2-2013 | 315 | 32 | 10.1% |
| 6 | Sarhan | 3-3-2013 | 507 | 48 | 9.6% |
| 7 | ManngiShilly | 17-3-2013 | 280 | 30 | 10.8% |
| 8 | Gaura(Giripul) | 24-3-2013 | 215 | 28 | 13.1% |
| 9 | Rajgarh | 7-4-2013 | 318 | 30 | 9.5% |
| 10 | Deothi | 21-4-2013 | 290 | 32 | 11% |
| 11 | Narag | 19-5-2013 | 255 | 28 | 11% |
| 12 | Nainatikkar | 22-9-2013 | 270 | 29 | 10.8% |
| 13 | Kunehar | 29-9-2013 | 328 | 35 | 10.7% |
| 14 | Garkhal | 24-11-2013 | 248 | 25 | 10% |
| 15 | Chambaghat | 9-3-2014 | 370 | 34 | 9.2% |
| 16 | Basal | 26-3-2014 | 275 | 30 | 10.9% |
| 17 | Jadhana | 24-8-2014 | 308 | 35 | 11.4% |
| 18 | Salogra | 28-9-2014 | 204 | 28 | 13.7% |
| 19 | Badhalag | 12-10-2014 | 480 | 52 | 10.8% |
| 20 | Dholkajubber | 19-10-2014 | 405 | 41 | 10.1% |
| Total | 6404 | 690 | 10.7% |
Table 1: Camp location, date, total number of patients out of which number and percentage of ENT cases examined.
The maximum percentage of ENT cases were seen at camp at Salogra (13.7%) and minimum at Chambaghat (9.2%). This shows a significant higher prevalence of ENT diseases in rural population.
Regarding the age distribution, nearly 35% ENT patients (238 out of 690) were in the paediatric age group. 30% were of younger age group (19 – 40 years), 20% were of middle age group and remaining 15% of older age group. This shows thar the paediatric population constitutes a major percentage of ENT cases in rural areas (Table 2). Regarding sex distribution, in paediatric patients male and female ratio was almost equal, but in adults more male patients attended the camps as compared to females (3:2) (Table 2).
| Age Group (in years) | Male | Female | Total |
|---|---|---|---|
| 0 - 18 | 118 | 120 | 238 |
| 19 - 40 | 125 | 85 | 210 |
| 41 - 60 | 88 | 53 | 141 |
| 61 and above | 61 | 40 | 101 |
| Total | 392 | 298 | 690 |
Table 2: Age and Sex distribution.
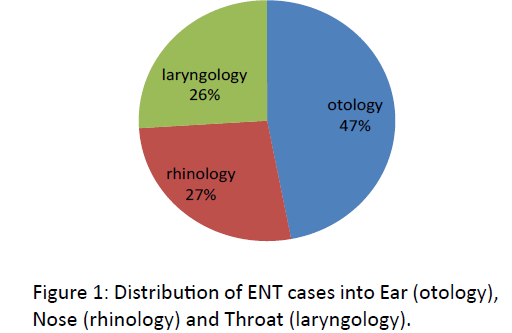
Regarding patients in each sub group of ENT, nearly half of the patients were of Ear diseases (otology). The patients of Nose diseases (rhinology) and Throat diseases (laryngology) were almost equal (Figure 1).
In the paediatric age group (upto 18 years of age), there were total of 238 patients, that constitute around 35% of total ENT patients. Out of which majority were otology cases. Ear wax was the most condition found out in paediatric age group (65 patients), followed closely by ASOM (Acute Suppurative Otitis Media) where children presented with pain in the ears and discharge. The other common otological diseases were CSOM (Chronic Suppurative Otitis Media) and Otitis Externa. Two patients with foreign body in ear and one with congenital deafness also present in the camp. Among the Nose cases, Rhinitis was the most common disease. 6 children with Epistaxis presented in these camps. There were 5 patients with vestibulitis of nose and 1 patient with foreign body nose which was removed. Among the Throat cases, the majority 37 cases were of Tonsillitis and 18 cases of pharyngitis. There were two children with speech disorders and one with tongue tie which were referred to our medical college and hospital for further treatment (Table 3).
| Disorders | Diseases | Patients | Percentage |
|---|---|---|---|
| Ear (Otology) | Ear Wax | 65 | 27.4% |
| ASOM | 45 | 19% | |
| CSOM | 24 | 10% | |
| Otitis Externa | 11 | 4.6% | |
| Others | 3 | 1.3% | |
| Nose (Rhinology) | Rhinitis | 20 | 8.3% |
| Epistaxis | 6 | 2.6% | |
| Vestibulitis | 5 | 2.1% | |
| Others | 1 | 0.4% | |
| Throat (Laryngology) | Tonsillitis | 37 | 15.5% |
| Pharyngitis | 18 | 7.5% | |
| Others | 3 | 1.3% | |
| Total | 238 | 100% |
Table 3: Distribution of Ear, Nose and Throat diseases in paediatric age group.
These results of paediatric ENT patients show the high prevalence of otological problems among rural children.
Among the adult patients (greater than 18 years of age), the distribution among Ear, Nose and Throat cases was more even with Otology diseases being the highest. Among the otology diseases, CSOM was the most common disease (56 patients) followed by Otitis Externa. There were 35 patients with ear wax, 28 patients with Presbyacusis (mostly were of older age group). In the older age group (more than 60 years of age), (Table 4) Presbyacusis was the most common disease. 8 patients presented with ASOM in adults. There were 5 patients with Tinnitus as their major complaint (Table 4). There were 2 patients with foreign body ear which was removed and 2 patients with unilateral sensori-neural hearing loss.
| Disorders | Diseases | Patients | Percentage |
|---|---|---|---|
| Ear (Otology) | CSOM | 56 | 12.4% |
| Otitis Externa | 40 | 8.8% | |
| Ear Wax | 35 | 7.7% | |
| Presbyacusis ASOM Tinnitus |
28 8 5 |
6.2% 1.8% 1.1% |
|
| Others | 4 | 0.9% | |
| Nose (Rhinology) | DNS | 54 | 11.9% |
| Allergic Rhinitis | 52 | 11.5% | |
| Rhinosinusitis Vestibulitis Nasal Polyposis |
25 10 9 |
5.5% 2.3% 2% |
|
| Others | 4 | 0.9% | |
| Throat (Laryngology) | GERD | 48 | 10.6% |
| Pharyngitis Tonsillitis Apthous Ulcers Laryngitis |
37 20 7 7 |
8.3% 4.5% 1.5% 1.5% |
|
| Others | 3 | 0.6% | |
| Total | 452 | 100% |
Table 4: Distribution of Ear, Nose and Throat diseases in adults.
Among the rhinology cases, the most common was Symptomatic Deviated Nasal Septum (DNS). There were 54 such adults presenting with nasal obstruction as their chief complaint. There were 52 patients with Allergic Rhinitis who presented as sneezing, itching over nose and eyes and watering of the eyes as their main complaints. 25 patients were clinically identified as Rhinosinusitis. 9 Patients had polypoidal mass in their nose. All of these patients were referred to our medical college and hospital for further evaluation. There were 10 patients with vestibultis, 2 with epistaxis, 1 case of nasal malignant growth and 1 patient diagnosed as atrophic rhinitis (Table 4).
Gastro Esophageal Reflux Disease (GERD) was one of the most common diseases in adults (48 patients) with its incidence higher in middle and older age groups. There were significant number of patients with pharyngitis (27 patients) and tonsillitis (20 patients). Tonsillitis patients were mainly of younger age group. There were 7 patients of oral apthous ulcers. 7 patients had chronic laryngitis. 2 patients presented with neck masses, these patients were referred to our medical college and hospital for further evaluation. 1 patient presented with ulcerative growth in buccal mucosa, who was further evaluated in our medical college and hospital (Table 4).
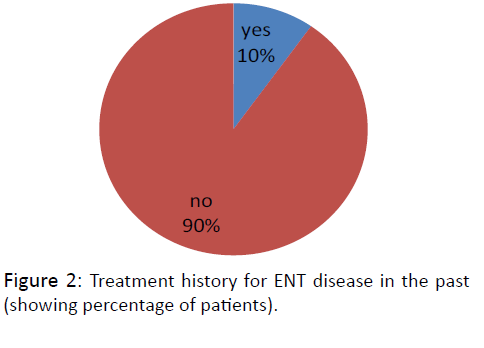
On being questioned about any previous treatment taken for the same in the past, it was found that only 68 out of total 690 rural population with ENT diseases had taken any treatment in the past. This constitutes just nearly 10% of total patients. This finding shows lack of treatment for NT diseases at the rural level (Figure 2).
Regarding availability of doctors in the villages, none of the 20 village panchayats had an ENT specialist. Only 10 village panchayats had a graduate doctor available in their areas. Remaining 10 village panchayats had no medical specialist available and had a travel a lot to avail such facility. In many of these villages rarely any transport facility was available.
Discussion
This study was done to determine the pattern of ENT diseases in the rural backward areas of this region and find ways to deal with them. Our institute MMMC&H had organized these free health camps to involve those people residing in rural backwards who had rarely ever visited a hospital because of poverty, lack of facilities and ignorance but attended these camps as they were held in their village panchayats itself and that the camps didn’t charge any money for health checkup and even medicines were distributed free of cost. The patient number in these camps on an average was on lower side between 200 to 500 but was significant considering the sparsely populated hilly terrains where these camps were organized (Table 1). The ENT cases in these camps varied between 30 to 50, thus constituting a significant 10 – 11% of total patients (Table 1). This is a significant percentage of population thus calling for a need to establish a well up to date ENT practice in terms of equipment and manpower training in order to meet the various aspects of management of these patients including their rehabilitation. Children constituted a major part of ENT patients (Table 2) in our study. There was a male predominance in adult patients (3:2) (Table 2) which could be attributed to social and family reasons leading to lesser number of women attending the camps.
Wide varieties of ear, nose and throat diseases present to otorhinolaryngologist [5]. Many of these diseases could be managed at the level of primary health care6. Health care facilities are easily available in urban areas but not in semi urban and rural areas. And in these areas doctors especially ENT specialists are not easily available and those available don’t have enough training and knowledge. In our study also we found that out of 20 village panchayats we visited, none of them had an ENT specialist and only 50% of them had a doctor available in their areas. Only 10% of the ENT patients had taken any treatment for their ailments in the past (Figure 2). Similar results were seen in other studies available in the literature [7].
Hearing loss is a significant health problem in a developing country [8]. CSOM is one of the most common cause of permanent hearing loss [9].It is most common ear disease10. In our study otological problems were the major burden as reported by WHO [11]. We found in our study that ear diseases constitute 47% of total ENT diseases (Figure 1). Similar results were obtained in other studies done in Enugu (54%) [12] and in Nepal (57.8%) [13]. In our study we found CSOM to the most common ENT disease in adults (12.4%) (Table 4). Similar results were obtained in other studies available in literature [12-14]. Other common ear diseases in adults in our study were otitis externa (8.8%) and ear wax (7.7%) (Table 4). J Hatcher et al also found CSOM and wax to be a major form of ear disease [15]. Otitis media as a result of infection has been more common among rural population as compared to urban population [14]. Poor living conditions, overcrowding, poor hygiene and poor nutrition could be one of the major cause.
In paediatric population, ear wax (27.4%) and otitis media (ASOM and CSOM) constituted major ENT diseases prevalent in our study. The incidence of Otitis Externa was also found to be significant in children in our study (Table 3). Various other studies have looked at the prevalence of ENT diseases among children [16] and have shown that the disease burden is due to Otitis Media which is the most common medical problem of childhood and a common cause of preventable hearing loss in children in developing countries [17], making it one of the most frequent morbidity encountered in day to day clinical practice. Prakash Adhikari in 2009 found wax followed by CSOM to be most common ear disease in children in rural areas [18]. A lot of people especially children have the habit of scratching their ears leading to Otitis Externa. It is a known preventable disease and constitute important health problem among children [19].
Presbyacusis is the most cause of hearing loss in older age group in our study. Similar results were obtained in the literature available. Thus otological problems are the major part of ENT diseases in rural population and leads to hearing loss. So there is an urgent and aggressive need to find a solution to this problem especially in rural and backward areas of the country. The Government of India initiative of National Programme for Prevention and Control of Deafness is a right step in this direction which needs to be implemented in a proper way with the help of otorhinolaryngology community in India.
Symptomatic DNS and Allergic Rhinitis were the major nasal diseases in the adults in our study. This goes along with other studies available in literature. Allergic Rhinitis is associated with significant co morbidities and health care costs [20]. The other nasal diseases commonly seen were rhinosinusitis, vestibulitis and nasal polyposis (Table 4). In children we found rhinitis to be the most common nasal disease, followed by epistaxis and vestibulitis (Table 3).
Among throat diseases, we found GERD to be the most common disease in adults (Table 4). It was more common in middle and older age groups. In a study by Rokonuzzaman SM et al. 87.75% individuals in rural areas had GERD [21]. Its higher occurance in our region can be attributed to eating habits of the people who prefer more spicy food. Other throat diseases common in adults were pharyngitis, tonsillitis and laryngitis. Tonsillitis was more common in younger age group. Oral aphthous ulcers also constituted 1.5% of total adult patients in our study. (Table 4) The cause of oral mucosal ulcers is due to temporary weakness in immune system, low levels of vitamin B12, folate, iron, ferritin [22].
In the paediatric age group, Tonsillitis was the most common throat disease in our study (Table 3). This confirms to reports of studies which have shown recurrent tonsillitis in 11.7% of Norway children in one study and to effect 12.1% of Turkey children in another study [23]. In our study we found 15.5% of rural children suffering from tonsillitis (Table 3). Upper respiratory tract infection is a cause of complaints like otitis media and tonsillitis in children [24].
These results clearly shows the wide prevalence of otorhinolaryngology diseases in rural backward areas and the urgent need to establish better healthcare especially ENT services for the rural population of our country.
Conclusion
There is wide prevalence of Ear, Nose and Throat diseases in rural backward areas and a severe lack of treatment facilities in these areas. Ignorance, poverty and traditional beliefs prevent rural population from taking proper treatment in city hospitals. The most common ENT diseases in adults in rural areas in our study were CSOM, DNS, Allergic Rhinitis, GERD and Otitis External whereas in paediatric age group were Ear Wax, ASOM, Tonsillitis and CSOM. Otology diseases were more common in both adults and paediatric age group.
This model of ENT health care of screening and treating patients in the health camps is effective and helps in alleviating the disease burden in rural areas. The need for the hour is to
- To create awareness of common ENT problems among rural masses and the treatment options available.
- To establish ENT care in rural and backward areas in terms of both equipment and manpower.
- Higher degree of exposure to ENT surgeons to various surgeries to have a successful outcome and treatment. This can be done by organizing more workshops and conferences in reputed centres.
- To establish National Health Programmes covering ENT diseases to provide treatment to our citizens residing in rural and backward areas. National Programme for Prevention and Control of Deafness is a right step in this direction but it needs to be implemented in a proper way with active participation of senior ENT faculty.
- We recommend frequent and more such health camps in rural areas of India to screen and treat patients with otorhinolaryngology diseases.
Acknowledgements
We would like to thank our institute Maharishi Markandeshwar Medical College and Hospital for its support and the patients for cooperating with the study protocol.
References
- Akinpelu OV, Amusa YB, Komolafe EO, Adeolu AA, Oladele AO, Ameve SA (2008) Challenges in management of chronic suppurative otitis media in a developing country. J LaryngolOtol 122: 16-20.
- Bhattia PL, Varughese R (1987) Pattern of otorhinolaryngological diseases in Jos community. Nig Med J 17: 67-73.
- Fasunla AJ, Lasisi OA (2007) Sinonasal Malignancies: A 10-year review in a Tertiary Health Institution. J Natl Med Assoc 99: 1407-1410.
- Zakzouk SM, Jamal TS, Daghistani KJ (2002) Epidemiology of acute otitis media among Saudi children. International Journal of Pediatric Otorhinolaryngology 62: 219-222.
- Ibekwe TS, Nwaorgu OGB, Onakoya PA, Ibekwe PU (2005) Spectrum of Otorhinolaryngological emergencies in elderly in Ibadan, Nigeria. Nig J Med 14: 411-414.
- Kishve SP, Kumar N, Kishve PS, Aarif SMM, Kalakoti P (2010) Ear, nose and throat disorders in paediatric patients at a rural hospital in India. Australasian Medical Journal 12: 786-790.
- Rourke T, Tassone P, Philpott C, Bath A (2009) ENT cases seen at a local 'walk-in centre': a one year review. J LaryngolOtol 123:339-342.
- Olusanya BO, Okolo AA, Aderemi AA (2004) Predictors of hearing loss in school entrants in a developing country. J Postgrad Med 50: 173-178.
- Biswas AC, Joarder AH, Siddiquee BH (2005) Prevalence of CSOM among rural school going children. Mymensingh Med J 14: 152-155.
- Okafor B.C (1984) The chronic discharging ear in Nigeria. J LaryngolOtol 98: 113-119.
- (2004) “Child and Adolescent Health and Development Prevention of Blindness and Deafness.” World Health Organization, Geneva, Switzerland.
- Okafor BC (1983) Otolaryngology in South Eastern Nigeria: pattern of diseases of the ear. Niger. Med. J 13: 11-19.
- Sigdel B, Nepali R (2012) Pattern of ear disease among paediatric ENT patients: An experience from Tertiary care centre, Pokhara, Nepal. J NepalPaediatrSoc 32: 142-145.
- Jacob A, Rupa V, Job A, Joseph A (1997) Hearing impairment and otitis media in a rural primary school in South India. IntJ PediatrOtorhinolaryngol 39: 133-138.
- Hatcher J, Smith A, Mackenzie I et al (1995) A prevalence study of ear problems in school children in Kiambu district, Kenya, 1992. IntJ PediatrOtorhinolaryngol 33: 197-205.
- Maharjan M, Bhandari S, Singh I, Mishra SC (2006) Prevalence of otitis media in school going children in Eastern Nepal. Kathmandu University Medical Journal 16: 479-482.
- Ologe FE, Nwawolo CC (2002) Prevalence of chronic suppurative otitis media (CSOM) among school children in a rural community in Nigeria. Nigeria Postgrad Med J 9: 63-66.
- Adhikari P (2009) Pattern of ear diseases in rural school children: Experiences of free health camps in Nepal. Int J PediatrOtorhinolaryngol 73: 1278-1280.
- Rao RS, Subramanyam MA, Nair MS, Rajashekar B (2002) Hearing impairment and ear diseases among children of school entry age in rural South India. Int J Pediatric Otorhinolaryngol 64: 105-110.
- Malone DC, Lawson KA, Smith DH, Arrighi HM, Battista C (1997) A cost of illness study of allergic rhinitis in the United States. Journal of Allergy and Clinical Immunology 99: 22-27.
- Rokonuzzaman SM, Bhuian MR (2011) Epidemiologic study of gastro esophageal disease in rural population. Mymensingh Med J 20:463-471.
- Greenberg MS, Pinto A (2003) Etiology and management of recurrent aphthous stomatitis. Current Infectious Disease Reports 5: 194-198.
- Kvestad E, Kvaerner KJ, Roysamb E, Tambs K, Harris JR, Magnus P (2005) Heritability of recurrent tonsillitis. Arch Otolaryngol Head Neck Surg 131: 383-387.
- Kari J Kværner, Per Nafstad, Jouni JK Jaakkola (2000) Upper Respiratory Morbidity in Preschool Children ACrosssectional study. Arch Otolaryngol Head Neck Surg 126:1201-1206.